
Sublobar resection is associated with better perioperative outcomes in elderly patients with clinical stage I non-small cell lung cancer: a multicenter retrospective cohort study
Introduction
Lung cancer is a disease often seen in the elderly. Appropriately 50% of newly diagnosed cases are aged 70 years or older, representing the fastest-growing segment of non-small cell lung cancer (NSCLC) (1). Meanwhile, the recent advance in technology and the overall aging of the population are expected to provoke the increased incidence of NSCLC in the elderly, especially for those at early-stage (2,3). Also, the advanced age and easy access to CT scan make it possible to diagnose some previously undiagnosed cases during their lifetime, which may also contribute to the increasing incidence of NSCLC observed. Nevertheless, it is estimated that the incidence of NSCLC in elderly patients (≥65 years) will rise 67% annually from 163,000 in 2010 to 271,000 in 2030 (4). This dramatic increase will surely cause a substantial global burden on the health care system.
Surgical resection is generally considered as the potentially curative option for early-stage NSCLC (5,6), including elderly patients (7). Regarding the type of surgery, most surgeons today would still acknowledge lobectomy as the major chance for curing early-stage disease in the elderly (2,8). However, increasing evidence has recently emerged and supported more limited resections for early-stage NSCLC in elderly patients when compared with lobectomy, with similar or non-inferior survival and better perioperative outcomes and less perioperative complications (7,9,10). Also, the advantages of reduced hospital stay and better preserved pulmonary function were also reported in patients underwent sublobar resection for early-stage NSCLC (11,12). Sublobar resection was suggested for very selected patients, such as those with advanced age and poor pulmonary function (13,14).
Unfortunately, despite the burgeoning population of early NSCLC in the elderly, almost all evidence for sublobar resection were derived from retrospective studies (15). Current evidence available for sublobar resection is ambiguous to establish the safety and effectiveness for early-stage NSCLC in the elderly. The conflicting results of inferior survival and limited lymph node removal were reported for sublobar resection (16). Sublobar resection was suggested not to be equivalent to lobectomy in older patients with adenocarcinoma (16,17). Meanwhile, the last major trial available to address this question was carried out over 20 years ago (18). Although the results were in favor of lobectomy, several issues complicated their straightforward application in modern practice (2). To address this issue, several multicenter randomized trials are ongoing to comparatively study the sublobar section vs. lobectomy for (elderly) patients with clinical stage IA NSCLC in USA (19), Japan (20) and China (21). Whereas the results are unlikely to be available soon. To help bridge this gap while awaiting trial results, we compared the clinical outcomes of sublobar resection vs. lobectomy in elderly patients (≥65 years) with clinical stage I NSCLC using the real-world data from electronic medical records of 10 tertiary hospitals in China.
Methods
Study population
Clinical data of lung cancer patients who underwent surgical resection at the Department of Thoracic Surgery of 10 tertiary hospitals in China were retrospectively reviewed based on the national collaborative prospective lung cancer database (LinkDoc Technology Co, Ltd., Beijing, China). Between January 2014 and September 2017, a total of 21,790 patients were identified. Eligible patients were those aged 65 years or older and underwent sublobar resection or lobectomy for clinical stage I disease. A cutoff value of 65 years was set to define the elderly patients according to retirement age and commonly associated definitions of an elder age. Patients without pathological confirmation of NSCLC were excluded. Other exclusion criterion was the use of preoperative therapies (chemotherapy, radiotherapy or biological treatment). These criteria yielded a sample size of 1,579. All procedures performed in this study were in accordance with the ethical standards of the Helsinki Declaration and were approved by the Ethics Committee of all participating centers (the ID of Ethic Approval is 2018-13-K08). Formal consent was not required for this retrospective study.
Clinical staging and treatments
The preoperative staging was performed in all patients by computed tomography scan with or without positron emission tomography at the discretion of surgeons in charge. Surgical information was determined from procedure documented in the medical records and was classified as lobectomy or sublobar resection. All tumors were staged according to the 7th edition of the American Joint Commission on Cancer classification (22). Tumor histology was classified according to the World Health Organization criteria (23). Treatment-related variables including surgical procedures, surgical margins, operation time, intraoperative blood loss, the number of lymph node dissection, duration of chest drainage and hospital stay, as well as perioperative complications, were analyzed to evaluate perioperative outcomes and safety of sublobar resection in the target population.
Other clinical data
Patient demographic and clinical characteristics were abstracted from the prospective LinkDoc database, including age at the time of surgery, sex, smoking history, comorbidity, body mass index (BMI), tumor size, location, histology and pathologic TNM stage, as well as preoperative pulmonary function tests [forced expiratory volume in 1 second (FEV1) and carbon monoxide diffusing capacity (DLCO)]. Follow-up data were also retrieved from the medical records of each patient. Survival patients were contacted by telephone interview. Cause of death was established from medical records or interview. All patients were followed up until February 20th, 2019.
Statistical analysis
Overall survival of the patients was determined from the date of surgery to the date of death or last follow up. Continuous variables are expressed as mean ± standard deviation (SD) and compared by rank-sum test. Categorical variables are presented as frequency and percentage and calculated via Chi-square test or Fisher exact test when appropriate. Overall survival was analyzed by the Kaplan-Meier method and compared between groups (lobectomy and sublobar resection or segmentectomy) by using the log-rank test.
In view of potential selection bias, propensity score matching was calculated to construct a matched sample of patients who underwent sublobar resection and lobectomy. Of the original 1,579 patients, 513 were removed secondary to pathologic stage II/III or procedures other than video-assisted thoracoscopic surgery (VATS), leaving 1,066 patients (750 lobectomy and 316 sublobar resections) for propensity score matching analysis. The independent variables included were age at surgery, sex, smoking history, tumor size, location and histology, and preoperative FEV1. Patients were matched 1:1 using the nearest-neighbor method with the caliper set at 0.2. All statistical analyses were two-sided and P<0.05 was considered as statistically significant (SAS version 9.4, SAS Institute, Cary, NC, USA).
A cut-off of 65 years was used to define elderly patients in this study. However, there is no international agreement on the definition of elderly patients. Increasing the age of patients may be meaningful. A subgroup analysis of patients aged over 75 years old was therefore carried out. Besides, in view of potential selection or surgical bias, subgroup analyses of patients aged over 75 years old, with pathologic stage I NSCLC, and those who smoking or undergoing VATS were also carried out regarding lobar and sublobar resections. Also, subgroup analysis of patients undergoing segmentectomy and lobectomy was conducted. Moreover, sensitivity analyses were performed by excluding center with larger patient number to adjust for potential center effect.
Results
Baseline and tumor characteristics
Among 1,579 surgically resected early-stage patients, 1,164 (73.7%) were treated by lobectomy and 415 (26.3%) by sublobar resection (106 segmentectomy and 309 wedge resection). The mean age of patients was 70.49 years with an equal sex distribution. Baseline characteristics of the patients are summarized in Table 1. Patients undergoing sublobar resection were older and had more comorbidities (like hypertension and coronary artery disease). In both groups, most patients were non-smokers with no significant differences regarding smoking history, sex, BMI and preoperative pulmonary function (P>0.05, Table 1). As for the surgical procedures, sublobar resection was more frequently performed by VATS.
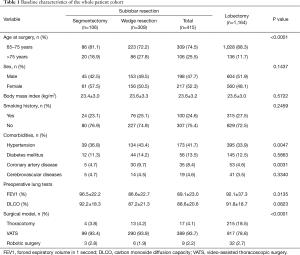
Full table
As shown in Table 2, sublobar resection was more likely to be performed in patients with smaller, left-sided tumors, at earlier stage and with histology of adenocarcinoma. Importantly, pathologic upstaging occurred more often in lobar resection group than that of sublobar group (14.7% vs. 2.3%, P<0.0001).
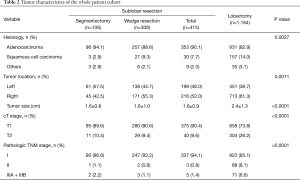
Full table
Unadjusted perioperative outcomes and short-term survival
Patients undergoing sublabor resection had less intraoperative blood loss, shorter operation time and hospital stay (Table 3). Fewer patients treated by sublobar resection had lymph node dissection done (57.1% vs. 96.1%, P<0.0001), especially for those by wedge resection (45.3%). Also, patients in sublobar resection group had less lymph nodes dissected (median: 5 vs. 11, P<0.0001).
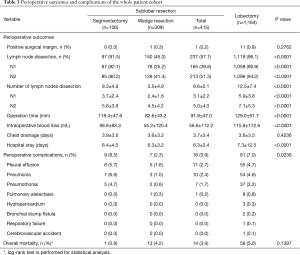
Full table
Meanwhile, fewer perioperative complications were observed in patients undergoing sublabor resection (3.9% vs. 7.0%, P=0.0238). Perioperative mortalities at 30 and 90 days were 2 and 5 patients, and all in the lobectomy group. The median follow-up time was 21.3 and 21.2 months in subloar and lobar resection groups, respectively. Seventy-two patients died during follow-up, 14 in sublobar group and 58 in lobar group (3.4% vs. 5.0%, P=0.1397). Forty-two patients died from cancers. Eleven patients died from other diseases, commonly cardiovascular and cerebrovascular diseases. The corresponding information was unknown for the remaining 19 patients.
Propensity score-matched analysis
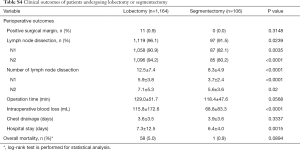
Propensity score matching resulted in 122 patients in each arm. The two cohorts were well-matched in the major clinical characteristics (Table 4).
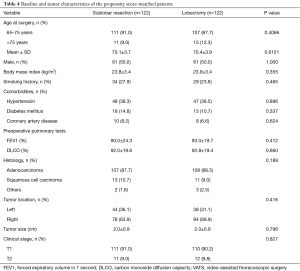
Full table
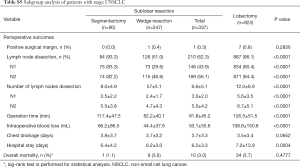
Of the matched patients, there were still significant differences between the two treatment strategies with respect to perioperative outcomes including intraoperative blood loss P<0.0001), operation time (P<0.0001), and duration of tube drainage (P<0.0001) and hospital stay (P=0.0049, Table 5). Also, the proportion of patients underwent lymph node dissection and the number of lymph nodes harvested were still significantly lower in sublobar resection group (65.6% vs. 95.9% and 6.9±5.1 vs. 11.3±6.5, P<0.0001, Table 5). However, after adjusted in a propensity-matched analysis, postoperative complications were found to occur significantly more frequent with sublobar resection than with lobectomy (3.3% vs. 0.0%, P=0.0437). Meanwhile, the difference in short term survival remained unchanged in the matched patients (0.8% vs. 1.6%, P=0.5917).
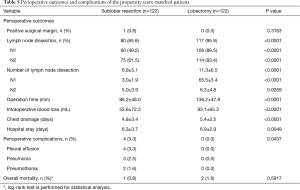
Full table
Subgroup analysis and sensitivity analysis
A cut-off of 65 years was used to define elderly patients in this study. However, there is no international agreement on the definition of elderly patients. A subgroup analysis of patients aged over 75 years old was therefore carried out. Patients undergoing sublobar resection were still older and had smaller, left sided and earlier stage tumors (Table S1). Meanwhile, less intraoperative blood loss, shorter operation time and hospital stay were observed in those undergoing sublobar resection (Table S2). Also, lymph node dissection was still limited in the sublobar group (58.5% vs. 94.9%, P<0.0001). Nine (6.6%) patients died in lobar group and 2 (1.9) died in sublobar group during a median follow-up time of 18.6 and 21.4 months, respectively (P=0.0582).
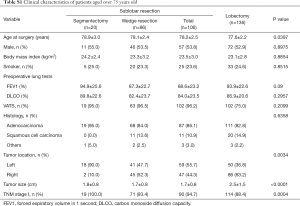
Full table
Full table
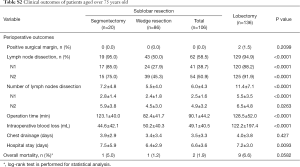
In view of known potential bias of wedge resection in lymph node dissection, subgroup analysis of segmentectomy and lobectomy was further carried out. More patients undergoing segmentectomy were aged older (>75 years), and had smaller, earlier-staged, left-sided tumor and with histology of adenocarcinoma. Meanwhile, segmentectomy was more frequently performed by VATS (Table S3). Also, segmentectomy was still significantly associated with less lymph node dissection, blood loss and hospital stay (Table S4). However, no significant difference was found in operative time, chest drainage and overall mortality between segmentectomy and lobectomy.
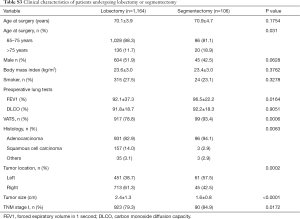
Full table
Full table
Besides, almost all patients undergoing sublobar resection were at pathologic stage I and by VATS. Whereas, approximately 15% of patients undergoing lobectomy were upstaged (II or III) or via thoracotomy. Subgroup analysis of patients at stage I or underwent VATS were carried out in terms of both complications and overall survival. The superiority in perioperative outcomes remained significantly in favor of sublobar resection in stage I or VATS subgroups (Tables S5 and S6).
Full table
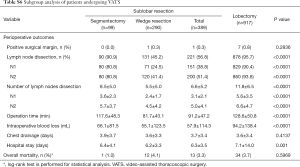
Full table
Moreover, most patients in this study were non-smokers. We then considered examining more the smoker subgroup. No significant difference in the duration of hospital stay was observed between sublobar and lobar resection in smokers, and also the cases of chest drainage and overall mortality (Table S7).
Full table
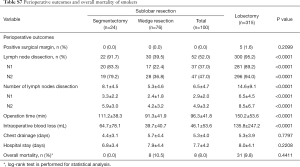
Additionally, work experience and management criteria of individual surgeon or center may vary in this electronic medical records-based multicenter study. Sensitivity analyses were further carried out by excluding centers with larger patient number to adjust for potential center effect. No significant center effect was observed regarding perioperative outcomes excepting chest draining, which showed some variations among the centers (Table S8).
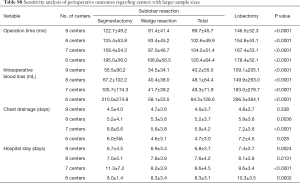
Full table
Discussion
Nowadays, increasing attention has been focused on sublobar resection as an alternative therapy for elderly patients with early-stage NSCLC. The contradictory results of previous studies have prompted us to further investigate the clinical outcomes of sublobar resection in elderly patients with clinical stage I NSCLC. The findings of our propensity score matching analysis demonstrated the significant perioperative advantages of sublobar resection, with less intraoperative blood loss, drainage days, operation time and hospital stay. Meanwhile, short term survival analysis showed no significant difference between the two treatment strategies. The ongoing long term follow up may help to better clarify the survival difference with respect to sublobar resection.
Sublobar resection has been recommended for highly selected patients, such as those with poor pulmonary functions or other major comorbidity that contraindicates lobectomy, according to the NCCN guidelines (5). In clinical practice, it was reported to be more frequently performed in patients with elder age, smaller, less malignant tumors and those with impaired pulmonary function (24,25). In our study, patients undergoing sublobar resection were older, and had more comorbidities and comparatively poor pulmonary function, although the difference in perioperative pulmonary function did not reach the statistical significance. In addition, tumors treated by sublobar resection were more often smaller, left-sided with histology of adenocarcinoma. To adjust for the potential selection bias, propensity score matching analysis was carried out. Our adjusted analysis showed the significant association of sublobar resection with better perioperative outcomes. These results were consistent with previous study of elderly patients in China by Qiu et al., which indicated less blood loss and chest tube days, as well as shorter duration of operation and hospital stay in a comparatively small number of patients undergoing sublobar resection for stage I NSCLC (245 elderly, ≥65 years, pathologic stage I NSCLC patients, 39 sublobectomy and 206 lobectomy) (10). Other previous studies indicated that sublobar resection did not offer improved perioperative complications, mortality or postoperative pulmonary function (18,26,27). However, the conflicting results of fewer major complications and shorter hospital stay were also noted following limited resection when compared with lobectomy. It has been thought to be reasonably explained by lung parenchyma preservation of less invasive sublobar resection (12,24). Several possibilities may help to explain these conflicting results, like the differences in surgical technology, perioperative patient care, study population, and study design. Some previous studies have focused on the patients with pathologic stage I NSCLC (2,7,28), while others mainly focused on those with clinical stage I NSCLC (24,26). Still, others only took patients with stage IA NSCLC into consideration (9,27). Furthermore, some studies mainly focused on the elderly patient, while others did not make such restrictions (29,30). The definitions of elderly patients also varied a lot, from 65 to 75 years old. In view of the meaningfulness of increasing age, a subgroup analysis of patients with elder age was further carried out. Similar results were obtained when limiting patients to those aged over 75 years old. In additions, wedge resection is generally considered to be different from segmentectomy in operative approach and morbidity. Our subgroup analysis of segmentectomy and lobectomy showed superior perioperative outcomes of segmentectomy without compromising short-term survival of patients. Nevertheless, the findings of our study corroborating the previous study of Qiu et al. allowed us to conjecture that sublobar resection can offer better perioperative outcomes than lobectomy in elderly Chinese patients with clinical stage I NSCLC.
Sublobar resection has been reported to show survival outcomes no different from lobectomy for management of early-stage NSCLC in the elderly. However, contradictory results of inferior survival were also reported. Previous study by Shirvani et al. indicated significant association of sublobar resection with worse overall survival in propensity score-matching analysis (HR: 1.36, 95% CI: 1.17–1.58, P<0.001) (2). Meanwhile, Veluswamy and colleagues reported the equivalence of lobectomy with segmentectomy, but not with limited resection, in early stage lung adenocarcinoma (16). The reason has been ascribed to comparatively worse survival outcome of nonanatomic wedge resection (31). Yet, others argued about the comparable outcome of wedge resection and segmentectomy in patients with cT1N0 NSCLC (32). In our study, short term survival analysis showed a non-inferior survival rate of patients undergoing lobectomy and sublobar resections. Thirteen out of 14 patients died in sublobar resection group were treated by wedge section. Subgroup analysis of segmentectomy and lobectomy also showed no significant survival difference. In additions, our other subgroup analyses also showed superior perioperative outcomes without compromising short-term survival of patients. Unfortunately, long term survival outcome is not available in the current status for us to clarify further the survival difference between lobar and sublobar resections or segmentectomy. One thing worth noting here is that pathologic upstaging was found to occur more frequently in patients undergoing lobectomy when compared with sublobar resection (14.7% vs. 0.9%, P<0.0001). Meanwhile, sublobar resection was significantly associated with less lymph node dissection, especially for wedge resection. We may not exclude the possibility that better perioperative outcomes observed in our sublobar patients were at the expense of less lymph node taken. Stringent preclinical evaluation and procedure selection are therefore of major importance for clinical management of this early-stage disease.
Sublobar resection has known to involve limited lymph node dissection (26). The latter was identified as an independent predictor of outcomes in patients with stage T1a or I NSCLC (9,33). Failure to examine lymph nodes may be a major challenge in patients undergoing sublobar resection (13). Accurate lymph node staging in combination with a minimally invasive approach was suggested to play more of a factor than the extent of resection (28). Moreover, the study by De Zoysa et al. indicated that there was no appreciable difference between lobectomy and sublobar resection in terms of survival when the adequate nodal dissection was accounted for (12). Qu et al. found the equivalent survival of patients managed by segmentectomy or lobectomy when under analogous extent of lymph node removal (17). In this regard, it may be reasonable to assume that the extended sublobar resection including systemic lymphadenectomy may be a solution that can help to better management of the older, frail patients (34), but it obviously requires further evaluation.
Not long enough follow-up time is the major obstacle that prevents us from fully understanding the clinical outcome of sublobar resection in elderly patients with clinical stage I NSCLC. Besides, the number of patients is comparatively smaller, especially for those of segmentectomy (35). Also, the potential surgical or selection bias and the heterogeneity of procedures performed and management criteria or policy of each center may exist in this electronic medical records-based multicenter retrospective study. We have attempted to address these limitations by using the propensity score matching, subgroup analysis, and sensitivity analyses. Future studies are still needed to better elucidate the perioperative and long-term outcomes of sublobar resection for elderly patients with clinical stage I NSCLC.
In conclusion, the data of our real-world study showed better perioperative outcomes of sublobar resection without compromising short term survival of elderly patients with clinical stage I NSCLC. However, accurate lymph node staging is the major consideration that should lead us to favor lobectomy over sublobar resection when an issue. Sublobar resection appears to offer better perioperative outcomes in patients with stringently diagnosed early-stage lung cancers.
Acknowledgments
The study database was developed by LinkDoc (Beijing) Technology Co. Ltd.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: All procedures performed in this study were in accordance with the ethical standards of the Helsinki Declaration and were approved by the Ethics Committee of all participating centers (the ID of Ethic Approval is 2018-13-K08). Formal consent was not required for this retrospective study.
References
- Pallis AG, Gridelli C, Wedding U, et al. Management of elderly patients with NSCLC; updated expert's opinion paper: EORTC Elderly Task Force, Lung Cancer Group and International Society for Geriatric Oncology. Ann Oncol 2014;25:1270. [PubMed]
- Shirvani SM, Jiang J, Chang JY, et al. Lobectomy, sublobar resection, and stereotactic ablative radiotherapy for early-stage non-small cell lung cancers in the elderly. JAMA Surg 2014;149:1244. [PubMed]
- National Lung Screening Trial Research Team, Aberle DR, Adams AM, et al. Reduced lung-cancer mortality with low-dose computed tomographic screening. N Engl J Med 2011;365:395-409. [PubMed]
- Smith BD, Smith GL, Hurria A, et al. Future of cancer incidence in the United States: burdens upon an aging, changing nation. J Clin Oncol 2009;27:2758-65. [PubMed]
- Ettinger DS, Borghaei H, Akerley W. NCCN Clinical Practice Guidelines in Oncology – Non-Small Cell Lung Cancer. J Natl Compr Canc Netw 2015;2:548-82. [PubMed]
- Smythe WR. Treatment of stage I and II non-small-cell lung cancer. Cancer Control 2001;8:318-25. [PubMed]
- Kilic A, Schuchert MJ, Pettiford BL, et al. Anatomic segmentectomy for stage I non-small cell lung cancer in the elderly. Ann Thorac Surg 2009;87:1662-6; discussion 1667-8.
- Zhang Y, Yuan C, Zhang Y, et al. Survival following segmentectomy or lobectomy in elderly patients with early-stage lung cancer. Oncotarget 2016;7:19081-6. [PubMed]
- Razi SS, John MM, Sainathan S, et al. Sublobar resection is equivalent to lobectomy for T1a non-small cell lung cancer in the elderly: a Surveillance, Epidemiology, and End Results database analysis. J Surg Res 2016;200:683. [PubMed]
- Qiu C, Wang G, Xu J, et al. Sublobectomy versus Lobectomy for Stage I Non-Small Cell Lung Cancer in the elderly. Int J Surg 2017;37:1-7. [PubMed]
- Harada H, Okada M, Sakamoto T, et al. Functional advantage after radical segmentectomy versus lobectomy for lung cancer. Ann Thorac Surg 2005;80:2041-5. [PubMed]
- De Zoysa MK, Hamed D, Routledge T, et al. Is limited pulmonary resection equivalent to lobectomy for surgical management of stage I non-small-cell lung cancer? Interact Cardiovasc Thorac Surg 2012;14:816-20. [PubMed]
- Sihoe AD, Van Schil P. Non-small cell lung cancer: when to offer sublobar resection. Lung Cancer 2014;86:115-20. [PubMed]
- Blanco R, Maestu I, de la Torre MG, et al. A review of the management of elderly patients with non-small-cell lung cancer. Ann Oncol 2015;26:451-63. [PubMed]
- Donington JS. Point: are limited resections appropriate in non-small cell lung cancer? Yes. Chest 2012;141:588. [PubMed]
- Veluswamy RR, Ezer N, Mhango G, et al. Limited Resection Versus Lobectomy for Older Patients With Early-Stage Lung Cancer: Impact of Histology. J Clin Oncol 2015;33:3447-53. [PubMed]
- Qu X, Wang K, Zhang T, et al. Long-term outcomes of stage I NSCLC (≤3 cm) patients following segmentectomy are equivalent to lobectomy under analogous extent of lymph node removal: a PSM based analysis. J Thorac Dis 2017;9:4561-73. [PubMed]
- Ginsberg RJ, Rubinstein LV. Randomized trial of lobectomy versus limited resection for T1 N0 non-small cell lung cancer. Lung Cancer Study Group. Ann Thorac Surg 1995;60:615-22. [PubMed]
- Kohman LJ, Gu L, Altorki N, et al. Biopsy first: Lessons learned from Cancer and Leukemia Group B (CALGB) 140503. J Thorac Cardiovasc Surg 2017;153:1592-7. [PubMed]
- Nakamura K, Saji H, Nakajima R, et al. A phase III randomized trial of lobectomy versus limited resection for small-sized peripheral non-small cell lung cancer (JCOG0802/WJOG4607L). Jpn J Clin Oncol 2010;40:271-4. [PubMed]
- Yang F, Sui X, Chen X, et al. Sublobar resection versus lobectomy in Surgical Treatment of Elderly Patients with early-stage non-small cell lung cancer (STEPS): study protocol for a randomized controlled trial. Trials 2016;17:191. [PubMed]
- Edge SB, Byrd DR, Compton CC, et al. AJCC Cancer Staging Manual 7th edition. New York: Springer, 2010.
- Detterbeck FC, Boffa DJ, Tanoue LT. The new lung cancer staging system. Chest 2009;136:260-71. [PubMed]
- Tsutani Y, Tsubokawa N, Ito M, et al. Postoperative complications and prognosis after lobar resection versus sublobar resection in elderly patients with clinical Stage I non-small-cell lung cancer. Eur J Cardiothorac Surg 2018;53:366-71. [PubMed]
- Birdas TJ, Koehler RP, Colonias A, et al. Sublobar resection with brachytherapy versus lobectomy for stage Ib nonsmall cell lung cancer. Ann Thorac Surg 2006;81:434-8; discussion 438-9. [PubMed]
- Landreneau RJ, Normolle DP, Christie NA, et al. Recurrence and survival outcomes after anatomic segmentectomy versus lobectomy for clinical stage I non-small-cell lung cancer: a propensity-matched analysis. J Clin Oncol 2014;32:2449-55. [PubMed]
- Okami J, Ito Y, Higashiyama M, et al. Sublobar resection provides an equivalent survival after lobectomy in elderly patients with early lung cancer. Ann Thorac Surg 2010;90:1651. [PubMed]
- Smith CB, Kale M, Mhango G, et al. Comparative outcomes of elderly stage I lung cancer patients treated with segmentectomy via video-assisted thoracoscopic surgery versus open resection. J Thorac Oncol 2014;9:383-9. [PubMed]
- Zhao ZR, Situ DR, Lau RWH, et al. Comparison of Segmentectomy and Lobectomy in Stage IA Adenocarcinomas. J Thorac Oncol 2017;12:890-6. [PubMed]
- Speicher PJ, Lin G, Gulack BC, et al. Sublobar Resection for Clinical Stage IA Non-small Cell Lung Cancer in the United States. Clin Lung Cancer 2016;17:47-55. [PubMed]
- Smith CB, Swanson SJ, Mhango G, et al. Survival after segmentectomy and wedge resection in stage I non-small-cell lung cancer. J Thorac Oncol 2013;8:73-8. [PubMed]
- Altorki NK, Kamel MK, Narula N, et al. Anatomical segmentectomy and wedge resections are associated with comparable outcomes for small cT1N0 non-small cell lung cancer. J Thorac Oncol 2016;11:1984-92. [PubMed]
- Gajra A, Newman N, Gamble GP, et al. Effect of number of lymph nodes sampled on outcome in patients with stage I non-small-cell lung cancer. J Clin Oncol 2003;21:1029-34. [PubMed]
- Okada M, Yoshikawa K, Hatta T, et al. Is segmentectomy with lymph node assessment an alternative to lobectomy for non-small cell lung cancer of 2 cm or smaller? Ann Thorac Surg 2001;71:956-60. [PubMed]
- Nishio W, Yoshimura M, Maniwa Y, et al. Re-Assessment of Intentional Extended Segmentectomy for Clinical T1aN0 Non-Small Cell Lung Cancer. Ann Thorac Surg 2016;102:1702-10. [PubMed]


