
Primary mediastinal neoplasms: a report of 1,005 cases from a single institution
Introduction
Mediastinal diseases represent a wide spectrum of lesions benign (neoplastic or non-neoplastic) and malignant, primary and secondary. Primary mediastinal neoplastic diseases are rare but the occurrence of their main types varies in reports depending on the method of analysis and the criteria of inclusion employed by a study. The authors usually concentrate on malignant neoplasms of mediastinum or its certain compartments (anterior, middle or posterior). Sometimes the term “mediastinal tumor” is used interchangeably with “thymic tumor” or “mediastinal neoplasm” but that seems to be an oversimplification (1).
The current one-institutional study was conducted at the National Tuberculosis and Lung Diseases Research Institute (NTLDRI) in Warsaw, a reference center in Poland for lung, pleural and mediastinal diseases. The aim of the study was an epidemiological analysis of primary mediastinal neoplasms (PMNs), benign or malignant (excluding heart and great vessels diseases) diagnosed at NTLDRI in correlation to age and gender of patients and dominant radiological findings. To our knowledge, this is the first such analysis conducted in Poland.
Methods
This was a retrospective study of mediastinal lesions that were analyzed microscopically from 2000 to the end of 2016 at the Department of Pathology of the NTLDRI. The Institute is dedicated to adult patients thus the cohort includes only few pediatric cases that were hospitalized at the NTLDRI. Prior to any surgical intervention mediastinal lesions were evaluated by imaging procedures including computed tomography (CT) and sometimes magnetic resonance imaging (MRI). Resectable tumors were surgically totally removed via sternotomy, thoracotomy or minimally invasive procedure [videothoracoscopic (VATS)]. Samples for histologic examination of inoperative, advanced masses were obtained during mediastinoscopy or ultrasound-guided fine needle aspiration [endobronchial ultrasound-guided transbronchial needle aspiration (EBUS-TBNA); endoscopic ultrasound-guided fine needle aspiration (EUS-FNA)]. Mediastinoscopy with surgical biopsy was also performed in cases when lymphoma was suspected radiologically or in cases of enlarged mediastinal lymph nodes but in the latter indication the procedure has been replaced since 2008 by ultrasound-guided needle aspiration.
In the first part of the study the cases were grouped according to radiological findings that dominated in CT scans of the chest as: mediastinal tumors, lymphadenopathy, cysts and others. Patients operated on due to myasthenia gravis but without evident mediastinal abnormality in radiological examination constituted the last, fifth group in the analysis. However, if the tumor was found on CT scans, the case was included into the group of tumors but the history of myasthenic symptoms was noted. The clinical information about the precise localization of the lesion in the mediastinal compartments and about symptoms other than myasthenic was not available at the time of microscopic examination in most cases.
In the second, main part of the study all results were grouped according to microscopic diagnoses irrespective of radiological images and the epidemiology of PMNs was analyzed statistically. If more than one clinically important histopathological entity was diagnosed in one biopsy sample, all of them were noted, e.g. a case of thymoma with concurrent follicular thymic hyperplasia and reactive lymph nodes was coded as “thymoma” and “hyperplasia”, while reactive lymph nodes were ignored. Reactive lymph nodes were noted if they constituted the only finding in a sample.
The lesions were regarded as “primary” if they originated from the thymus, mediastinal lymph nodes or mediastinal soft tissues. Metastatic lesions or the diseases of the pleura, esophagus, trachea and retrosternal thyroid gland were grouped as “secondary”. Secondary malignancies as well as lesions of uncertain origin (mediastinal or extra-mediastinal) were excluded from further epidemiological study.
The final diagnosis was based on microscopic analysis of the histological or cytological slides routinely fixed, processed and stained with hematoxylin and eosin. Additional histochemical and immunohistochemical tests were performed in all cases where needed. The neoplastic tumors were classified according to the 4th edition of World Health Organization (WHO) classification of tumors of the lung, pleura, thymus and heart [2015]. The diagnoses of older cases that were based on previous histological classifications were updated to the current classification. Thymic carcinomas (TCs) and thymic neuroendocrine tumors (TNETs) were included in one group (TC/TNETs) to simplify the calculations.
The age and gender of the patients were obtained from the institutional database. Each patient was counted once even if they underwent multiple biopsies to establish the final diagnosis unless in this 16-year period of time they were admitted to the hospital several times due to the distinct diseases.
Statistical analysis
A comparison of qualitative variables was done with the chi-squared test (with Yates correction) or with Fisher’s exact if the expected numbers in table were low. To allow for any type of a trend, a correlation between quantitative variable and time was assessed with Spearman rank correlation coefficient. Strength of a relationship was interpreted as follows: |r| ≥0.9 = very strong; 0.7≤ |r| <0.9 = strong; 0.5≤ |r| <0.7 = moderate; 0.3≤ |r| <0.5 = weak; |r| <0.3 = very week (2). The significance level (P) was set at 0.05. All the calculations were done in R package, version 3.4.3.
Results
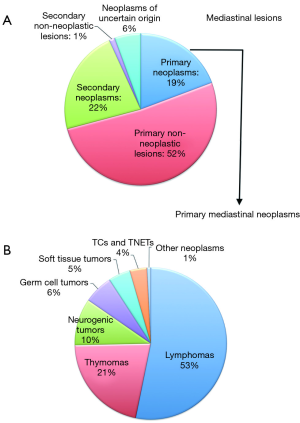
There were 6,263 patients with mediastinal abnormalities registered in the database of the Pathology Department between 2000 and 2016. In 1,155 cases the diagnosis could not be established due to the unrepresentative sample. In the remaining cohort of 5,108 patients, 1,228 had secondary lesions, in 290 patients the diagnosis of neoplasm was established but the organ of origin was uncertain and in 3,590 patients microscopic analysis revealed one or more primary mediastinal lesions (3,691 in total). There were 1,005 neoplasms identified in this cohort and they constituted 19% of all mediastinal disorders.
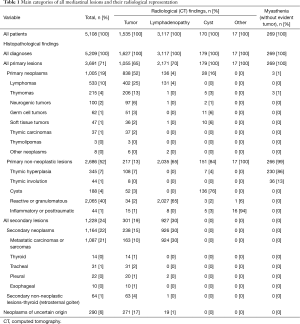
Histopathology vs. radiological findings (Table 1, Figure 1A)
Full table
In the cohort of 5,108 cases with established histopathological diagnosis there were 1,535 (30%) cases described radiologically as ‘tumors’. Much more common were lesions described as ‘mediastinal lymphadenopathy’ that amounted to 61% [3,117] of the cases. The groups ‘cysts’ and ‘others’ constituted 3% [170] and less than 1% [17] of all cases, respectively. Two hundred sixty nine (5%) patients were operated on due to myasthenic symptoms without radiological evidence of significant mediastinal pathology.
Significant majority (1,347, 88%) of mediastinal tumors were of neoplastic origin. Lymphomas (402, 25%) were the most common and were found twice as often than thymomas (206, 13%). Much rare were metastatic carcinomas (usually from the lung and breast) and sarcomas and subsequently tumors of neuronal origin, germ cell tumors (GCTs), soft tissue tumors (STTs) and TC/TNETs. All lesions originated from trachea and the most neoplasms of the retrosternal thyroid gland and esophagus were carcinomas. Pleural lesions that radiologically had the form of a mediastinal tumor microscopically were represented mainly by malignant mesotheliomas and solitary fibrous tumors (both conventional and malignant variants).
The precise localization of the tumors in the mediastinum was only given in 16% [284] of cases—there were 175 and 109 tumors of anterior and posterior compartment, respectively. The most common neoplasms of anterior mediastinum were lymphomas (72, 41%) followed by thymomas (29, 17%), while neurogenic tumors (NTs) (41, 38%) were the most frequent in posterior mediastinum.
In 280 cases of mediastinal tumors microscopic examination revealed non-neoplastic lesions usually thymic hyperplasia, retrosternal goiter or non-neoplastic cysts (usually thymic). Non-neoplastic disorders often accompanied neoplasms but in 12% of all mediastinal lesions described radiologically as ‘tumors’ they constituted the only finding.
Mediastinal lymphadenopathy was usually caused by reactive or granulomatous enlargement of lymph nodes (2,027, 65%). In 924 cases (30%) metastatic carcinomas predominantly from the lung, kidney or breast were found and in 131 cases (4%) the lymphadenopathy was caused by a lymphoma.
Cystic lesions were usually non-neoplastic cysts (136, 80%: thymic, bronchogenic and mesothelial in almost equal numbers) but there were also GCTs (predominantly mature teratomas), STTs (lymphangiomas and hemangiomas), thymomas and NTs (schwannomas).
There was also a small group of 17 cases with non-specific radiological findings, usually inflammatory or posttraumatic, that was named in our study as ‘other lesions’ and was not analyzed in detail.
In the cohort of patients operated on due to myasthenic symptoms without radiologically detected mediastinal tumor [269] microscopic examination revealed non-neoplastic thymic hyperplasia (230, 86%; predominantly follicular), involuted thymus (36, 13%) and in three cases (1%) a thymoma (of type A, B1 and B2B3).
Histopathology vs. epidemiology
In the analyzed cohort there were 3,590 patients with primary mediastinal lesions. A microscopic analysis revealed in this cohort 3,691 distinct histopathological entities including 1,005 neoplasms.
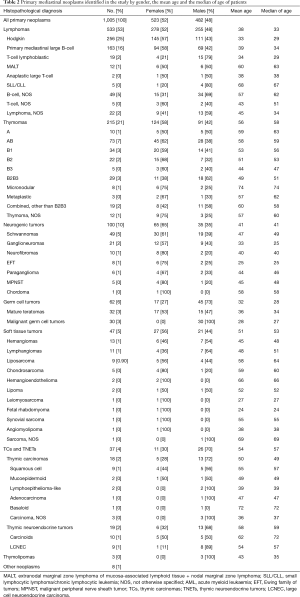
The most common neoplasms were lymphomas with these representing over half of all PMNs that were identified. They were followed by thymomas then neurogenic, germ cell and STTs and TC/TNETs (Figure 1B). All mediastinal neoplasms and their histological subtypes in men and women are presented in Table 2.
Full table
Statistical analysis revealed a significant correlation between the main groups of neoplasms and the gender or age of patients (Table 3). For 10 patients a date of birth was unknown so their age at the moment of diagnosis could not be precisely established. Lymphomas, thymomas and NTs were more prevalent in women whereas TCs/TNETs were far more common in men (P<0.001). Lymphomas were identified most frequently in younger patients, in the 2nd, 3rd and 4th decade of life while thymic epithelial tumors (thymomas and TC/TNETs) were most prevalent between the 6th and 8th decade of life. NTs were found in different age groups with a mean age of 41 years. The highest contribution of these neoplasms (7.98%) was observed in young patients of less than 20 years of age (P<0.001) (Figure 2A).
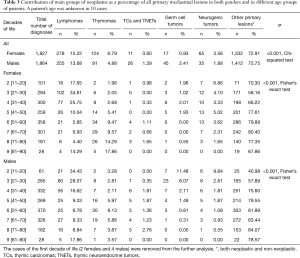
Full table

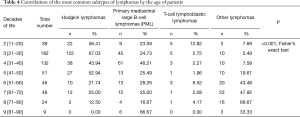
The most frequent subtypes of lymphomas (Table 4, Figure 2B), i.e., classical Hodgkin lymphomas (cHL) and primary mediastinal large B-cell lymphomas (PML), were more common in women and in patients between the 2nd and 4th decade of life. The second peak of occurrence of PML was noted in the population of patients over 80-years of age. Lymphoblastic T-cell lymphomas (T-LBL) were more prevalent in men. Their contribution in the whole group of lymphomas was highest in the 2nd, 6th and 8th decade of life. Due to the small number of nodal and extranodal (thymic) marginal zone lymphomas identified, these cases were grouped together. These lymphomas showed no gender predilection and were most common in the 6th decade of life.
Full table
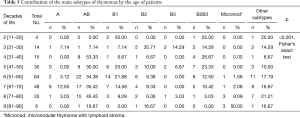
There was no significant correlation between the histological subtypes of thymomas and the gender of patients (P=0.389) whereas a correlation was found between the histology and the age of patients (Table 5). For young patients of less than 30 years of age types B2 and B3 or their combination were prevalent, while type AB was the most common in the 4th and from the 6th to 8th decade of life. Type A was most frequently diagnosed in patients in the 7th decade of life while B1 in the 5th and 6th decade of life. The incidence of micronodular type of thymoma was the highest in the oldest cohort, i.e., over 70-years of age (Figure 2C).
Full table
Thirty percent of patients [64] with thymomas of all histological subtypes except metaplastic thymoma presented myasthenic symptoms. On the other hand, in the whole group of patients with myasthenia gravis, [336] 19% developed thymoma. Neither TC nor TNET was diagnosed in patients with myasthenia. The most common pathology found in this cohort was a non-neoplastic thymic hyperplasia (69%) and in 11% of patients with myasthenia no significant thymic abnormality was diagnosed. In seven hyperplastic or involuted thymuses focal nodular hyperplasia of the thymic epithelium was seen.
In the group of GCTs (62, 6% of PMNs and 1% of all lesions) half of them were malignant and these were noted exclusively in men. Malignant tumors included non-seminomatous GCTs (55, 5% of PMNs) or seminomas (7, 1% of PMNs). In non-seminomatous GCTs yolk sac tumor component was the most often seen (17 cases). GCTs in a form of mature teratomas were diagnosed in almost equal numbers in both genders. Some of these tumors in males were a residual tumor after neoadjuvant chemotherapy of malignant GCTs. In two men a mature teratoma was accompanied by a carcinoid.
The correlation between the histological subtypes of NTs or TC/TNETs and the age and gender of the patients was not statistically significant (P>0.05). NTs were usually benign and they encompassed mainly schwannomas [49], ganglioneuromas [21] and neurofibromas [10]. The most common histological subtype of TCs (18, 2% of PMNs) was squamous cell carcinoma. TNETs (19, 2%) that for statistical purposes were included in one group with the TCs comprised atypical [7] or typical [3] carcinoids and large cell neuroendocrine carcinomas [9].
The group of STTs covered 12 diverse histological types of neoplasms, both benign and malignant. The most frequent ones were histologically benign vascular tumors, hemangiomas (13, 1%) or lymphangiomas (11, 1%). Solitary fibrous tumors (9 cases, 5 conventional and 4 malignant) were rated as pleural tumors and were excluded from further analysis.
In five cases there were two concurrent neoplasms found in the samples obtained from mediastinal lesion: B1B2 thymoma and small lymphocytic lymphoma (SLL), B2B3 thymoma and MALT lymphoma [extranodal marginal zone lymphoma of mucosa-associated lymphoid tissue (MALT)], micronodular thymoma and metastatic large cell neuroendocrine lung carcinoma (a patient presented both mediastinal and lung tumor), B1 thymoma and small cell carcinoma probably of pulmonary origin and neurofibroma with concomitant malignant peripheral nerve sheath tumor.
Discussion
In the Polish National Cancer Registry that is based on the 10th Revision of the International Classification of Diseases (ICD-10) an incidence of malignant neoplasms of intrathoracic organs other than lungs and airways is less than 1 case/100 000/year and they constitute approximately 0.2% of all neoplasms in Poland (3). Even if these numbers are underestimated due to the insufficient completeness of tumors registration in Poland, primary mediastinal cancers are very rare. The Register excludes lymphomas and sarcomas from the neoplasms of mediastinum because they are classified separately independently of the organ of origin (3).
For practical use the current study like others in the literature selected the cases based on their anatomical location rather than ICD-10 codes. A cohort of patients consisted of adults with mediastinal abnormalities found radiologically and diagnosed microscopically in our Institution between 2000 and 2016. We decided not to limit the analysis only to mediastinal “tumors” to avoid omitting neoplasms that on CT scans could have a form of cysts or enlarged lymph nodes.
In a cohort of 5,108 analyzed patients almost half of them developed neoplastic diseases more often secondary, i.e., metastatic or infiltrating the mediastinum from neighboring organs. PMNs constituted 19% of all the lesions identified and the most frequent were lymphomas usually cHLs or PMLs and this is consistent with the observations of some other authors (4-6). Both types dominated in young women but for PML the second highest incidence in patients in the 9th decade of life was noted. T-LBLs, the third type of lymphomas in number were far less numerous than the previous two. T-LBLs are regarded as lymphomas of young men and in our study a clear prevalence in the male gender was also confirmed (7,8). They were most common in the 2nd and 3rd decade of life but occurred in patients of up to 80-years of age. The number of T-LBLs in our study is certainly underestimated because they are frequent mediastinal neoplasm of adolescents who are not a large group of patients in our institution. Other lymphomas were rare, some of them occurred to be a disseminated disease but with the first mediastinal representation. Regardless of histology and the organ of origin (a thymus or lymph nodes) most of lymphomas had radiologically a form of a ‘tumor’. On microscopic examination a definitive organ of origin could rarely be established due to the diffuse neoplastic infiltration destroying mediastinal tissues.
Thymic epithelial tumors, i.e., thymomas, TCs and TNETs accounted in our study for one-quarter of all PMNs and were twice less common than lymphomas. We analyzed thymomas and TC/TNETs separately to compare their epidemiology. Thymomas were most prevalent in women in the 6th–8th decades of life, while TCs were six times rarer and were usually seen in men of similar age. The prevalence of thymomas in females is remarkable since no gender predilection is usually reported in the literature (9,10). Low-grade histological subtypes of thymomas, i.e., A and AB occurred more often in the 6th–7th decades of life. The more aggressive subtypes, B2, B3 and B2B3 were more common in younger patients and the mean patients’ age for these tumors ranged between 44 and 51 years. Moreover, these subtypes were more prevalent in patients under 30 years of age. Our results correspond with the literature (11,12). Micronodular thymomas with lymphoid stroma (MNTs) in our study were not infrequently a minor component of conventional thymomas, usually A or AB and in these combined tumors micronodular component was ignored in further analysis. Of interest, MNTs in a pure or distinctly predominant form were found in the oldest group of patients (8th–9th decade of life) as well as they represented prevalent thymoma subtype in patients over 80 years of age. Other authors reported MNTs in younger patients with a mean age of around 60 but some researchers jointed both pure and combined MNTs in one group (13,14). MNT is not unequivocally regarded as malignant neoplasm due to the lack of documented cases of metastases, recurrences or disease-related deaths (9,15,16). Considering our results we assume that MNTs may be true malignant tumors but they may have long clinical course and a progression may not be disclosed before the death of the patient by another cause.
Of note, five cases of two simultaneous neoplasms were found in the cohort and four of them concerned thymomas. Two cases were resected tumors composed of thymomas with admixed lymphomas (SLL and MALT lymphoma) that involved not only thymus but also other resected structures as lymph nodes or lung. In both cases clinicians did not expect lymphomas before surgery. One of these cases was published previously as a case report (17). The next two cases revealed the coexistence of thymomas and lung carcinomas. In both cases patients had established or suspected advance lung tumors and biopsies were performed to confirm the metastases of carcinomas and the thymomas were found accidentally. Thymoma patients have an increased risk of developing second malignancies especially non-Hodgkin lymphomas (10,18). The results of our study are promising but cannot confirm this opinion since our data is limited only to the mediastinal malignancies found simultaneously in samples obtained during the same procedure.
TCs [18] and neuroendocrine tumors [19] were six times rarer than thymomas and represented concomitantly only 37 cases (4% of PMNs). To differentiate between primary TC/TNETs and metastatic cancers from other organs mainly from the lung in small samples obtained by mediastinoscopy or FNA was the most severe difficulty in current study and it is a constant problem in a routine microscopic diagnostics of mediastinal lesions. Although an immunohistochemical tests were performed in all cases where needed and the amount of tissue was sufficient, in 290 cases determining the exact organ of origin of a carcinoma was impossible. These cases were excluded from the epidemiological analysis and thus the total number of TCs and TNETs may be underestimated. In our study TCs and TNETs consisted of 7% and 8% of all thymic epithelial tumors, respectively and for 2% of PMNs each. In the database of the International Thymic Malignancy Interest Group (ITMIG) a contribution of TCs in all thymic tumors were twice higher (19). In our study TCs were more common in men with a mean age of 50 years and a squamous cell carcinoma was the most frequent histological subtype and this is in concordance with the observations of other authors (19). The TNETs in our analysis showed greater contribution in thymic tumors (8%) than reported in the literature (~5%) (20,21). Large cell neuroendocrine carcinomas showed strong male predominance while carcinoids occurred in equal numbers in both genders. This contrasts with previous studies that presented reverse results (16,22). One hundred sixty five small cell carcinomas were found in the current study (data not shown), but in no cases a thymic origin could not be definitely confirmed. In the literature small cell carcinomas constitute approximately 10% of all TNETs (16).
In the current study 30% of thymomas and none of TC/TNETs were accompanied by myasthenia gravis. Padda et al. in the analysis of a database for thymic tumors of the ITMIG found myasthenia in 2% of TCs and 0.2% of TNETs (23). In three patients operated on due to the myasthenia without significant radiological abnormalities of the mediastinum microscopic evaluation revealed thymomas of types A, B1 and B2B3. Sometimes authors report in such cases so called “microscopic thymomas”—focal or multifocal proliferation of thymic epithelial cells of less than 0.1 cm in diameter with unknown clinical significance and unproven relationship with conventional thymomas (16,24). In our routine practice we avoid using this misleading term not to burden a patient with the diagnosis of malignant neoplasm. The WHO classification [2015] proposes a synonym ‘nodular hyperplasia of the thymic epithelium’ that we prefer to use (16). In the current study seven such cases were found in macroscopically unchanged myasthenic thymuses.
Mediastinal germ cells tumors were infrequent in the current study and only 62 cases (6% of PMNs and 1% of all lesions) were found. Mature teratomas occurred in approximately equal number in patients of both genders with an average age of 36. There were 17 women with GCT and all the tumors found in females were benign mature teratomas. Moran et al. in their analysis of 322 primary mediastinal tumors noted GCTs only in two women and both tumors were teratomas with malignant component (25). Takeda et al. found one female patient with seminoma and one with embryonal carcinoma in a cohort of 129 patients with GCTs; Coskun et al. described a case of mediastinal yolk sac tumor in a 66-year-old woman (26,27). In our cohort malignant forms of GCTs, usually non-seminomatous GCTs were noted exclusively in men of a mean age 28 years and the patients often underwent chemotherapy prior to surgery of residual tumor. Of note, the most common component of non-seminomatous GCTs was yolk sac tumor (as a pure form or as a component of mixed GCT) that we found in nearly 31% of these tumors and this incidence was much higher than the occurrence observed by Takeda at al. (10%) but not as high as the number mentioned by Moran et al. (73%) (25,26). Other histological subtypes were rarely detected in our study this is possibly because they occurred to be more sensitive to neoadjuvant chemotherapy and necrotized before surgical removal of a residual tumor.
Another group of mediastinal neoplasms in this study comprised of NTs, usually benign, i.e., schwannomas, ganglioneuromas and neurofibromas. These predominated in women with an average age of 41. The largest contribution of these tumors in PMNs was observed in patients in the 2nd decade of life. NTs are one of the most important neoplasms in infants and children and in this cohort they are often malignant (16,28). In our study based on an adults’ population malignant NTs were from the Ewing family of tumors and malignant peripheral nerve sheath tumors and we found only 8 and 5 cases of these sarcomas, respectively. NTs were the third PMNs after thymic and mesenchymal lesions among adults in a study of Liu et al. and the commonest lesion in pediatric population (29). A Chinese study found that NTs accounted for 7.7% of all mediastinal lesions in adults (29). In our analysis they constituted 6% of mediastinal tumors and only 2% if all mediastinal lesions including cysts and lymphadenopathy were considered.
The majority of STTs in the current study (47, 5% of PMNs) were histologically benign vascular neoplasms, i.e., hemangiomas (13, 1%) and lymphangiomas (11, 1%). Vascular tumors had a form of uni- or multifocal proliferations radiologically often described as cysts. They showed slight male predominance and mean age of patients reached 45–48 years. In other studies benign vascular tumors usually appeared in younger patients with an average age approximately 35 years. Mediastinal lymphangiomas showed female prevalence, while hemangiomas were slightly more frequent in men (30,31). Liposarcomas were the most common mediastinal sarcomas in our analysis (9, 0.9%). They occurred mostly around 60 years of age and showed no gender predilection and this is in concordance with the literature (5,29).
The limitation of current study was a lack of clinical information about the detailed location of lesions in mediastinal compartments (anterior, middle or posterior) in most cases. Awareness of topographic site of a lesion and anatomy of mediastinum enables a pathologist to narrow a differential diagnosis to the most probable one. Thymus, fat tissue and lymph nodes are major content of an anterior (prevascular) compartment; trachea, esophagus, lymph nodes, heart and great vessels occupy middle (visceral) part whereas posterior (paravertebral) space contains paravertebral soft tissues (32). The most common neoplasms of anterior mediastinum are usually thymomas whereas NTs are more prevalent in posterior compartment (4,8). Information about the specific location in the mediastinum was only given in 16% of cases in our study and we found that the anterior mediastinum was the most frequent location for lymphomas (41%) followed by thymomas (17%), while NTs (38%) were the most frequent in the posterior mediastinum. However, our results may be burdened by error due to the unrepresentative sample.
Other limitations such as the cohort being limited practically only to adult patients and the exclusion of heart and great vessel diseases were dependent on the specificity of our institution.
One thousand five PMNs were found in the current study and they represented 27% of primary mediastinal disorders and 19% of all mediastinal lesions. Most of the PMNs (841/1,005) were radiologically defined as a ‘tumor’ but 14% cases, usually lymphomas had a form of enlarged lymph nodes and 3% (GCTs, STTs, thymomas and NTs) of cysts. Limiting the study inclusion criteria to ‘tumors’ we would have omitted such cases. It is obvious that a term ‘mediastinal tumor’ cannot be used interchangeably with ‘mediastinal neoplasm’—our analysis showed that 12% of tumors occurred ultimately to be non-neoplastic disorders, e.g., hyperplastic thymus, cyst filled with fluid, retrosternal goiter or a conglomerate of reactive lymph nodes. A comparative analysis of the occurrences of individual mediastinal lesions with the literature is very difficult due to the different study inclusion criteria used by researchers. Some authors analyzed both neoplastic and non-neoplastic lesions as we did while others concentrated only on malignant neoplasms. Sometimes all lesions were included in a study independently of the surgical procedure of obtaining the sample similarly to our analysis but there are studies based only on resected tumors. There are even studies that selected the cases without microscopic verification (4-6,29,33). Mediastinal lymphadenopathy was usually not analyzed, however we decided to include it to have the whole spectrum of mediastinal diseases due to the reasons mentioned earlier.
In conclusion, the most relevant results of our study were: (I) lymphomas were the most frequent primary mediastinal tumors; (II) thymomas were most prevalent in women in the 6th–8th decades of life, while TCs were usually seen in men of similar age; (III) micronodular thymomas with lymphoid stroma predominated in the oldest group of all thymoma patients (>70 years of age); (IV) malignant GCTs were found exclusively in males; (V) NTs predominated in women of middle age. PMNs are rare conditions thus they may pose a problem in microscopic diagnostics that always must include in differentiation other more often lesions both malignant and benign. Awareness of basic epidemiology, incidence and radiological findings may be very helpful for pathologist to conduct the diagnosis in the proper direction.
Acknowledgments
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: According to the national and institutional laws this study did not require any ethical committee approval since a methodology was based on routine diagnostic procedures. An informed patient’s consent for any diagnostic procedure was obtained in an each individual case. All data for statistical analysis were handled anonymously.
References
- Müller-Hermelink HK, Engel P, Kuo TT, et al. Tumours of the Thymus. In: Travis WD, Brambilla E, Muller-Hermelink HK, et al. editors. WHO Classification of Tumours. Pathology and Genetics. Tumours of the Lung, Pleura, Thymus and Heart. Lyon: IARC Press, 2004:145-248.
- Hinkle DE, Wiersma W, Jurs SG. Applied Statistics for the Behavioral Sciences. 5th ed. Boston: Houghton Mifflin, 2003.
- Didkowska J, Wojciechowska U, Olasek P. Cancer in Poland in 2015. Polish National Cancer Registry Department of Epidemiology and Cancer Prevention, Warsaw, 2017.
- Aroor AR, Prakasha SR, Seshadri S, et al. A study of clinical characteristics of mediastinal mass. J Clin Diagn Res 2014;8:77-80. [PubMed]
- Vaziri M, Pazooki A, Zahedi-Shoolami L. Mediastinal Masses: Review of 105 Cases. Acta Medica Iranica 2009;47:297-300.
- Temes R, Chavez T, Mapel D, et al. Primary Mediastinal Malignancies: Findings in 219 Patients. West J Med 1999;170:161-6. [PubMed]
- Medeiros LJ. Diagnostic Pathology: Lymph Nodes and Spleen with Extranodal Lymphomas 1st ed. Canada: Lippincott Wiliams and Wilkins, 2011.
- Maeshima AM, Taniguchi H, Suzuki T, et al. Distribution of malignant lymphomas in the anterior mediastinum: a single-institution study of 76 cases in Japan, 1997-2016. Int J Hematol 2017;106:675-80. [Crossref] [PubMed]
- Marx A, Weis CA, Ströbel P. Thymome. Pathologe 2016;37:412-24. [Crossref] [PubMed]
- Engels EA. Epidemiology of thymoma and associated malignancies. J Thorac Oncol 2010;5:S260-5. [Crossref] [PubMed]
- Zhu L, Zhang J, Marx A, et al. Clinicopathological analysis of 241 thymic epithelial tumors— experience in the Shanghai Chest Hospital from 1997–2004. J Thorac Dis 2016;8:718-26. [Crossref] [PubMed]
- Okumura M, Ohta M, Tateyama H, et al. The World Health Organization histologic classification system reflects the oncologic behavior of thymoma: a clinical study of 273 patients. Cancer 2002;94:624-32. [Crossref] [PubMed]
- Mneimneh WS, Gökmen-Polar Y, Kesler KA, et al. Micronodular thymic neoplasms: case series and literature review with emphasis on the spectrum of differentiation. Mod Pathol 2015;28:1415-27. [Crossref] [PubMed]
- Suster S, Moran CA. Micronodular thymoma with lymphoid B-cell hyperplasia: clinicopathologic and immunohistochemical study of eighteen cases of a distinctive morphologic variant of thymic epithelial neoplasm. Am J Surg Pathol 1999;23:955-62. [Crossref] [PubMed]
- Burke AP, Aubry MC, Malaszewski JJ, et al. Practical Thoracic Pathology: Diseases of the Lung, Heart and Thymus 1st ed. Philadelphia: Wolters Kluwer, 2017.
- Travis WD, Brambilla E, Burke AP, et al. WHO classification of Tumours of the Lung, Pleura, Thymus and Heart. 4th ed. Lyon: IARC, 2015.
- Szolkowska M, Langfort R, Winiarski S, et al. Two neoplasms rich in small lymphocytes, B1B2 thymoma and small lymphocytic lymphoma, intermingled in one tumor mass. A case report. Pol J Pathol 2017;68:75-81. [Crossref] [PubMed]
- Engels EA, Pfeiffer RM. Malignant thymoma in the United States: demographic patterns in incidence and associations with subsequent malignancies. Int J Cancer 2003;105:546-51. [Crossref] [PubMed]
- Ahmad U, Yao X, Detterbeck F, et al. Thymic carcinoma outcomes and prognosis: results of an international analysis. J Thorac Cardiovasc Surg 2015;149:95-100, 101.e1-2.
- Öberg K, Hellman P, Ferolla P, et al. Neuroendocrine bronchial and thymic tumors: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann Oncol 2012;23 Suppl 7:vii120-3. [PubMed]
- Suster S, Moran CA. Diagnostic Pathology: Thoracic 2nd ed. Philadelphia: Elsevier, 2017.
- Soga J, Yakuwa Y, Osaka M. Evaluation of 342 cases of mediastinal/thymic carcinoids collected from literature: a comparative study between typical carcinoids and atypical varieties. Ann Thorac Cardiovasc Surg 1999;5:285-92. [PubMed]
- Padda SK, Yao X, Antonicelli A, et al. Paraneoplastic Syndromes and Thymic Malignancies: An Examination of the International Thymic Malignancy Interest Group Retrospective Database. J Thorac Oncol 2018;13:436-46. [Crossref] [PubMed]
- Fukuhara M, Higuchi M, Owada Y, et al. Clinical and pathological aspects of microscopic thymoma with myasthenia gravis and review of published reports. J Thorac Dis 2017;9:1592-7. [Crossref] [PubMed]
- Moran CA, Suster S. Primary germ cell tumors of the mediastinum: I. Analysis of 322 cases with special emphasis on teratomatous lesions and a proposal for histopathologic classification and clinical staging. Cancer 1997;80:681-90. [Crossref] [PubMed]
- Takeda S, Miyoshi S, Ohta M, et al. Primary germ cell tumors in the mediastinum: a 50-year experience at a single Japanese institution. Cancer 2003;97:367-76. [Crossref] [PubMed]
- Coskun U, Günel N, Yildirim Y, et al. Primary mediastinal yolk sac tumor in a 66-year-old woman. Med Princ Pract 2002;11:218-20. [Crossref] [PubMed]
- Bicakcioglu P, Demirag F, Yazicioglu A, et al. Intrathoracic neurogenic tumors. Thorac Cardiovasc Surg 2014;62:147-52. [PubMed]
- Liu T, Al-Kzayer LFY, Xie X, et al. Mediastinal lesions across the age spectrum: a clinicopathological comparison between pediatric and adult patients. Oncotarget 2017;8:59845-53. [PubMed]
- Park JG, Aubry MC, Godfrey JA, et al. Mediastinal lymphangioma: Mayo Clinic experience of 25 cases. Mayo Clin Proc 2006;81:1197-203. [Crossref] [PubMed]
- Moran CA, Suster S. Mediastinal hemangiomas: a study of 18 cases with emphasis on the spectrum of morphological features. Hum Pathol 1995;26:416-21. [Crossref] [PubMed]
- Carter BW, Tomiyama N, Bhora FY, et al. A modern definition of mediastinal compartments. J Thorac Oncol 2014;9:S97-101. [Crossref] [PubMed]
- Dubashi B, Cyriac S, Tenali SG. Clinicopathological analysis and outcome of primary mediastinal malignancies - A report of 91 cases from a single institute. Ann Thorac Med 2009;4:140-2. [Crossref] [PubMed]


