
Performance of the EuroSCORE II and the Society of Thoracic Surgeons score in patients undergoing aortic valve replacement for aortic stenosis
Introduction
The heart valve surgery is often the only way to improve the long-term survival of a patient with severe valvular heart disease. However, it is associated with the risk of serious post-operative complications, including death. In the risk assessment of cardiac surgery, risk calculators are used—in European conditions, EuroSCORE II is most often used (1). The reliability of risk calculators is relatively high in surgical revascularization of the myocardium, however, in patients qualified for cardiac valve surgery, there are significant discrepancies between the risk of surgery predicted by risk calculators and actual mortality (2-5). The presented study investigated the utility of commonly used risk calculators in the group of polish patients undergoing aortic valve replacement (AVR) because of aortic stenosis.
Methods
This was a prospective study of consecutive patients with hemodynamically significant aortic stenosis (a valve area below 1 cm2 and/or a mean pressure gradient ≥40 mmHg) undergoing AVR. The exclusion criteria were: a lack of consent to participate in the study and age under 18 years. Once a patient gave his/her consent to participate, the risk of surgery using EuroSCORE II and STS (from 2008) was calculated for each patient. The day before surgery a blood sample for biomarkers was collected from each patient. Complete blood count was performed with K2-EDTA samples, using a Cobas 6000 electronic counter (Roche, Mannheim, Germany). The primary end-point was death from all causes in 30-day follow-up. The secondary end-point was death from all causes in 1-year follow-up. All procedures were performed through a midline sternotomy incision under general anaesthesia in a normothermia. Patients were followed by direct observation during hospitalization, clinic visits, or telephone interviews for 30 days and 1 year after the surgery. The study was conducted at the Institute of Cardiology, Warsaw, between 2014 and 2018. The protocol was approved by the Institutional Ethics Committee of Institute of Cardiology, Warsaw, Poland (number 1705). All participants they gave their informed consent before taking part in the study.
Statistical analysis
A statistical analysis was performed using SAS version 9.2. Data are presented as the mean ± SD and the frequency (%). Logistic regression was used to assess relationships between variables. The following preoperative covariates: age, left ventricular ejection fraction, NYHA classes, creatinine, EuroSCORE II, STS score, high-sensitivity C-reactive protein (hs-CRP), high-sensitivity troponin T (hs-TnT), hematocrit, hemoglobin, N-terminal of the prohormone brain natriuretic peptide (NT-proBNP), platelets, red cell distribution width (RDW), red blood cell count (RBC) and white blood cell count were investigated for association with the 1-year mortality in univariate analysis. Significant determinants (P<0.05) identified from univariate analysis were subsequently entered into multivariate models. The Hosmer-Lemeshow test was performed to evaluate goodness of fit within equally sized subgroups in increasing order of patient risk. For calibration analysis, a P value of >0.05 indicated a well-calibrated model. Area under the receiver operative characteristics curves (c-statistics) with 95% confidence intervals (95% CI) were used to assess the discriminative ability of risk scores EuroSCORE II and STS for 30-day and 1-year survival following aortic valve surgery. The cut-off value and the log-rank test to compare the curves were employed. All tests were two-tailed and P<0.05 considered statistically significant.
Results
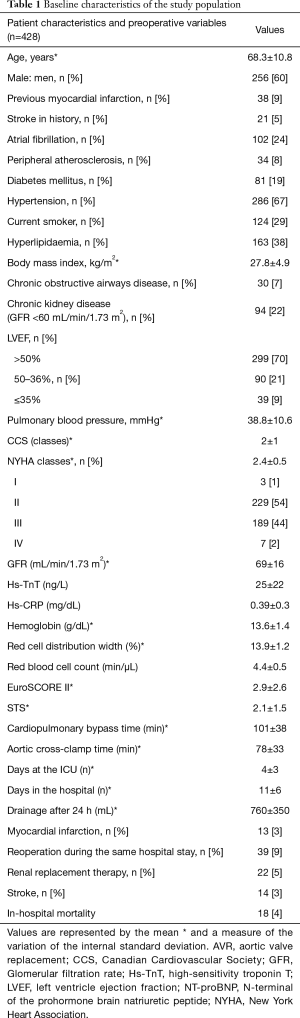
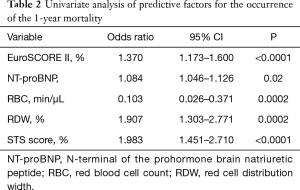
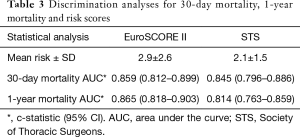
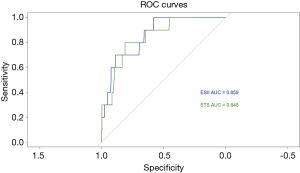
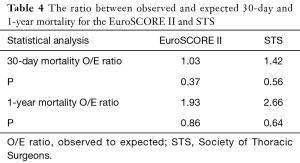
The study included 428 patients who underwent aortic valve. The mean age in the study group was 68.3 (±10.8) and 60% (n=256) patients were men. Baseline characteristics of the patients are presented in Table 1. In 278 patients, a biological aortic valve prosthesis was implanted, and in 150 a mechanical valve. Thirteen patients died during the 30-day follow-up period as a result of gradually increasing multi-organ failure and 25 patients died during 1-year follow-up. Statistically significant predictors of 1-year mortality at univariate analysis are presented in Table 2. At multivariate analysis RDW (OR 2.185; 95% CI: 1.315–3.630; P=0.002) and RBC (OR 0.118; 95% CI: 0.014–0.987; P=0.04) remained independent predictors of the 1-year mortality. The actual 30-day and annual mortality was 3.0% and 5.8% respectively vs. mortality 2.9% predicted by the EuroSCORE II and 2.1% by the STS model. Table 3 shows the discrimination of 30-day and 1-year mortality by scores. The EuroSCORE II and STS risk calculators did not differ in their predictive ability both for 30-day mortality prediction (P=0.499) and 1-year mortality (P=0.765). Figure 1 shows the areas under receiver operator characteristic curves of EuroSCORE II and STS score for 30-day survival following AVR surgery. The Hosmer-Lemeshow testing revealed good calibration of the EuroSCORE II and the STS score for 30-day and 1-year mortality in patients undergoing aortic valve surgery (Table 4).
Full table
Full table
Full table
Full table
Discussion
This is the first prospective study evaluating the utility of EuroSCORE II and STS risk calculators in polish population of patients with severe aortic stenosis undergoing classical AVR surgery for predicting 30-day and 1-year mortality.
The risk calculators are used to assess the surgical risk of heart valve surgery. In European conditions they are EuroSCORE II and less often American STS (1-8). EuroSCORE—European System for Cardiac Operative Risk Evaluation, was a first European tool for calculating the risk of death in the early postoperative period. The EuroSCORE was published in 1999 (9). Gradually accepted, it has become a commonly used tool for risk assessment in patients treated with cardiac surgery. Its use in everyday practice significantly contributed to the improvement of the results of heart surgery at the beginning of the new millennium. However, due to the discrepancy between the predicted and the actual mortality, at the 25th meeting of the European Association of Cardio Thoracic Surgery (EACTS) in Lisbon in October 2011 a new revised EuroSCORE II model was published and next available in the form of an electronic calculator in April 2012. The first reports on the use of EuroSCORE II indicated a significant improvement in risk calibration compared to older model, however, in the subsequent articles appearing there were also discrepancies between the predicted and the actual perioperative mortality (1,5,10,11).
Available literature indicates significant limitations on both the EuroSCORE calculator, the revised version—EuroSCORE II and the American STS (2-5,12). There is a tendency to overestimate the risk of death in patients undergoing heart valve surgery using EuroSCORE and for low risk patients using STS. In turn, the calculation of death risk with using EuroSCORE II reduces the risk especially in patients with numerous additional diseases (2,10). There have been reports that the EuroSCORE II scale did not improve the risk assessment in patients undergoing isolated AVR surgery. In the Chalmers et al.’s study on a group of 814 patients undergoing AVR surgery, the actual 30-day mortality was 2.3% vs. 7.1% predicted by the EuroSCORE and 2.1% by the EuroSCORE II calculator. In spite of similar actual mortality to the EuroSCORE II calculation result, the EuroSCORE II calculator did not improve the predictive ability of mortality as compared to EuroSCORE (C-statistic values: 0.69 vs. 0.67) (5).
In the presented study, the EuroSCORE II and STS calculators showed a significantly better discrimination ability to predict both 30-day mortality as well as 1-year compared to the EuroSCORE calculator. On the other hand, discriminatory abilities of EuroSCORE II calculators and STS did not differ significantly between themselves. The calibration capacity, i.e., the correspondence between the predicted and observed mortality, was the closest when using the EuroSCORE II calculator (3.0% vs. 2.9%), compared to the STS (2.1%) model. Thus, the results of the presented study indicate satisfactory discrimination and calibration of the EuroSCORE II and STS calculator in the group of patients with aortic stenosis undergoing valve replacement by the classical method. It seems that in Polish conditions, the EuroSCORE II or STS calculator should be the tool of choice for assessing the risk of death in patients with severe aortic stenosis qualified for AVR. However, it is worth noting that the available risk calculators do not allow accurate estimation of perioperative mortality due to insufficient calibration and discrimination (10). Accurate qualification for surgical treatment of valvular heart disease seems to be important also due to the development of new alternative treatments for heart disease, such as TAVI, for patients with medium or high risk of surgery (13). Therefore, it seems reasonable to put forward the thesis that our knowledge about predictors requires supplementation and, therefore, further research, in order to better calibrate and discriminate against the anticipated risk. Based on the research carried out so far, it seems that biomarkers such as RDW, RBC, Troponin T or frailty may be useful in improving discrimination against the EuroSCORE II calculator (14-19). Moreover, it is worth noting that when qualifying a patient for cardiac surgery, it is necessary to assess the therapeutic resources of a given center (including staff training), the results of postoperative treatment and the results of percutaneous intervention (6,20). The decision to treat cardiac surgery should be made after a detailed analysis of experts (hearteam), in consultation with the patient and his family, in order to choose the most optimal type of therapy (21,22).
Acknowledgments
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The protocol was approved by the Institutional Ethics Committee of Institute of Cardiology, Warsaw, Poland (number 1705) and written informed consent was obtained from all patients.
References
- Nashef SA, Roques F, Sharples LD, et al. EuroSCORE II. Eur J Cardiothorac Surg 2012;41:734-44. [Crossref] [PubMed]
- Kuwaki K, Inaba H, Yamamoto T, et al. Prospective validation of EuroSCORE II EuroSCORE II and the Society of Thoracic Surgeons Score in patients undergoing aortic valve replacement for aortic stenosis. J Cardiovasc Surg (Torino) 2015;56:455-62. [PubMed]
- Borracci RA, Rubio M, Celano L, et al. Prospective validation of EuroSCORE II in patients undergoing cardiac surgery in Argentinean Centres. Interact Cardiovasc Thorac Surg 2014;18:539-43. [Crossref] [PubMed]
- Grant SW, Hickey GL, Dimarakis I, et al. Performance of the EuroSCORE Models in Emergency Cardiac Surgery. Circ Cardiovasc Qual Outcomes 2013;6:178-85. [Crossref] [PubMed]
- Chalmers J, Pullan M, Fabri B, et al. Validation of EuroSCORE II in a modern cohort of patients undergoing cardiac surgery. Eur J Cardiothorac Surg 2013;43:688-94. [Crossref] [PubMed]
- Baumgartner H, Falk V, Bax J, et al 2017 ESC/EACTS. Guidelines for the management of valvular heart disease. European Heart Journal 2017;38.2739-91.
- Osnabrugge RL, Speir AM, Head SJ, et al. Performance of EuroSCORE II in a large US database: implications for transcatheter aortic valve implantation. Eur J Cardiothorac Surg 2014;46:400-8. [Crossref] [PubMed]
- Barili F, Pacini D, Capo A, et al. Does EuroSCORE II perform better than its original versions? A multicentre validation study. Eur Heart J 2013;34:22-9. [Crossref] [PubMed]
- Nashef SA, Roques F, Michel P, et al. European system for cardiac operative risk evaluation (EuroSCORE). Eur J Cardiothorac Surg 1999;16:9-13. [Crossref] [PubMed]
- Parolari A, Pesce LL, Trezzi M, et al. EuroSCORE performance in valve surgery: a meta-analysis. Ann Thorac Surg 2010;89:787-93. [Crossref] [PubMed]
- Gammie JS, O'Brien SM, Griffith BP, et al. Influence of hospital procedural volume on care process and mortality for patients undergoing elective surgery for mitral regurgitation. Circulation 2007;115:881-7. [Crossref] [PubMed]
- van Gameren M, Kappetein AP, Steyerberg EW, et al. Do we need separate risk stratification models for hospital mortality after heart valve surgery? Ann Thorac Surg 2008;85:921-30. [Crossref] [PubMed]
- Collas VM, Van De Heyning CM, Paelinck BP, et al. Validation of transcatheter aortic valve implantation risk scores in relation to early and mid-term survival: a single-centre study. Interact Cardiovasc Thorac Surg 2016;22:273-9. [Crossref] [PubMed]
- Duchnowski P, Szymański P, Orłowska-Baranowska E, et al. Raised red cell distribution width as a prognostic marker in aortic valve replacement surgery. Kardiol Pol 2016;74:547-52. [PubMed]
- Duchnowski P, Hryniewiecki T, Stokłosa P, et al. Red Cell Distribution Width as a Prognostic Marker in Patients Undergoing Valve Surgery. J Heart Valve Dis 2017;26:714-20. [PubMed]
- Duchnowski P, Hryniewiecki T, Kuśmierczyk M, et al. Red cell distribution width as a predictor of multiple organ dysfunction syndrome in patients undergoing heart valve surgery. Biol Open 2018. [Crossref] [PubMed]
- Petäjä L, Røsjø H, Mildh L, et al. Predictive value of high-sensitivity troponin T in addition to EuroSCORE II in cardiac surgery. Interact Cardiovasc Thorac Surg 2016;23:133-41. [Crossref] [PubMed]
- Duchnowski P, Hryniewiecki T, Kuśmierczyk M, et al. High-sensitivity troponin T as a prognostic marker in patients undergoing aortic valve replacement. Pol Arch Intern Med 2017;127:628-30. [Crossref] [PubMed]
- Duchnowski P, Hryniewiecki T, Stokłosa P, et al. Number of erythrocytes as a prognostic marker in patients undergoing heart valve surgery. Kardiol Pol 2018;76:791-3. [Crossref] [PubMed]
- Vahanian A, Alfieri O, Andreotti F, et al. Guidelines on the management of valvular heart disease (version 2012). Eur Heart J 2012;33:2451-96. [Crossref] [PubMed]
- Adams DH, Rosenhek R, Falk V. Degenerative mitral valve regurgitation: best practice revolution. Eur Heart J 2010;31:1958-66. [Crossref] [PubMed]
- Montori VM, Ting HH. Sharing decision making about cardiac surgery: improving the quality of the decision to undergo or forego surgery. Circ Cardiovasc Qual Outcomes 2009;2:519-21. [Crossref] [PubMed]


