
Is arthroplasty necessary after sternoclavicular tumor resection?
Introduction
The diagnosis and treatment of tumors involving the sternum are managed by thoracic and those of tumors of the clavicle by orthopedic surgeons. Presently, there are a number of reports documenting sternoclavicular joint reconstruction after sternal tumor resection (1,2). However, the management of clavicular tumors is controversial (3,4). When the lesion involves the sternoclavicular joint, it is often necessary to resect not only parts of the sternum and clavicle but also the sternoclavicular joint. The process of sternoclavicular joint reconstruction is challenging, and the need for it is often questioned by both thoracic and orthopedic surgeons. There is a paucity of literature on this subject. In this report, we retrospectively reviewed 5 patients with sternoclavicular joint pathologies who were treated between 2016 and 2017. By combining our findings with existing reports, we discuss the approaches to the management of this disease.
Clinical
Patient information
Our series included 5 patients (2 male, ranging in age from 39 to 60 years with a mean of 52 years). Primary symptoms include sternoclavicular joint pain with varying degrees of limitation to the range of motion of the shoulder joint and numbness of the upper extremities. Radiographic studies indicated osseous lesions at the sternoclavicular joint. Three patients underwent unilateral procedures while two patients underwent bilateral sternoclavicular joint resections. Sternoclavicular joint reconstruction was not performed in any patient. One patient was diagnosed with follicular thyroid carcinoma metastasis of the sternum, one patient had malignant transformation of osteochondroma, one patient had a grade I periosteal chondrosarcoma, one patient had reactive osteopetrosis, and one patient had Ewing’s sarcoma.
Operative techniques
Patients were placed under general anesthesia in the supine position. Padding was placed posterior to the shoulders to provide slight elevation. A T-shaped incision was used for bilateral sternoclavicular joint resection (Figure 1). For unilateral sternoclavicular joint resection, the incision extended proximally from the sternoclavicular joint towards the towards the sternal angle and the side of the pathological clavicle (Figure 2). The first rib, sternum, and clavicle subjacent to the tumor were liberally exposed. The type of disease dictated the extent of resection. Resection of the clavicle is made with a wire saw. The disease-free side of the sternoclavicular joint was preserved. An electric saw was then used to cut the sternum down to the upper edge of the second rib, whereas the first rib was cut using rib shears, which completed the tumor resection. The tumor was then dissected by exposing the clavicles bilaterally, first and second ribs, and the superior aspect of the sternum. If the tumor invaded the first rib, then the amount resected from the second rib was increased to achieve a R0 resection with complete removal of the lesion. For all patients, sternoclavicular arthroplasty was not performed and a clavicular stump was left in place. For one patient with bilateral sternoclavicular joint resections, the superior sternum and second rib were resected, leaving a large defect in the chest wall. As a result, a titanium alloy sternal fixation plate was secured bilaterally to the second ribs and a polyester patch was used to fill the superior portion of the defect. Surgical drains were placed in all patients and later removed in a timely fashion. We encountered no injuries to the subclavian artery and vein, innominate vein, or brachial plexus. For all patients, functional rehabilitation was initiated 2 weeks after surgery.
Results
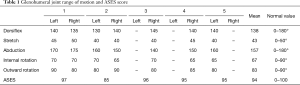
All patient had incisions closed primarily for healing by first intention with no associated complications. Chest CT was performed three months after surgery and no hemothorax, pneumothorax, or tumor recurrence was observed. Patients were instructed to initiate an exercise regimen. At the 6-month post-operative follow-up, active range of motion of the shoulder was assessed and scored using the American Shoulders and Elbow Surgeon (ASES) guidelines (Table 1). The average shoulder active range of motion was 157° with an ASES score of 94. All patients were able to place one palm on the top of his/her head and to independently perform activities of daily living. Three patients complained of chest tightness, and two patients reported numbness near the incision site.
Full table
Discussion
The sternoclavicular joint is a synovial joint whose stability is maintained by multiple ligaments. Therefore, sternoclavicular arthroplasty relies on the reconstruction of the ligaments (5,6). Serious ligamentous injury can occur in the traumatic setting but its surgical management has always been an orthopedic challenge. Relevant research have reported that surgical treatment can achieve good efficacy for traumatic sternoclavicular dislocation, but there are also many failure cases. Currently, internal fixation for traumatic sternoclavicular dislocation is still in discussion. Experts have attempted various repair techniques with no significant efficacy in establishing stability or preventing recurrent dislocations (7-10). When a pathological lesion involves the sternoclavicular joint, to ensure maximum resection of the tumor, complete resection of the sternoclavicular joint and the surrounding tissue is often necessary. Conventional steel plating does not replace ligament function, cannot guarantee joint stability, and can be easily dislocated due to movement of the upper extremity. For this reason, some experts have proposed using the second metatarsophalangeal joint for reconstruction (11). While shoulder function recovered well in these patients, one sustained a post-operative dislocation of the sternoclavicular joint. Reconstruction with the second metatarsophalangeal joint is traumatic, requires an autologous toe joint, can be technically challenging, and the reconstructed joint risks post-operative dislocation. Recent literature also reports the usage of a mesh-bone cement sandwich for sternoclavicular joint reconstruction (12,13). However, limited data exist on sternoclavicular joint reconstruction using synthetic materials. Additionally, implants may be affected by poor biocompatibility and can be costly. Some experts believe that sternoclavicular joint resection has little effect on shoulder joint mobility, because in their studies that mainly focused on clavicular tumors, they performed partial or total resection of the clavicle, with no reconstruction, and they found that post-operative shoulder function was unaffected (14). However, all reported cases document unilateral resections, and no reports have documented bilateral resections.
In this series, five patients underwent sternoclavicular joint resection without arthroplasty. In one patient who underwent bilateral resection of the sternoclavicular joint as well as the first ribs, significant restoration of shoulder function was achieved with rehabilitation by 3 months after surgery and complete recovery by 6 months with an ASES score of 97 and full ability to perform the activities of daily living. In the second patient, resections of bilateral sternoclavicular joint and the first and second ribs were performed with subsequent chest wall patch reconstruction involving the bilateral first and second rib stumps. This patient complained of post-operative chest wall tightness. At the 3-month post-operative follow-up, this patient’s shoulder abduction reached an average of 120°. Due to poor recovery of shoulder range of motion, the patient underwent focused rehabilitation and, upon 6-month post-operative follow-up, the patient’s shoulder abduction improved to an average of 155°. In the remaining 3 patients, unilateral sternoclavicular joint and first rib resections were performed. At 3–6 months follow-up, their shoulder joint mobility returned to normal. At 6-month follow-up, all five patients were able to perform shoulder abduction to an average of 157° with an ASES score of 94 and independently perform activities of daily living. Due to the weak thoracic subcutaneous tissue in the anterior chest wall, sternoclavicular joint resection may often be extensive resulting in the formation of a contracted scar that can limit shoulder function. This indicates that early post-operative mobility exercises are vital to recovery. When SCJ resection is performed, there is indeed some instability in the proximal clavicle. During the follow-up of the patients, it can be seen that the proximal clavicle has some activity when the upper limbs move, but this does not affect the shoulder joint movement. The residual clavicle stump after resection of the sternoclavicular joint does not significantly affect the aesthetics of the chest wall during shoulder movement.
In summary, pathological lesions involving the sternoclavicular joint requiring unilateral or bilateral joint resection do not require arthroplasty. Moderate post-operative functional exercises can achieve meaningful recovery of shoulder range of motion with minor impact on upper extremity function and no negative effects on activities of daily living. If the resection is extensive, we advocate for attempting reconstruction at the rib attachments of the sternum rather than at the stenoclavicular joint. Due to fewer cases studies at present, it is necessary to continue to study whether reconstruction is required after sternoclavicular joint resection in adolescents.
Acknowledgments
I would like to thank all my teachers who have helped me to develop the fundamental and essential academic competence. My sincere appreciation also goes to the colleagues from Department of Thoracic surgery, Shanghai Sixth People's Hospital Affiliated to Shanghai Jiaotong University, who participated this study with great cooperation.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images.
References
- Aranda JL, Jimenez MF, Rodriguez M, et al. Tridimensional titanium-printed custom-made prosthesis for sternocostal reconstruction. Eur J Cardiothorac Surg 2015;48:e92-4. [Crossref] [PubMed]
- Okui M, Kohno M, Shigenobu T, et al. Resection and reconstruction of sternum. Kyobu Geka 2014;67:38-43. [PubMed]
- Li Z, Ye Z, Zhang M. Functional and oncological outcomes after total claviculectomy for primary malignancy. Acta Orthop Belg 2012;78:170-4. [PubMed]
- Kapoor S, Tiwari A, Kapoor S. Primary tumours and tumorous lesions of clavicle. Int Orthop 2008;32:829-34. [Crossref] [PubMed]
- Lee JT, Campbell KJ, Michalski MP, et al. Surgical anatomy of the sternoclavicular joint: a qualitative and quantitative anatomical study. J Bone Joint Surg Am 2014;96:e166. [Crossref] [PubMed]
- Renfree KJ, Wright TW. Anatomy and biomechanics of the acromioclavicular and sternoclavicular joints. Clin Sports Med 2003;22:219-37. [Crossref] [PubMed]
- Bontempo NA, Mazzocca AD. Biomechanics and treatment of acromioclavicular and ternoclavicular joint injuries. Br J Sports Med 2010;44:361-9. [Crossref] [PubMed]
- Rockwood CA Jr, Groh GI, Wirth MA, et al. Resection arthroplasty of the sternoclavicular joint. J Bone Joint Surg Am 1997;79:387-93. [Crossref] [PubMed]
- Groh GI, Wirth MA, Rockwood CA Jr. Treatment of traumatic posterior sternoclavicular islocations. J Shoulder Elbow Surg 2011;20:107-13. [Crossref] [PubMed]
- De Palma A, Sollitto F, Loizzi D, et al. Chest wall stabilization and reconstruction: short and long-term results 5 years after the introduction of a new titanium plates system. J Thorac Dis 2016;8:490-8. [Crossref] [PubMed]
- Bendon CL, Giele HP. Second toe metatarsophalangeal joint transfer for sternoclavicular joint reconstruction. J Hand Surg Am 2014;39:1327-32. [Crossref] [PubMed]
- Collaud S, Pfofe D, Decurtins M, et al. Mesh-bone cement sandwich for sternal and sternoclavicular joint reconstruction. Eur J Cardiothorac Surg 2013;43:643-5. [Crossref] [PubMed]
- Hajjar WM, Alnassar S, Abu-Daff SN, et al. A novel technique for the reconstruction of resected sternoclavicular joints: A case report with a review of the literature. Ann Thorac Med 2013;8:60-3. [Crossref] [PubMed]
- Rossi B, Fabbriciani C, Chalidis BE, et al. Primary malignant clavicular tumours: a clinicopathological analysis of six cases and evaluation of surgical management. Arch Orthop Trauma Surg 2011;131:935-9. [Crossref] [PubMed]


