
Demographic ageing and its influence on current lung transplant practice
Hall and colleagues, from the University of Florida in Gainesville (USA) report in a recent issue of The Annals of Thoracic Surgery (1), an interesting analysis on the effect of both donor and recipient age on lung transplant outcomes. For their purpose, they reviewed the United Network for Organ Sharing (UNOS) database, recruiting all adult recipients transplanted between 2005 and 2015. Interestingly, on univariable analyses they observed that donors older than 60 years as well as recipients older than 70 years had the worst survival. Moreover, after analysing the combination of donor and recipient ages, they observed that only recipients aged between 60 and 69 years behaved worse when receiving donors over 60 years. Furthermore, any other negative impact on survival was found when other donor/recipient age combinations were investigated. These poor results of older donors are likely to be associated to the advanced age of the recipients to whom older donors are allocated, mainly receiving single lung transplants. However, in an additional propensity score matching analysis adjusting for relevant covariates, the authors found that when survival in recipients between 60 and 69 years was compared with those receiving younger donors versus donors older than 60 years, differences in recipient survival disappeared. The authors concluded that, given the growing population of recipients older than 60 years, the use of older donors in these patients is not related to higher mortality rates.
Undoubtedly, donor age restrictions in lung transplantation have been progressively relaxed over time in order to overcome the steadily increasing demand. At present, the ideal lung donor criterion of age less than 55 years is no longer taken into account in the majority of lung transplant centers. In addition, the last published guidelines of the International Society for Heart and Lung Transplantation (ISHLT) (2) obviated a recommendation of an upper age limit for lung donation. Therefore, the key issue is not the donor age but whether any kind of donor/recipient age matching has to be considered. It is conceivable that, as Hall and colleagues have demonstrated, older patients may receive older donors safely. If these old lungs behave well, showing good oxygenation, good elastic recoil, no lobar atelectasis, and absence of major pathological findings, it might be expected that the majority of such aged grafts will work well. But the question remains as to whether an old donor (beyond 65 years) may be suitable for a young patient with cystic fibrosis, for instance. It is our center’s policy to tend to allocate younger donors to younger recipients, whenever possible (3). In contrast, the data presented by Hall and colleagues implicate that even young patients may receive older donors. However, we must keep in mind that the natural period of function for a donor lung over 65 years transplanted into a 20-year-old recipient may last longer than 120 years, and we do not know whether this is possible, or if this recipient will develop an anticipated graft senescence.
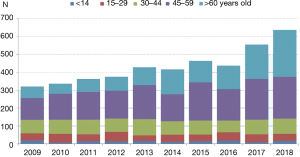
An important issue regarding the authors’ study refers to the donor profile. Only 20% of lung donors in USA are older than 50 years. On the contrary, donor age has increased progressively in Spain, so in 2018 up to 35% of effective lung donors were older than 60 years (Figure 1) (4). Hence, recipient characteristics (age, frailty) rather than donor factors (extended criteria donors) might be a critical element in determining the results of lung transplantation. Recently, we demonstrated worse early and long-term lung transplant outcomes in a group of “extended recipients” irrespective of whether the lung donor was optimal or marginal (5). Consequently, in order to achieve optimal results following lung transplantation, we should focus on the recipient rather than on the donor: a good recipient is expected to behave well either with lung grafts from ‘gold-standard’ donors or from non-ideal ones. Conversely, a critically ill recipient might have a calamitous post-transplant course despite receiving a strictly “perfect” donor. In support of this notion, we have observed some severe cases of primary graft dysfunction when matching very young lung donors to seriously ill old recipients, specially following single lung transplantation (5).
The strength of the present study is the use of the UNOS database and, consequently, the great number of cases accrued. It is impossible for a single Institution, or even multicentre studies to have the ability to recruit such number of patients. On the contrary, UNOS data have some limitations and biases that should be taken into account when examining big data, such as variability of clinical practice among contributing centers, missing data, etc. Moreover, monitoring the accuracy of transplant data, the validation process during data entry, and the internal verification at UNOS, have all limited to some degree these caveats when analysing UNOS database (6).
For practising surgeons, it’s of uppermost importance to accurately match the best recipient for a given lung donor offer. Aiming at optimal results, early transplant surgeons allocated standard criteria donors to carefully selected lung transplant recipients. However, the disparity between the increased demand and the shortage of ideal donors led most transplant groups to push the boundaries of lung transplant donor acceptability criteria. In addition, paralleling demographic ageing, median age of potential recipients on the waiting lists has steadily increased. But how far beyond the upper limit of 65 years we can dare to go in accepting donors for lung transplantation? In the current literature, published data concerning lung transplant outcomes for recipients of elderly donors remain conflicting. A large, single-centre study demonstrated that short and long-term outcomes were not worse when transplanting lung grafts from donors older than 55 years. It is noteworthy that allocating these older lung donors to recipients with pulmonary hypertension or to those requiring long periods of intraoperative cardiopulmonary bypass was associated with increased mortality rates (7). In line with this observation, Bittle and colleagues demonstrated similar outcomes after lung transplantation for recipients of donors aged 55–65 years as compared to those receiving grafts of younger donors (<55 years) (8). Considering recipient age, Katsnelson and colleagues concluded that donor age did not have an impact on mid-term survival for lung transplant recipients aged 65–80 years at transplantation (9).
Not all reports, however, support these findings. It is interesting to note that a review of 23,905 lung transplants from the UNOS database reported that allocating old donors to old recipients was not associated with a decreased survival. Nevertheless, the authors demonstrated that using old donors into younger recipients had a negative impact on survival (10).
In agreement with Shigemura and colleagues (7), we demonstrated that recipient characteristics could influence outcomes in patients who receive lung grafts from marginal donors (5). Consequently, it seems reasonable to diverge older donors to stable and surgically easy recipients, such as emphysema patients. As these patients usually show a more stable natural course of the disease, they could probably benefit more from being allocated to older donors. Moreover, in individuals with end-stage lung disease and limited life-expectancy, the decision of allocating them to an extended criteria donor or waiting for an ideal-criteria one should be based on other relevant factors such as mortality on waiting list or quality of life after lung transplantation. Thereby, when dealing with critically ill lung transplant recipients, it will be probably more adequate to look at prolonging life expectancy and quality of life rather than looking far beyond the horizon of a long graft survival.
Acknowledgments
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
References
- Hall DJ, Jeng EI, Gregg JA, et al. The impact of donor and recipient age: older lung transplant recipients do not require younger lungs. Ann Thorac Surg 2019;107:868-76. [Crossref] [PubMed]
- Chambers DC, Cherikh WS, Goldfarb SB, et al. The International Thoracic Organ Transplant Registry of the International Society for Heart and Lung Transplantation: Thirty-fifth adult lung and heart-lung transplant report—2018; Focus theme: Multiorgan Transplantation. J Heart Lung Transplant 2018;37:1169-83. [Crossref] [PubMed]
- Moreno P, Alvarez A, Carrasco G, et al. Lung transplantation for cystic fibrosis: differential characteristics and outcomes between children and adults. Eur J Cardiothorac Surg 2016;49:1334-43. [Crossref] [PubMed]
- Available online: (accessed: May 17, 2019).http://www.ont.es/infesp/Paginas/Memorias.aspx
- Moreno P, Alvarez A, Santos F, et al. Extended recipients but not extended donors are associated with poor outcomes following lung transplantation. Eur J Cardiothorac Surg 2014;45:1040-7. [Crossref] [PubMed]
- Dickinson DM, Bryant PC, Williams MC, et al. Transplant data: sources, collection, and caveats. Am J Transplant 2004;4 Suppl 9:13-26. [Crossref] [PubMed]
- Shigemura N, Horai T, Bhama JK, et al. Lung transplantation with lungs from older donors: recipient and surgical factors affect outcomes. Transplantation 2014;98:903-8. [Crossref] [PubMed]
- Bittle GJ, Sanchez PG, Kon ZN, et al. The use of lung donors older than 55 years: a review of the United Network of Organ Sharing database. J Heart Lung Transplant 2013;32:760-8. [Crossref] [PubMed]
- Katsnelson J, Whitson BA, Tumin D, et al. Lung transplantation with lungs from older donors: an analysis of survival in elderly recipients. J Surg Res 2017;214:109-16. [Crossref] [PubMed]
- Hayes D Jr, Black SM, Tobias JD, et al. Influence of donor and recipient age in lung transplantation. J Heart Lung Transplant 2015;34:43-9. [Crossref] [PubMed]


