
The safety and feasibility of thoracoscopic uncommon pulmonary segmentectomy
Introduction
Although the standard surgical procedure for primary lung cancer is anatomic lobectomy, the number of patients undergoing anatomic pulmonary segmentectomy is increasing as several previous studies have demonstrated non-inferior oncological and perioperative results in both intentional and unintentional segmentectomies (1,2).
Brunelli described that frequently performed segmentectomies including upper division segmentectomy of the left upper lobe, lingual segmentectomy, superior segmentectomy of the lower lobe and basilar segmentectomy of the lower lobe were decided as common segmentectomies while any segmentectomies except for common segmentectomies were as uncommon segmentectomies (3). General thoracic surgeons currently have more opportunities to perform uncommon pulmonary segmentectomy, because the rates of detection of small ground glass opacities and partial solid nodules have increased. In addition, small-sized solid nodules suspected to be indicative of pulmonary metastasis are being detected more frequently, where these can also be a candidate for uncommon pulmonary segmentectomy.
Thoracoscopic lobectomy is considered the standard approach for patients with early stage lung cancer worldwide, where several previous reports have demonstrated that the thoracoscopic approach is less invasive and non-inferior oncologically than the thoracotomy approach (4,5). The minimal invasiveness of the thoracoscopic approach also applies to segmentectomy. Lopez-Pastorini et al. reported that thoracoscopic segmentectomy is associated with decreased postoperative drainage and hospitalization time, and less severe complications (6). However, the proportion of segmentectomies performed via the thoracoscopic approach remains low compared to lobectomy due to technical difficulties. Brunelli described that only 25% of segmentectomies were performed via thoracoscopic approach in the last edition of the European Society of Thoracic Surgeons (ESTS) database (3). Moreover, uncommon segmentectomy is frequently performed via a thoracotomy because uncommon pulmonary segmentectomies are associated with various technical difficulties compared to common segmentectomies. In this study, we investigated the safety and feasibility of thoracoscopic uncommon pulmonary segmentectomy.
Methods
This study was approved by Japanese Red Cross Maebashi Hospital Institutional Review Board (No. 2019-16).
A total of 105 patients underwent thoracoscopic anatomic pulmonary segmentectomy in our department between March 2006 and September 2018. Among them, 37 received an uncommon segmentectomy and 68 received a common segmentectomy. In this study, uncommon pulmonary segmentectomy was defined as any segmentectomy except for segmentectomies of the lingual, basilar, or superior segment of the lower lobe, or upper division of the left upper lobe as Brunelli previously described (3). We retrospectively compared patient characteristics and perioperative outcomes between patients receiving uncommon versus common segmentectomy.
During the same period, we performed 656 thoracoscopic lobectomies. In our institutional policy, lobectomy was standard resection for patients with non-small cell lung cancer (NSCLC). Intentional segmentectomy for NSCLC was performed only for patients with less than 1 cm solid part when the patient chose not lobectomy but intentional segmentectomy. In addition, unintentional segmentectomy was performed for patients with low pulmonary function or poor cardiopulmonary status as a passive limited resection. In case with pulmonary metastasis from other types of cancer, wedge resection was basically selected. If it was difficult to ensure the safe margin by wedge resection because of the tumor location, segmentectomy was performed. In case with benign disease, the surgical procedure is selected by the same criteria as pulmonary metastasis.
All patients in our department, except for those with an allergy to the contrast agent, underwent preoperative three-dimensional computed tomography (3D-CT) angiography and bronchography to image bronchovascular structures and determine the relative locations of the tumors and pulmonary vessels.
In our department, senior surgeons (M Kamiyoshihara and H Igai) usually performed pulmonary segmentectomy due to the technical difficulties although several cases of lobectomies were performed by mid-career surgeons.
The thoracoscopic pulmonary segmentectomy was performed under general anesthesia using one-lung ventilation with the patient in the lateral decubitus position. We placed a monitor above the head of the patient to image all procedures. A 10- or 5-mm flexible type thoracoscope was utilized in all patients. Our thoracoscopic anatomic pulmonary resection involves three or four ports. A 3–5 cm access incision was made in the fourth or fifth intercostal space on the anterior axillary line. The thoracoscopic port was placed in the sixth or seventh intercostal space on the posterior axillary line. An additional port for surgical instruments was placed in the sixth intercostal space on the anterior axillary line. If necessary, we also placed an additional port on the sixth or seventh intercostal space just beside the scapula angle. The access incision and additional ports for surgical instruments were covered with an XXS-sized wound retractor (Alexis Wound Retractor; Applied Medical, Rancho Santa Margarita, CA, USA). Large vessels or bronchi were divided with a stapler. Small-caliber vessels were divided with an energy device or scissors after ligation. The specimen was placed in an endovascular bag and retrieved through the access incision after the pulmonary segmentectomy was completed. The access incision was lengthened if necessitated by the size of the specimen. A rib-spreader was not used in any case. The interlobar and hilar lymph node were sampled in patients with primary lung cancer undergoing segmentectomy to confirm pathological stage. In intentional segmentectomies, we planned to perform additional lobectomy if the resected lymph node was positive. In unintentional segmentectomies, we did not plan to perform additional lobectomy because these patients were not able to be tolerate for additional lobectomy. No lymphadenectomy was performed in patients with metastatic lung cancer or benign disease.
We adopted the inflation-deflation technique or selective jet ventilation to identify the intersegmental plane accurately (7). Moreover, we also used intersegmental pulmonary veins in the hilum area as landmarks to identify the intersegmental plane. After identification, we utilized electrocautery or staplers to divide the intersegmental plane depending on the surgeons’ preference. However, the hilum area of the intersegmental plane was usually divided with a stapler to avoid a postoperative air leak due to a fistula of a bronchiole, even if we utilized electrocautery to divide the peripheral area. Finally, the intersegmental plane was covered with a polyglycolic acid sheet (Neovail, sheet type; Gunze, Kyoto, Japan), and fibrin glue spray (Bolheal; Chemo-Sero Therapeutic Institute, Kumamoto, Japan, or Beriplast P; CSL Behring, King of Prussia, PA, USA) was applied to the intersegmental plane to reduce postoperative air leaks.
To compare the perioperative results between patients undergoing common segmentectomy and uncommon segmentectomy, statistical analyses using the Mann-Whitney U test or Fisher’s exact test were performed. Differences were considered significant at P<0.05. Calculations and statistical tests were performed with the EZR graphical user interface (Saitama Medical Centre, Jichi Medical University, Saitama, Japan).
Results
Table 1 lists the lobes, including the resected segments, operated on during the common and uncommon segmentectomies in this study. While uncommon segmentectomies were performed in the left S1+2 in nine patients, S3 in three, S9+10 in one, others including the sub-segment area in one, right S1 in four, S2 in six, S3 in two, S7+8 in two, S9+10 in six, and others including the sub-segment area in three, common segmentectomies were performed in the left superior segment of the upper lobe in twenty patients, lingual segment in eight, left posterior segment of the lower lobe (S6) in eleven, left basal segment in seven, right posterior segment of the lower lobe (S6) in nineteen, and right basal segment in three.

Full table
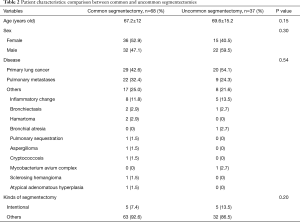
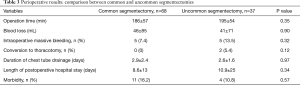
No significant differences were observed in patient characteristics between the two groups, including age (67.2±12 vs. 69.6±15.2 years, P=0.15), sex (female/male: 36/32 vs. 15/22, P=0.3), disease (primary lung cancer/pulmonary metastases/others: 29/22/17 vs. 20/9/8, P=0.54), or the ratio of intentional to other types of segmentectomy (intentional/other: 5/63 vs. 5/32, P=0.2) (Table 2). The two groups did not differ significantly in terms of perioperative results, including operative time (186±57 vs. 195±54 min, P=0.35), blood loss (46±85 vs. 41±71 mL, P=0.9), postoperative drainage (2.9±2.4 vs. 2.6±1.6 days, P=0.97), postoperative hospitalization (8.6±13 vs. 10.9±25 days, P=0.34), morbidity rate (16.2 vs. 10.8%, P=0.57), rate of conversion to thoracotomy (0% vs. 5.4%, P=0.12), or rate of significant bleeding (7.4% vs. 13.5%, P=0.32; Table 3). There was no mortality in both groups.
Full table
Full table
In patients with primary lung cancer undergoing intentional segmentectomies, 5 patients underwent usual segmentectomies while 5 patients underwent unusual segmentectomies. Although tumor size in a patient was pathologically 27 mm, tumor sizes in other 9 patients were 5 mm or less. No local recurrence in the intersegmental plane and intrathoracic lymph node or distant metastasis were detected in the patients undergoing usual and unusual segmentectomies (mean observational period, 721±283 days).
In patients with primary lung cancer undergoing unintentional segmentectomies, 24 patients underwent usual segmentectomies while 15 patients underwent unusual segmentectomies. Although only a patient revealed hilar lymph node metastasis pathologically, other 38 patients revealed no lymph node metastasis. There was only a patient in each metastasis including local recurrence in intersegmental plane, intrathoracic lymph node metastasis or distant metastasis. Tumor size was 13.9±11.6 mm in the 38 patients. There was no significant difference about tumor size between the patients undergoing usual and unusual segmentectomies (P=0.27). In addition, tumor size was not significantly correlated with the rate of local recurrence in intersegmental plane, intrathoracic lymph node metastasis or distant metastasis (P=0.1, 0.3, 0.14). In addition, there were no significant differences between the patients undergoing usual and unusual segmentectomies about the rate of local recurrence in intersegmental plane, intrathoracic lymph node metastasis or distant metastasis (P=0.37, 0.37, 0.37).
Discussion
We performed uncommon segmentectomies in 37 cases with pulmonary benign or malignant disease, and showed that uncommon segmentectomies are not inferior to common segmentectomies in terms of perioperative results.
An uncommon pulmonary segmentectomy has some technical difficulties compared to common segmentectomy. Oizumi et al. defined uncommon segmentectomies as those involving more than two intersegmental planes made during the operation (8). Segmentectomies requiring dissection of multiple intersegmental surfaces were classified as “fairly difficult” or “difficult” in that study. To overcome technical difficulties, it is important to recognize the optimal technique for uncommon segmentectomy. For instance, our group previously used the “intersegmental tunneling method” during thoracoscopic lateral and posterior (S9+10) segmentectomy, which is an uncommon type of segmentectomy (9). Using this technique, we accurately identified the branches of the pulmonary vein projecting to the affected basilar and posterior segment, which helped us perform this uncommon segmentectomy satisfactorily. Oizumi et al. described that knacks or tips which help thoracic surgeons perform anterior segmentectomy of right upper lobe in their previous report (10). They insisted the key to perform this unusual segmentectomy successfully is to release the vascular sheath using forceps and dissect the parenchyma using a sealing device. In addition, the slip knot method was introduced as the procedure making it possible to remove the smaller subsegments with sufficient surgical margin. They finally concluded that anterior segmentectomy of right upper lobe was successfully performed by using these useful techniques although the segmentectomy was considered fairly difficult. Aside from these useful techniques for uncommon pulmonary segmentectomies by Japanese surgeons, Rakovich described key aspects of the surgical techniques for thoracoscopic left apical bisegmentectomy, and reported successful results (11). Moreover, González-Rivas et al. provided guidance for several types of uncommon segmentectomies using a uniportal thoracoscopic approach (12). The wide variety of useful techniques allows uncommon segmentectomies to be performed successfully. Thoracoscopic uncommon pulmonary segmentectomy is feasible and safe if all such techniques are taken into consideration.
It is also important to determine the relative locations of the tumor and pulmonary vessels to ensure an appropriate intersegmental plane and oncological safety margin. Many previous studies describing common and uncommon pulmonary segmentectomies discussed the importance of preoperative 3D-CT angiography and bronchography for recognizing these locations (13,14). Therefore, all patients (except one with an allergy to the contrast agent) in our department underwent preoperative 3D-CT angiography and bronchography. We were able to examine the surgical margin between the intersegmental plane and the tumor by palpation using a thoracotomy approach. However, we are unable to palpate the tumor during the thoracoscopic approach. Therefore, thoracic surgeons must ensure an adequate oncological safety margin without palpating the tumor during thoracoscopic pulmonary segmentectomy. Preoperative recognition of the relative location of the tumor and pulmonary vessels can help ensure an adequate oncological safety margin when using the thoracoscopic approach. Moreover, the inflation-deflation and selective jet ventilation techniques occasionally fail to identify the intersegmental plane accurately, especially in an emphysematous lung, because of collateral ventilation. Misaki et al. reported using infrared thoracoscopy to identify the intersegmental line without inflating the lung, by injecting indocyanine green (15). Although this dye-based method is useful for patients with an emphysematous lung, infrared thoracoscopy is required and the intersegmental lines can only be observed for a few minutes because the dye disappears due to pulmonary circulation. Therefore, in cases of an emphysematous lung, we divide the intersegmental plane along the branches of the pulmonary vessels in the direction from the hilum to the periphery. Exposing the pulmonary vessel toward the periphery as much as possible aids smooth and safe stapler insertion.
Several studies have demonstrated that the locoregional recurrence rate for segmentectomy is not inferior to that for lobectomy in patients with NSCLC (16-18). Ginsberg et al. demonstrated no significant differences in outcome between lobectomy and anatomical segmentectomy, although this was based on a subset analysis (18). Furthermore, the proportion of uncommon segmentectomies in these studies was not reported. An uncommon segmentectomy is characterized by two or more divided intersegmental planes. Therefore, it is more difficult to create an appropriate intersegmental plane during uncommon versus common segmentectomy. As a result, uncommon segmentectomy has more difficulties with respect to achieving an oncological safety margin than common segmentectomy, which might increase the local recurrence rate. Nevertheless, the non-inferiority of uncommon segmentectomy in terms of the local recurrence rate was shown in this study using preoperative 3D-CT angiography and bronchography. However, the number of patients in this study was relatively small; a larger prospective study might be necessary to accurately determine the local recurrence rate in uncommon pulmonary segmentectomy.
Conclusions
In this study, we showed the non-inferiority of uncommon pulmonary segmentectomy compared to common segmentectomies in short-term perioperative outcomes. Thoracoscopic uncommon pulmonary segmentectomy is feasible and safe with use of appropriate techniques. It also helps ensure a sufficient oncological safety margin through division of the appropriate intersegmental plane.
Acknowledgments
The authors appreciate all of the surgeons and coworkers who contributed to this study, and we thank the editors and reviewers for their assistance with the manuscript.
Footnote
Conflicts of Interest: Meeting presentation: The abstract has been presented at the 27th European Conference on General Thoracic Surgery of the European Society of Thoracic Surgeons, Dublin, Ireland, 9-12 June 2019.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. This study was approved by Japanese Red Cross Maebashi Hospital Institutional Review Board (No. 2019-16); all patients provided written informed consent prior to their inclusion in the study.
References
- Vansteenkiste J, Crinò L, Dooms C, et al. 2nd ESMO Consensus Conference on Lung Cancer: early-stage non-small-cell lung cancer consensus on diagnosis, treatment and follow-up. Ann Oncol 2014;25:1462-74. [Crossref] [PubMed]
- Detterbeck FC, Mazzone PJ, Naidich DP, et al. Screening for lung cancer: Diagnosis and management of lung cancer, 3rd ed: American College of Chest Physicians evidence-based clinical practice guidelines. Chest 2013;143:e78S-92S.
- Brunelli A. Uncommon pulmonary anatomic segmentectomies: state of the art and technical aspects. J Vis Surg 2018;4:175. [Crossref]
- Stephens N, Rice D, Correa A, et al. Thoracoscopic lobectomy is associated with improved short-term and equivalent oncological outcomes compared with open lobectomy for clinical Stage I non-small-cell lung cancer: a propensity-matched analysis of 963 cases. Eur J Cardiothorac Surg 2014;46:607-13. [Crossref] [PubMed]
- Scott WJ, Allen MS, Darling G, et al. Video-assisted thoracic surgery versus open lobectomy for lung cancer: a secondary analysis of data from the American College of Surgeons Oncology Group Z0030 randomized clinical trial. J Thorac Cardiovasc Surg 2010;139:976-81; discussion 981-3. [Crossref] [PubMed]
- Lopez-Pastorini A, Koryllos A, Schnell J, et al. Perioperative outcome after open and thoracoscopic segmentectomy for the treatment of malignant and benign pulmonary lesions: a propensity-matched analysis. J Thorac Dis 2018;10:3651-60. [Crossref] [PubMed]
- Okada M, Mimura T, Ikegaki J, et al. A novel video-assisted anatomic segmentectomy technique: selective segmental inflation via bronchofiberoptic jet followed by cautery cutting. J Thorac Cardiovasc Surg 2007;133:753-8. [Crossref] [PubMed]
- Oizumi H, Kanauchi N, Kato H, et al. Anatomic thoracoscopic pulmonary segmentectomy under 3-dimensional multidetector computed tomography simulation: a report of 52 consecutive cases. J Thorac Cardiovasc Surg 2011;141:678-82. [Crossref] [PubMed]
- Igai H, Kamiyoshihara M, Kawatani N, et al. Thoracoscopic lateral and posterior basal (S9 + 10) segmentectomy using intersegmental tunnelling. Eur J Cardiothorac Surg 2017;51:790-1. [PubMed]
- Oizumi H, Kato H, Endoh M, et al. Port-access thoracoscopic anatomical right anterior segmentectomy. J Vis Surg 2015;1:16. [PubMed]
- Rakovich G. Thoracoscopic left apical bisegmentectomy. Multimed Man Cardiothorac Surg 2018. [Crossref] [PubMed]
- González-Rivas D, Lirio F, Sesma J. Uniportal anatomic combined unusual segmentectomies. J Vis Surg 2017;3:91. [Crossref] [PubMed]
- Iwata H, Shirahashi K, Mizuno Y, et al. Surgical technique of lung segmental resection with two intersegmental planes. Interact Cardiovasc Thorac Surg 2013;16:423-5. [Crossref] [PubMed]
- Oizumi H, Kato H, Endoh M, et al. Techniques to define segmental anatomy during segmentectomy. Ann Cardiothorac Surg 2014;3:170-5. [PubMed]
- Misaki N, Chang SS, Igai H, et al. New clinically applicable method for visualizing adjacent lung segments using an infrared thoracoscopy system. J Thorac Cardiovasc Surg 2010;140:752-6. [Crossref] [PubMed]
- Martin-Ucar AE, Nakas A, Pilling JE, et al. A case-matched study of anatomical segmentectomy versus lobectomy for stage I lung cancer in high-risk patients. Eur J Cardiothorac Surg 2005;27:675-9. [Crossref] [PubMed]
- Pastorino U, Valente M, Bedini V, et al. Limited resection for Stage I lung cancer. Eur J Surg Oncol 1991;17:42-6. [PubMed]
- Ginsberg RJ, Rubinstein LV. Randomized trial of lobectomy versus limited resection for T1 N0 non-small cell lung cancer. Ann Thorac Surg 1995;60:615-22; discussion 622-3. [Crossref]


