
Single-dose del Nido cardioplegia used in adult minimally invasive valve surgery
Introduction
New challenges have appeared for myocardial protection with the new developments for minimally invasive heart surgery, in which there is a small incision, limited working field and relatively longer cross-clamp time, and in which multi-dose blood cardioplegia worsens the exposure of the working area. A single-dose cardioplegia method which can offer long-time preservation would be the ideal option. Histidine-Tryptophan-Ketoglutarate (HTK) is a single-dose of cardioplegia which has been used in some heart centers. However, the price of this solution is very high, especially in China. The protection for the patients with pre-operatively poor right ventricular function is inadequate (1,2). Moreover, the single dose of the 2,000 mL-volume solution, which enters into the circulation at one time may induce significant disturbance to homeostasis, and cause severe hemodilution, hyponatremia, along with other effects. An alternative, del Nido cardioplegia (DNC), developed in the early 1990s, is a single-dose, cost-effective formulation that has been safely used for decades in pediatric patients (3,4). The advantage of a single dose, which is said to last up to 180 min, has induced some clinicians in North American heart centers to adopt it, with success, for adult patients. We began to use DNC in adult minimally invasive valve surgery in May 2017. To analyze the safety and efficacy of DNC (1:4, blood: crystalloid) in adult minimally invasive valve surgery, we compared this solution with the classical whole blood cardioplegia (4:1, blood: crystalloid).
Methods
Ethics
This study was approved by the Ethics Committee in Zhongshan Hospital of Fudan University (approval No: 2017-120) and was conducted in full compliance with its policies and procedures.
Surgical technique
Between January and December 2017, 165 consecutive adults patients who underwent minimally invasive valve surgery by the same team of surgeons were divided into two cohorts based on the type of cardioplegia administered during surgery: (I) single-dose DNC (DNC group, n=76, male 41, female 35) used in patients from May to December 2017, and (II) intermittent standard whole blood cardioplegia based on St. Thomas solution (SBC group, n=89, male 45, female 44) used in patients from January to April, 2017. There were 123 patients (54 in the DNC group, 69 in the SBC group) who underwent mitral valve replacement or mitral valvuloplasty at 30 degrees in the left supine position and the surgical access was gained through the 4th intercostal with a thoracoscope. There were 35 patients (20 in the DNC group, 15 in the SBC group) who underwent aortic valve replacement in the supine position with the surgical access being gained through an “L” suprasternal incision. There were 7 patients (2 in the DNC group, 5 in the SBC group) who underwent double valve replacement at the supine position with the surgical access being gained through an “L” suprasternal incision.
Anesthesia and cardiopulmonary bypass (CPB)
All patients were operated under intravenous inhalation general anesthesia and mild hypothermia CPB. The circuit was primed with 1,000 mL of Plasma-Lyte A (Baxter Healthcare, Deerfield, IL, USA), 1,000 mL of Gelofusine (4%, B/Braun), 150 mL of 20% mannitol, 500 international unit (IU) of heparin, 40 mL of methylprednisolone (Pfizer Manufacturing Belgium NV) and 20 g of albumin (20%, Instituto Grifols, S.A. Anticoagulation was established with an initial dose of 400 IU per kilogram of body weight which was injected into the central venous line before the initiation of CPB with a target activated clotting time over 480 seconds. Venous drainage was gained by a 24-F femoral vein drainage tube (Edwards, Edwards Lifesciences LLC, Irvine, CA, USA) with about 40 mmHg negative pressure. If venous drainage was unsatisfactory, another 15-F femoral artery tube (Medtronic, Medtronic inc, Minneapolis, MN, USA) would be inserted into the right internal jugular vein to assist the venous drainage. The arterial inflow was through the femoral artery by 16–20 F femoral artery cannula (Edwards, Edwards Lifesciences LLC, Draper, UT, USA) selected by the size of the patient’s femoral artery. The pump flows on the bypass were maintained at 20–2.4 L/min/m2, and the mean arterial pressure was maintained at 50–70 mmHg. Carbon dioxide field flooding was routinely employed to help expel gas from the heart just before off-clamp.
Myocardial protection
Cardioplegia was delivered through aortic root without aortic insufficiency with 200–250 mmHg pump pressure and 100–120 mmHg pressure at the end of the cannula. In the case of aortic insufficiency where aortotomy would be performed, the aortotomy provided exposure and access to the coronary ostia for direct administration. Both cardioplegias were given at 10 °C. The standard cardioplegia based on SBC, referring to the basic principles of Buckberg solution (see Tables 1,2 for the comparison of the formulae and the concentration of solution composition after mixing with blood) with a 4:1 blood mixture was administered with 20 mL/kg volume and redosed at 20-min intervals with 300–500 mL solution with a half concentration of potassium. Warm blood given before off-clamp lasted for 5–10 min. For cases using DN (see Tables 1,2) with a 1:4 blood mixture, a single dose of 20 mL/kg volume (maximum dose of 1,000 mL for patients larger than 50 kg) was delivered.
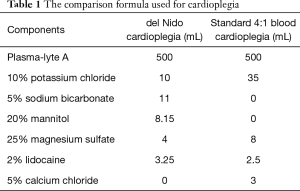
Full table
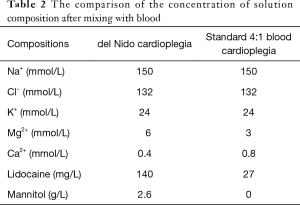
Full table
Variables collected included age, gender, body mass index (BMI), past medical history, preoperative comorbidities, preoperative evaluation of heart and other organs function, the type of operation, the CPB/cardioplegia details, time on ventilator, days stayed in ICU, postoperative complications, pre and postoperative echocardiography findings, and discharge status. All the variables of laboratory inspection came from the electronic medical record, and the postoperative sample was routinely obtained at the first postoperative day.
Statistics
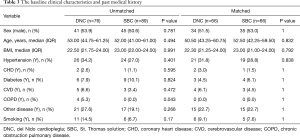
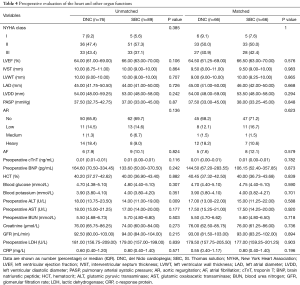
Median (interquartile range) and frequencies (percentages) were summarized by cardioplegia solution types (DNC solution and S cardioplegia solution) for continuous and categorical variables, respectively. A propensity score matching was performed to reduce the differences between the two groups and all variables listed in Tables 3,4 and operation types listed in Table 5 were included in a logistic regression model to estimate the propensity score. Nearest-neighbor matching without replacement was used, and the caliper of width equaled to 0.2 of the standard deviation of the logic of the propensity score. For unmatched data, Chi-square tests or Fisher Exact Tests were used for comparison of categorical variables and Wilcoxon tests were used for continuous variables between the two groups (Tables 3-6). For matched data, continuous variables were compared using the Wilcoxon signed-rank test, and binary variables and multiple categorical variables were analyzed using the McNemar test and Fisher Exact Tests respectively. Based on propensity-matched data, a linear regression model with cardioplegia group (DNC group vs. SBC group) as the main factors adjusting for aortic cross-clamp time, the interaction of cardioplegia group and aortic cross-clamp time, and operation types was used to assess the effect of cardioplegic solution type on the postoperative cTnT. The postoperative cTnT values were log transformed in the linear regression models to achieve the normality assumption. The results are shown in Table 7. All data was analyzed by using the R version 3.5.1 software.
Full table
Full table

Full table
Full table
Full table
Results
Preoperative data (Tables 3,4)
The baseline clinical characteristics including the age, the gender, BMI, the past medical history, the preoperative comorbidities, the New York Heart Association (NYHA) class, the left ventricular ejection fraction (LVEF), the interventricular septal thickness, the left atrial diameter, the left ventricular end-diastolic diameter, the pulmonary systolic pressure, the degree of aortic valve regurgitation, the prevalence of atrial fibrillation, the serum cTnT, the serum brain natriuretic peptide (BNP), the serum lactic dehydrogenase (LDH), the hematocrit (HCT), the blood glucose, the blood potassium, the serum glutamic oxaloacetic transaminase (AST), the serum glutamic pyruvic transaminase (ALT), the serum blood urea nitrogen (BUN), the serum creatinine (Cr), the glomerular filtration rate (GFR), the c-response protein (CRP) were similar between the two groups.
Operative data (Table 5)
Mitral valve surgeries accounted for the majority in both groups (71.1% in the DNC group, 77.5% in the SBC group). The volume of cardioplegia was significantly higher in the SBC group. Since the DN solution contained four-fifths crystalloid, the filtration volume was considerably higher in the DNC group. The automatic restoration of sinus rhythm in the DNC group was markedly higher than that in the SBC group (97.0% vs. 78.8%, P=0.006). There was no difference in the surgical procedures, the CPB time, and the cross-clamp time between the two groups.
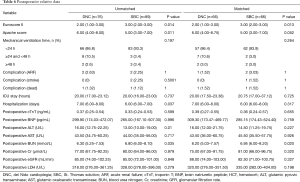
Postoperative data (see Table 6)
The Euroscore II was significantly lower in the DNC group compared with the SBC group (2.00 vs. 3.00, P<0.05). The BUN in the DNC group was substantially lower than that in the SBC group (6.20 vs. 6.95, P<0.05). The Apache score and the level of serum ALT were markedly higher in the DNC group compared with the SBC group pre-matched, but the differences disappeared after propensity- matching. There was no difference in the cTnT (0.39 vs. 0.36, P=0.655), the BNP, the LDH, the AST, the Cr, the GFR, the ventilation time, the ICU stay time, the hospital-stay days, the postoperative complications and the hospital death between the two groups.
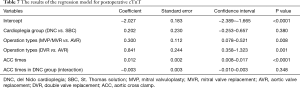
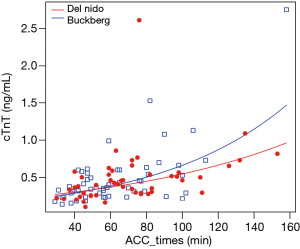
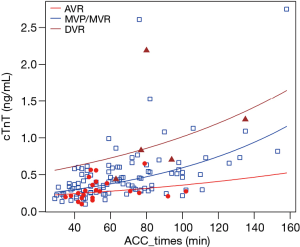
Postoperative cTnT (Table 7)
There was no significant influence of the cardioplegia group on postoperative cTnT (P=0.380), while the longer aortic cross-clamp time was associated with the higher cTnT levels. The operation types were closely related to the cTnT levels, but the interaction of the cardioplegia group and the aortic cross-clamp time was not significant (P=0.348). Some of these results can be seen in Figures 1,2.
Discussion
Since the inception and development of heart surgery, the discussion concerning myocardial protection has been going on for decades. At present, the most widely used 4:1 blood cardioplegia in adult cardiovascular surgery is a set of myocardial protection measures developed from Buckberg in the 1990s (5-7). This practice system of myocardial protection has been widely adopted in clinical application for many years because of its precise and cost-effective effect. It is considered the classical method of adult myocardial protection. Presently, with the rapid development of microinvasive surgery, and the increase of reoperation cases and severe patients in adult heart surgery, new requirements for myocardial protection have arisen. Due to the small working field in minimally invasive cardiac surgery, poor exposure, prolonged aortic cross-clamp time and worsening exposure with repeated infusion of blood cardioplegia, whether cardioplegia is reliable and effective via single infusion or prolonging repeating infusion interval, has become a new issue of contention in adult heart surgery.
DNC is named after Dr. Pedro del Nido, who, in the 1990s, with his study group in the University of Pittsburgh, developed a basic formula for the imitation of extracellular fluid. DNC still uses high potassium to induce cardiac arrest, which makes cardiac arrest rapid and straightforward. However, hyperkalemic arrest leads to depolarization of cardiac cell membrane, which inhibits the activity of Na+-K+ pump, and leads to Na+ accumulation in cells, followed by intracellular Ca2+ aggregation because of the Na+-Ca2+ exchange mechanism, resulting in cell damage. Therefore, in order to combat the adverse effects of hyperkalemic depolarization of cell membranes, a large dose of lidocaine, a Na+ channel blocker, is added to del Nido solution to prolong the cardiac myocyte refractory period and to increase the polarization of hyperkalemic depolarization of myocardial cell membrane. This inhibits the Na+-Ca2+ exchange mechanism thus preventing the accumulation of sodium and calcium ions in the cells, which causes the consumption of energy substrates in cardiomyocytes to slow down. At the same time, a high concentration of lidocaine also allows the effect of cardiac arrest to be sustained over a long time. Because only a single infusion is needed, and the myocardial protection effect is satisfactory, it has been used worldwide in the field of infant myocardial protection. It has been reported that cardiac arrest achieved by single infusion in pediatric cardiac surgery can be sustained for up to 180 min (4).
Therefore, in terms of myocardial protection, the most commonly used standard 4:1 blood cardioplegia in adult heart surgery has the disadvantage of incurring high potassium depolarization. With the development of surgical technology, the advantage of DNC is obvious because it meets the requirement of a single infusion or a long-repeated infusion interval.
Across many major US institutions and internationally, DNC has reported to have been successfully used in adults. For example, the Cleveland Heart Center in the United States stated that DNC was safe and effective compared with Buckberg solution in adult single heart valve surgery, and, that it could reduce blood sugar level, save medical expenses, and shorten the time of aortic occlusion and extracorporeal circulation (8). New York-Presbyterian Hospital reported that DNC could be safely used in aortic valve reoperation (9). In studies focusing on the CABG population, similar outcomes between traditional and DNC were reported (10-12). Some authors compared DNC with blood cardioplegia in adults undergoing valve replacement with or without CABG (13-15).
In order to determine the safety time limit of a single infusion of DNC, we contrived to select cases where the patients had small differences in indications, the surgical technique was mature and stable, the surgeon team was experienced, and where the time of aortic occlusion was expected to be within 60 to 90 min of minimally invasive cardiac valve surgery. The study was initially planned to be a prospective randomized controlled study, but the surgeons involved in the research underwent several surgical practice cases, and, because of the intuitive convenience of DNC in surgery, DNC was soon preferred. In order to complete the study safely and objectively while avoiding interference with the surgeon’s surgical skills and learning curve, we selected patients operated on by a single surgical group with a continuous minimally invasive cardiac valve operation within one year using a propensity score matching analysis to compare with traditional 4:1 blood cardioplegia. From the comparative statistical analysis of the two groups, the indices of myocardial injury, liver, and kidney function; Apache score; respiratory assist time; ICU time; hospitalization time; significant organ complications; and mortality after operation; were not significantly different. cTnT, a marker of myocardial injury, was selected as the main index of myocardial injury after the operation. Regression analysis showed that cTnT increased with the prolongation of myocardial ischemia time, and was closely related to the type of operation, but had no significant correlation with the kind of cardioplegia. What’s more, the Euroscore II, an indicator for predicting postoperative mortality and incidence of major cardiac adverse events, was significantly lower in the DNC group than that in the SBC group. In the DNC group, spontaneous restoration of sinus rhythm was more frequent, and this finding could be a result of the antiarrhythmic effect of lidocaine present in DNC.
The renal function, which is closely related to the cardiac function in the DNC group, was slightly better than that in the SBC group, but whether this advantage exists or not will require further investigation using a larger sample size or selecting cases with a longer duration of aortic cross-clamp. Therefore, this study proves preliminarily that the single-dose infusion of DNC is safe and effective in minimally invasive valve surgery in adults.
Our findings were consistent with most of the current literature (8-12). In adult cardiac surgery, the single-dose infusion of DNC can shorten the time of aortic clamp and cardiopulmonary bypass, because it makes the operation smoother, and obviates the need to interrupt the operation to repeat infusion of cardioplegia. Most scholars have argued that cardiac arrest with single-dose DNC for adult cardiac surgery can be maintained safely for 90 min (13-18). In this study, the time of aortic occlusion was 66±27 min during minimally invasive cardiac valve surgery, which was within the safe range of the single infusion. Therefore, the effect of a single infusion of DNC was equivalent to that of classical 4:1 blood cardioplegia within 90 min of cardiac arrest. The 90-min safety time of single infusion and a decreased need for defibrillation after aortic cross-clamping not only ensured the safety of the heart but also offered significant convenience for minimally invasive heart valve surgery. Furthermore, del Nido is extremely cheap compared with HTK solution, and thus its cost performance is particularly significant.
Based on this study, the positive evaluation of the safety and efficacy of single-dose infusion of DNC in 90 min led the surgical team to have great confidence in the application of DNC in adult cardiovascular surgery. The use of DNC in our hospital began with its advantages in minimally invasive cardiac surgery, and gradually was applied to all kinds of adult cardiac surgeries, including all major vascular surgeries, coronary surgeries, and heart valve surgeries. Subsequent studies, including those investigating the adjustment of cardiac arrest fluid infusion strategies in patients with coronary stenosis, ischemic cardiomyopathy, and hypertrophic cardiomyopathy, are ongoing.
The limitations of our findings can be characterized by the following aspects of our study: non-randomized single-center study, small sample size, involving minimally invasive surgery mostly confined to patients with low risk, and with a lack of long-term follow-up data.
Conclusions
According to our results, we can conclude that in minimally invasive cardiac valve operation in adults, a single infusion of DNC within 90 min of aortic occlusion can achieve the same protective effect as the standard 4:1 blood cardioplegia. This method can also improve surgical workflow by preventing the frequent interruptions caused by cardioplegia administration.
Acknowledgments
Funding: This study is supported by the second batch of joint research projects on major diseases, Shanghai Municipal Health Commission (the project fund number: W2014-009).
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: This study was approved by the Ethics Committee in Zhongshan Hospital of Fudan University (approval No: 2017-120) and was conducted in full compliance with its policies and procedures.
References
- Gaudino M, Pragliola C, Anselmi A, et al. Randomized trial of HTK versus warm blood cardioplegia for right ventricular protection in mitral surgery. Scand Cardiovasc J 2013;47:359-67. [Crossref] [PubMed]
- Siddiqi S, Blackstone EH, Bakaeen FG. Bretschneider and del Nido solutions: Are they safe for coronary artery bypass grafting? If so, how should we use them? J Card Surg 2018;33:229-34. [Crossref] [PubMed]
- Charette K, Gerrah R, Quaegebeur J, et al. Single dose myocardial protection technique utilizing del Nido cardioplegia solution during congenital heart surgery procedures. Perfusion 2012;27:98-103. [Crossref] [PubMed]
- Matte GS, del Nido PJ. History and use of del Nido cardioplegia solution at Boston Children’s Hospital. J Extra Corpor Technol 2012;44:98-103. [PubMed]
- Buckberg GD. Development of Blood Cardioplegia and Retrograde Techniques: The ExperimenterI Observer Complex. J Card Surg 1998;13:163-70. [Crossref] [PubMed]
- Buckberg GD, Beyersdorf F, Allen BS, et al. Integrated Myocardial Management: Background and Initial Application. J Card Surg 1995;10:68-89. [Crossref] [PubMed]
- Buckberg GD. Update on Current Techniques of Myocardial Protection. Ann Thorac Surg 1995;60:805-14. [Crossref] [PubMed]
- Mick SL, Robich MP, Houghtaling PL, et al. Del Nido versus Buckberg cardioplegia in adult isolated valve surgery. J Thorac Cardiovasc Surg 2015;149:626-34; discussion 634-6. [Crossref] [PubMed]
- Sorabella RA, Akashi H, Yerebakan H, et al. Myocardial protection using del Nido cardioplegia solution in adult reoperative aortic valve surgery. J Card Surg 2014;29:445-9. [Crossref] [PubMed]
- Hamad R, Nguyen A, Laliberte E, et al. Comparison of del Nido cardioplegia with blood cardioplegia in adult combined surgery. Innovations (Phila) 2017;12:356-62. [Crossref] [PubMed]
- Yerebakan H, Sorabella RA, Najjar M, et al. Del Nido cardioplegia can be safely administered in high-risk coronary artery bypass Grafting surgery after acute myocardial infarction: a propensity-matched comparison. J Cardiothorac Surg 2014;9:141-7. [Crossref] [PubMed]
- Ramanathan R, Parrish DW, Armour TK, et al. Use of del Nido cardioplegia in adult cardiac surgery. Thorac Cardiovasc Surg 2015;63:624-7. [Crossref] [PubMed]
- Timek T, Willekes C, Hulme O, et al. Propensity matched analysis of del Nido cardioplegia in adult coronary artery bypass grafting: Initial experience with 100 consecutive patients. Ann Thorac Surg 2016;101:2237-41. [Crossref] [PubMed]
- Kavala AA, Turkyilmaz S. Comparison of del Nido Cardioplegia with Blood Cardioplegia in Coronary Artery Bypass Grafting Combined with Mitral Valve Replacement. Braz J Cardiovasc Surg 2018;33:496-504. [Crossref] [PubMed]
- Ad N, Holmes SD, Massimiano PS, et al. The use of del Nido cardioplegia in adult cardiac surgery: A prospective randomized trial. J Thorac Cardiovasc Surg 2018;155:1011-8. [Crossref] [PubMed]
- Kim K, Ball C, Grady P, et al. Use of del Nido cardioplegia for adult cardiac surgery at the Cleveland clinic: Perfusion implications. J Extra Corpor Technol 2014;46:317-23. [PubMed]
- Li Y, Lin H, Zhao Y, et al. Del Nido cardioplegia for myocardial protection in adult cardiac surgery: A systematic review and meta-analysis. ASAIO J 2018;64:360-7. [Crossref] [PubMed]
- Tam DY, Fremes SE. Del Nido cardioplegia: A one stop shot for adult cardiac surgery? J Thorac Cardiovasc Surg 2018;155:1019-20. [Crossref] [PubMed]


