
Clinical characteristics and economic burden of tuberculous-destroyed lung in Korea: a National Health Insurance Service-National Sample Cohort-based study
Introduction
The incidence of tuberculous (TB) in Korea was 25–99/100,000 people in 2016 (1), which is relatively high compared to Western countries (2). TB is a risk factor for chronic obstructive pulmonary disease (COPD) because bronchiectasis and airflow limitations are caused by endobronchial involvement and destruction of lung parenchyma (3). Tuberculous-destroyed lung (TDL) defines patients who have extensive parenchymal destruction after a pulmonary TB infection with or without anti-TB treatment (4-6).
The definition and clinical characteristics of TDL patients have been studied since early 19th century, for recent 20 years. TDL can cause a progressive decline in lung function with frequent exacerbations (4,5,7). Korean multicenter retrospective studies showed that TDL patients had experienced acute exacerbations 0.4 times per year and the frequency of acute exacerbations were correlated with the severity of the airflow limitation, and pulmonary function was negatively correlated with the number of lobes involved (5,8). These retrospective studies have revealed the negative effects of TDL on lung function and patient prognosis as an independent respiratory disease from COPD. About the treatment of TDL, a multicenter double-blind clinical trial was recently published in patients with TDL receiving inhaled indacaterol. That study revealed that inhaled indacaterol provides significant symptom and lung function improvement (6). An inhaled bronchodilator benefits patients diagnosed not only with COPD but also TDL. However, little is known about the current status of physicians’ prescriptions and the economic burden of patients with TDL. In order to detect and appropriately treat TDL patients, we designed a clinical study using nationwide database system.
This study evaluated the baseline characteristics, healthcare utilization, and costs of patients diagnosed TDL in Korea for 5 years using Health Insurance Review and Assessment Service (HIRA) data. Globally, this is the first large-scale report showing the nationwide social economic burden of TDL.
Methods
Study population and design
We used a dataset provided by HIRA corresponding to approximately 51 million subjects with national claims data from nearly the entire Korean population. Korea is compulsorily covered by medical insurance, 98% of the total population are covered and 99% of claims are electronically submitted by healthcare service providers. The changes of missing claims are highly unlikely (9). The healthcare system in Korea has two components, health insurance and medical aid. The national health insurance system provides coverage to all citizens and medical aid component provides support to lower income groups (10). HIRA research data consists of 6 files: (I) general information file; (II) healthcare services file including inpatient prescription; (III) the diagnosis file; (IV) the outpatient prescription file; (V) the drug master file; and (VI) the provider information file (9). Disease diagnoses held in the general information file are coded based on the International Codes of Disease 10th Edition Clinical Modification (ICD-10-CM). We searched the database to identify patients diagnosed with TDL using ICD codes B90 and J984 for the period from January 01, 2011 to December 31, 2015. Patients who had the ICD code for TDL as the primary to fifth sub-diagnosis among patients aged >40 years old were included. The cohort database included age, sex, insurance type (health insurance and medical aid), comorbidities, drug prescription data (drug name and rate of prescription), billing code, and healthcare services provided to beneficiaries such as procedures, diagnostic tests, treatment, and inpatient prescriptions. The provider information file carries information about healthcare providers such as the provider ID; practice location; provider type (i.e., primary, secondary, or tertiary); the number of beds; and inception date of institution (9). We collected and retrospectively analyzed 5 years of drug prescription and healthcare visit claims data from 2011 to 2015. Days of healthcare use were analyzed separately according to outpatient and inpatient services. Days of outpatient service utilization were analyzed only for patients who used such a service. Days of inpatient service utilization were analyzed only for patients who used an inpatient service, including the emergency room (ER) or intensive care unit (ICU). The total number of days utilizing healthcare were analyzed for all patients who used outpatient or inpatient services. Percentage of TDL patients who took any of respiratory drugs at least one time during the study period was calculated. Frequencies of medication prescriptions were expressed as a percentage of the patients who had prescribed each drug at least one time in the total number of TDL patients (allowed duplication). Moreover, costs for healthcare utilization and respiratory medications were analyzed with the billing code and rate of prescription in Korean won (KRW) and converted into US dollars (USD) according to the exchange rate ($1 USD =1,126 KRW) on November 20, 2018.
Statistical analyses
All statistical analyses were performed using SAS version 9.2 (SAS Institute, Cary, NC, USA). Results are expressed as mean ± standard deviation for continuous variables and proportions for categorical variables.
Ethics statement
To protect the patients’ information and identity, all patients received an anonymous identification code in the HIRA sample data. The authors could not identify any patients included in the sample data. This study was approved by the Institutional Review Board of Seoul St. Mary’s Hospital, which waived the requirement for informed consent (KC18ZESE0458).
Results
Baseline characteristics
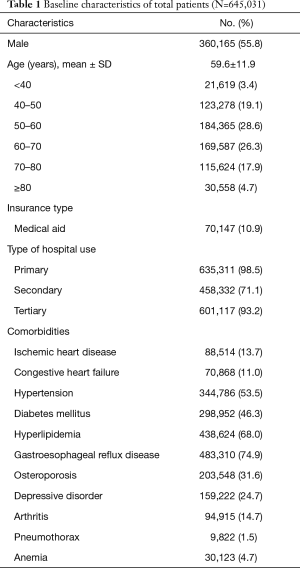
Table 1 shows the baseline characteristics of all included patients. In total, 645,031 patients were diagnosed with TDL over the 5 years. Among them, 55.8% were male, the mean age was 59.6±11.9 years old, and the most common age group was 50–60 s. About 11% of the patients received medical aid. During the study period, 98.5% of the patients used primary care hospitals, 71.1% used secondary hospitals, and 93.2% used tertiary hospitals. The comorbid medical diseases are summarized in Table 1, showing that gastroesophageal reflux disease (74.9%), hyperlipidemia (68.0%), and hypertension (53.5%) were the most common. In addition, diabetes mellitus was found in 46.3% of the patients and cardiovascular comorbidities, such as ischemic heart disease (13.7%) or congestive heart failure (11.0%), were also included.
Full table
Healthcare utilization
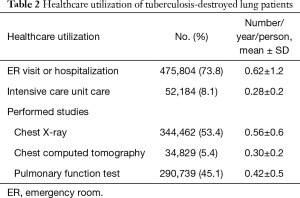
The frequencies of healthcare utilization are presented in Table 2, and expended costs and service days are included in Tables 3,4. During the study period, 475,804 (73.8%) patients visited the ER or were hospitalized. Annual frequencies of ER visits or hospital admissions were 0.62±1.2 per person. About 8.1% (0.28±0.2 times/year/person) of patients were admitted to the ICU. Patients diagnosed with TDL had received 0.56±0.6 chest X-rays, 0.30±0.2 chest computed tomography (CT) scans, and 0.42±0.5 pulmonary function test (PFT)s per person annually.
Full table
Full table
Full table
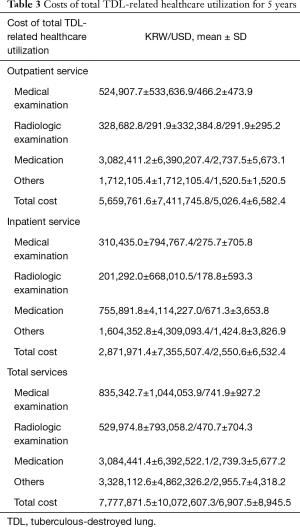
The summarized costs for healthcare utilization are shown in Table 3. Total cost per person during the 5-year study period was >$6,907 USD; half ($2,739 USD) was expended for medications, 10% for medical examinations, and 7% for radiological examinations. When these costs were divided according to whether they were inpatient or outpatient services, the costs for outpatient services were twice as much as those for inpatient services (5,026 vs. 2,550 USD) over the 5 years.
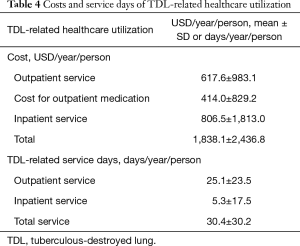
Analysis results for the annual cost and service days for TDL-related healthcare utilization per person are shown in Table 4. Patients diagnosed with TDL received services for about 30.4±30.2 days per year, and 25 days were in the outpatient clinic. Annual total costs were $1,838 USD per person, $806 USD for inpatient services, $617 USD for outpatient services, and $414 USD for outpatient medications. Forty-three percentage of the annual costs analyzed individually were expended for inpatient services.
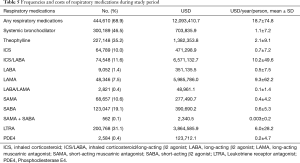
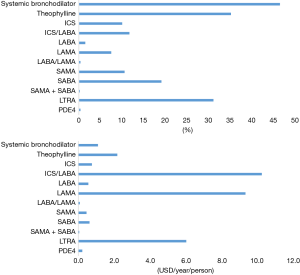
Table 5 and Figure 1 show the frequencies and costs of respiratory medications during the study period. A total of 68.9% of the patients were prescribed respiratory medications and $12 million USD ($18 USD per person annually) were paid for the medications. The most frequently prescribed medications were oral systemic bronchodilators (46.5%) and methylxanthine (35.2%). The most frequently prescribed inhalers were short-acting β2 agonists (19.1%). An inhaled corticosteroid (ICS)/long-acting β2 agonist (LABA) combination was used in 11.6%, and ICS only in 10.0%, of patients. Long-acting muscarinic antagonists (LAMAs) and LABAs were used in 7.5% and 1.4%, individually. Annual cost per person was highest for ICS/LABA ($10 USD) and LAMA ($9 USD).
Full table
Discussion
This is the first large-scale study showing the economic burden of patients with TDL using a nationwide database. Patients with TDL were admitted to the hospital 0.6 times including 0.28 times per person annually for ICU care. The total costs for 5 years were mainly produced by outpatient services, which were larger than those for inpatient services including medication prescription and medical or radiological examinations. Among the total 30 days of TDL-related services, 5 days were spent for inpatient services, 1/5 of outpatient service per person annually. That is, 5-day individual cost per month for inpatient services made 43% of the total costs. In addition, 68.9% of the patients had been prescribed respiratory medications for TDL. Oral bronchodilators and methylxanthine were favored rather than inhaled bronchodilators and corticosteroids.
The first description of destroyed lung after pulmonary TB was in the 1960s, but TDL only began to be analyzed in the early 2000s. Lee et al. reported a decline in lung function with chronic airflow obstruction (CAO) due to TDL in 2003 (4). They compared 21 patients with CAO and parenchymal damage in more than one-half of one lung to 11 patients with COPD. PFTs showed that patients with CAO had a lower forced vital capacity (FVC) and post-bronchodilator forced expiratory volume for 1 s (FEV1) than those with COPD. Patients with CAO who wheezed were more responsive to a bronchodilator than those who did not. Patients with TDL could have a CAO pathophysiology that is different from that of COPD, and bronchodilator therapy may be useful for treating CAO.
A large-scale retrospective review of clinical and radiographic findings of TDL was conducted in 2012, including 169 patients followed for 15 years from a single tertiary center (7). The authors found a median of 1 (range, 0–11) hospitalization during the median 31-month follow-up period. The clinical respiratory events were pneumonia (56.8%), hemoptysis (21.9%), and spontaneous pneumothorax (14.2%). Overall mortality was 27.8% with a median survival duration of 39 (range, 0–176) months. About 60% of patients had been prescribed respiratory medications, 46% used inhaled anticholinergic drugs, and 40% used oral methylxanthine. The prognostic factor contributing to mortality associated with TDL was a field score >3, denoting a percentage of parenchymal injured lung area >51% (P=0.004).
Rhee et al. studied 595 patients with TDL from 21 university hospitals in Korea over 6 years and reported that 76.8% of the patients had an airflow obstruction (FEV1/FVC <0.7) with 0.4 exacerbations per year (5). Interestingly, the number of annual exacerbations in patients with TDL was similar to those in patients with COPD (0.4±0.05 vs. 0.32±0.03, P=0.062); however, the rates of LAMA or LABA/ICS prescriptions were significantly lower in patients with TDL compared to those with COPD (LAMA 50.0% vs. 73.9%, P<0.001, ICS/LABA 45% vs. 84.2%, P<0.001). Based on this large-scale review of patients with TDL, physicians recognized that these patients had a poor prognosis with acute exacerbations similar to COPD. Moreover, despite the effects of airflow obstruction on the mortality rate of patients with TDL, airflow obstruction is under-recognized and less often treated with long-acting inhaled bronchodilators.
The clinical significance of inhaled bronchodilators for treating TDL was shown in a retrospective study (11) and a multicenter double-blind clinical trial (6). In the latter study, after a 2-month treatment, inhaled tiotropium led to a >10% improvement in FEV1; inhaled indacaterol increased FEV1 by 150 mL and controlled symptoms. More than half of patients with TDL have airflow obstructions and use of long-acting bronchodilators benefits lung function and symptom control. Although the positive effect of bronchodilator use in TDL patients has been shown recently in this multicenter double-blind clinical trial, prescription rates of the LAMA or LABA were remarkably low (7.5%, 1.4% respectively) in our study result. Clinical guidelines should be established to treat airflow obstruction in TDL patients.
In a global report published in 2016, direct costs for respiratory diseases made up approximately 6% of the total €800 billion healthcare budget of the European Union. The four major respiratory diseases, including COPD, asthma, pneumonia, and TB, had costs totaling €38.7, €17.7, €10.1, and €2.1 billion, respectively (12). In Korea, the mean annual cost for patients with respiratory disease was estimated to be $8,853 per patient in 2012. The estimated percentages of each ailment among the 999 enrolled patients were of 5.6% for COPD, 31.8% for asthma, 55.7% for allergic rhinitis, and 6.9% for rhinosinusitis (13). Based on these results, the total annual costs of $1,838 USD per person by patients with TDL in our study seem low (about 20% of $8,853 USD) compared to those in patients with a respiratory disease. However, because TDL had not been defined in that study, it is possible that TDL patients could be missed or included as COPD or asthma. The economic burden of TDL would increase if underdiagnosed patients with TDL are re-assessed.
TDL is a chronic lung disease and the most important factors determining the economic and social costs are disease severity, the presence of acute exacerbations, and comorbidities (14). The predominant healthcare cost item in a COPD cohort was hospitalization for exacerbations, which is associated with patient mortality (15). Our data also showed that most patients with TDL had comorbidities that needed to be treated and half of the annual costs were used for inpatient services, although the number of inpatient days was only 20% of the number of outpatient days. Interventions to prevent acute disease exacerbations and progression of comorbid conditions should be accompanied to alleviate the clinical and economic burden of TDL. Moreover, it is necessary to raise awareness of disease incidents, perform early diagnosis and disease control mediated by active treatment using bronchodilators.
This study has provided the first description of the nationwide TDL burden in Korea using HIRA data. Because South Korea has provided national medical health care services since 1989, HIRA data contain almost all of the claims data. Patients enrolled in our study represented the nationwide population of South Korea. The indirect costs for disability should be included because loss of productivity contributes to a significantly larger burden of disease than direct medical costs (13,16). As patients with COPD have different economic burdens on the healthcare system in Korea depending on disease severity (17), the healthcare burden of TDL should also be discussed in later research depending on disease severity. Moreover, HIRA data have limitations because of its nature, retrospective claims data. As the claims data are generated to reimburse healthcare services eligible for coverage, discrepancies occur between diagnosis entered in the data and diseases that a patient has in reality (9). Patients registered with ICD 10 codes could be over or underdiagnosed and make a bias. Lack of patients’ clinical characteristics such as socioeconomic status and absence of control group could also be the limitation of this study.
Conclusions
TDL imposes a high medical economic burden. These economic costs were primarily made up of inpatient services and costs for prescribed medications, which were higher than those for medical or radiological examinations. Physicians in Korea mainly use oral bronchodilators or methylxanthine rather than inhaled long-acting bronchodilators. The treatment guidelines and definition of TDL disease should be established to prevent utilization of healthcare and to lower the economic burden of TDL.
Acknowledgments
Funding: This study was supported by a grant of the Ministry of Health and Welfare, Republic of Korea (Grant No. HC16C-2254-010017).
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: This study was approved by the Institutional Review Board of Seoul St. Mary’s Hospital, which waived the requirement for informed consent (KC18ZESE0458).
References
- Kim JK, Jeong I, Lee JY, et al. Tuberculosis Relief Belt Supporting Project (Tuberculosis Patient Management Project for Poverty Group). Tuberc Respir Dis (Seoul) 2018;81:241-6. [Crossref] [PubMed]
- Kim JH, Yim JJ. Achievements in and Challenges of Tuberculosis Control in South Korea. Emerg Infect Dis 2015;21:1913-20. [Crossref] [PubMed]
- Jordan TS, Spencer EM, Davies P. Tuberculosis, bronchiectasis and chronic airflow obstruction. Respirology 2010;15:623-8. [Crossref] [PubMed]
- Lee JH, Chang JH. Lung function in patients with chronic airflow obstruction due to tuberculous destroyed lung. Respir Med 2003;97:1237-42. [Crossref] [PubMed]
- Rhee CK, Yoo KH, Lee JH, et al. Clinical characteristics of patients with tuberculosis-destroyed lung. Int J Tuberc Lung Dis 2013;17:67-75. [Crossref] [PubMed]
- Kim CJ, Yoon HK, Park MJ, et al. Inhaled indacaterol for the treatment of COPD patients with destroyed lung by tuberculosis and moderate-to-severe airflow limitation: results from the randomized INFINITY study. Int J Chron Obstruct Pulmon Dis 2017;12:1589-96. [Crossref] [PubMed]
- Ryu YJ, Lee JH, Chun EM, et al. Clinical outcomes and prognostic factors in patients with tuberculous destroyed lung. Int J Tuberc Lung Dis 2011;15:246-50. i. [PubMed]
- Kim SJ, Lee J, Park YS, et al. Effect of airflow limitation on acute exacerbations in patients with destroyed lungs by tuberculosis. J Korean Med Sci 2015;30:737-42. [Crossref] [PubMed]
- Kim JA, Yoon S, Kim LY, et al. Towards Actualizing the Value Potential of Korea Health Insurance Review and Assessment (HIRA) Data as a Resource for Health Research: Strengths, Limitations, Applications, and Strategies for Optimal Use of HIRA Data. J Korean Med Sci 2017;32:718-28. [Crossref] [PubMed]
- Health Insurance review and assessment service. Available online: http://www.hira.or.kr
- Yum HK, Park IN. Effect of inhaled tiotropium on spirometric parameters in patients with tuberculous destroyed lung. Tuberc Respir Dis (Seoul) 2014;77:167-71. [Crossref] [PubMed]
- López-Campos JL, Tan W, Soriano JB. Global burden of COPD. Respirology 2016;21:14-23. [Crossref] [PubMed]
- Yoo KH, Ahn HR, Park JK, et al. Burden of Respiratory Disease in Korea: An Observational Study on Allergic Rhinitis, Asthma, COPD, and Rhinosinusitis. Allergy Asthma Immunol Res 2016;8:527-34. [Crossref] [PubMed]
- Kim WY, Kim MH, Jo EJ, et al. Predicting Mortality in Patients with Tuberculous Destroyed Lung Receiving Mechanical Ventilation. Tuberc Respir Dis (Seoul) 2018;81:247-55. [Crossref] [PubMed]
- Anzueto A, Sethi S, Martinez FJ. Exacerbations of chronic obstructive pulmonary disease. Proc Am Thorac Soc 2007;4:554-64. [Crossref] [PubMed]
- Tang YM, Liu XN, Zhang QJ, et al. Chronic obstructive pulmonary disease deaths, disability-adjusted life years, and risk factors in Hubei province of mid-China, 1990-2015: the Global Burden of Disease Study 2015. Public Health 2018;161:12-9. [Crossref] [PubMed]
- Kim J, Rhee CK, Yoo KH, et al. The health care burden of high grade chronic obstructive pulmonary disease in Korea: analysis of the Korean Health Insurance Review and Assessment Service data. Int J Chron Obstruct Pulmon Dis 2013;8:561-8. [PubMed]


