
Comparison of the perioperative efficacy between single-port and two-port video-assisted thoracoscopic surgery anatomical lung resection for non-small cell lung cancer: a systematic review and meta-analysis
Introduction
Lung cancer is one of the tumours with the highest risk in the world, and its morbidity and mortality is increasing year by year. At present, surgery is still the first choice for the treatment of lung cancer. However, with the rapid development of minimally invasive concepts, the surgical approach to lung cancer has shifted from traditional thoracotomy to thoracoscopic surgery with minimal trauma and quick recovery. In the last three decades, video-assisted thoracoscopic surgery (VATS) has gradually become a standard option in the diagnosis and treatment of non-small cell lung cancer. Compared with traditional open thoracotomy, the main advantages of VATS cover reduction of postoperative pain (1), shortened postoperative hospital stay (2) and a better perioperative result (3). In 1998, Yamamoto et al. first reported a single-port thoracoscopic surgery (4). Since then, several surgeons have been willing to explore the new area of minimally invasive thoracic surgery.
Two-port thoracoscopic surgery: 3–5 cm along the intercostal incision in the 5th intercostal space of the anterior iliac crest as the only operation port, and a 2 cm thoracoscope observation hole in the 7th intercostal space or the 8th rib of the midline of the iliac crest. Single-port thoracoscopic surgery: 3 to 5 cm along the intercostal incision in the 5th intercostal space at the anterior iliac crest, no insertion of the distractor, no secondary operation ports and separate observation ports. In 2011, Gonzalez-Rivas et al. first reported a single-port VATS lobectomy (5). More and more surgeons regard uniport VATS as a feasible option for non-small cell lung cancer. Reduced postoperative pain with paresthesia, improved patient satisfaction (6), reduced surgical trauma (7), and better cosmetic results (8) are the most significant features of the single-port technique.
However, few studies have compared single-port with two-port VATS anatomical lung resection in patients with early-stage NSCLC, and whether uniport VATS is associated with a higher number of potential advantages remains controversial. The purpose of this systematic review and meta-analysis is to compare the perioperative efficacy between single-port and two-port VATS anatomical lung resection in patients with early-stage NSCLC. The evaluation index included the duration of operation, bleeding volume, number of lymph nodes retrieved, duration of postoperative drainage, postoperative hospital-stay, postoperative pain using the visual analogue scale (VAS), and complications.
Methods
Data sources
We searched for eligible studies published before 1st December 2018 in The Cochrane Library, PubMed, Embase, Web of Science, and China Biology Medicine disc. In order to maximize the sensitivity of the search and identify all of the relevant studies, the following groups of keywords or MeSH terms were used, “uniportal” or “uniport” or “single-port” or “single port” or “single-incision” or “single incision”, and “two port” or “two-port” or “two incision” or “two-incision”, and “VATS” or “video-assisted” or “video-assisted thoracoscopic surgery” or “thoracic surgery” or “thoracoscopic surgery” or “video-assisted”, and “non-small cell lung cancer” or “non-small cell lung carcinoma” or “non-small cell lung neoplasms” or “lung adenocarcinoma” or “lung squamous cell carcinoma” or “large cell lung cancer”. Simultaneously, we scrutinized the references that were included in any of the identified literature to determine the comprehensiveness of the literature search.
Study inclusion
Studies were considered to be eligible and were included if they met the following criteria: (I) they discussed patients who were diagnosed as early NSCLC referring to the stage I-II according to the staging criteria of the International Association for the Study of Lung Cancer (IASLC) 2018 eighth edition (9); these patients did not received neoadjuvant therapy before surgery; (II) they were randomized or non-randomized controlled trials of single-port and two-port VAT; (III) the pathological diagnosis was early non-small cell lung cancer (including preoperative biopsy, intraoperative frozen section, or routine postoperative pathology); (IV) their data was comprehensive and complete; (V) they were published in Chinese or English.
Studies were excluded if they met the following conditions: (I) it was evident from the indications that the patients were not early NSCLC (and were likely small cell lung cancer, or lung carcinoid); (II) they were reviews, case reports, letters, comments, or meta-analyses; (III) they contained irrelevant or incomplete data; (IV) they were animal experiments; and (V) the tumor described was a metastatic lesion of other tumors.
Data extraction and critical appraisal
All relevant data were extracted independently by two reviewers (G Zhang and W Yang) from the text, and figures and tables were derived from identified papers. The information gathered included the first author, year of publication, country or region, study type and period, and TNM Classification of Malignant Tumors (TNM). In addition, the subjects’ baseline characteristics including the number of cases in each group, mean age, gender, tumor location, pathological type and size, and outcome measures were gathered. These outcome measures included duration of operation, perioperative bleeding volume, number of lymph nodes retrieved, duration of postoperative drainage, length of postoperative hospital stay, pain scores on days 1 and 3 postoperatively, and complications. If the two researchers disagreed on the statistical results, they intensively discussed the issue and eventually reached a consensus. The final results were adjudicated and reviewed by a senior investigator (S Pan).
A meta-analysis of the data included in the literature was performed using the Cochrane Collaboration RevMan5.3 software (Cochrane Collaboration, Software Update, Oxford, UK; http://review-manager.software.informer.com/5.3/). We estimated the effective values of the dichotomous variables or continuous variables by odds ratio (OR) or normalized mean differences (SMD) and 95% confidence intervals (CI), respectively. Heterogeneity testing was performed on the included studies using the Chi-square and I2 tests (10). If each study was homogenous (P>0.05 or I2 <50%), a fixed effects model was used for meta-analysis; if there was heterogeneity between studies (P<0.05 or I2 >50%), the random effects model was analyzed. A funnel plot in which no fewer than 10 studies were included was drawn to observe the distribution pattern of clinical research data collected to determine whether publication bias existed.
Results
This paper follows the guidelines for a systematic review and meta-analysis. Our electronic retrieval strategy identified a total of 421 studies from 5 electronic databases. After deleting duplicates, irrelevant articles, comments, case reports, letters, and meta-analyses, 15 papers were identified and further evaluated by screening the full text. After excluding 4 studies that did not provide sufficient data, 11 studies (11-21) were included for a final evaluation and were considered suitable for a quantitative meta-analysis. The article selection process is shown in Figure 1.
Study characteristics and risk of bias assessment
The included studies were published before December 1st, 2018. All 11 studies, containing 3 prospective studies and 8 retrospective observational studies, comprised a total of 1,592 patients of whom 854 (53.6%) and 738 (46.4%) underwent single-port VATS and two-port VATS respectively. Among these studies, one article used a propensity score or a matched pair method (12). If studies were homogeneous (P>0.05 or I2 <50%), a fixed-effects model was used for meta-analysis; otherwise, the random-effects model was used. The standard for evaluation in all of the available studies was NOS quality scale, with scores ranging from 5 to 8. A detailed summary of the study characteristics is presented in Table 1.
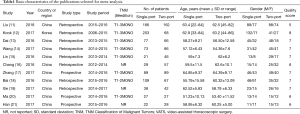
Full table
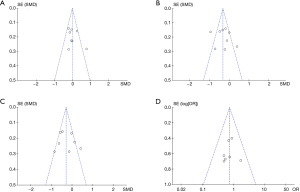
This meta-analysis used Review Manager Version 5.3 to assess publication bias, in which no fewer than 10 studies were included. Publication bias was evaluated for the number of lymph nodes retrieved, duration of postoperative drainage, length of postoperative hospital-stay, and complications. The results, summarized in Figure 2, illustrate that there was less publication bias in our meta-analysis according to symmetrical funnel plots.
Operative outcomes
Duration of operation
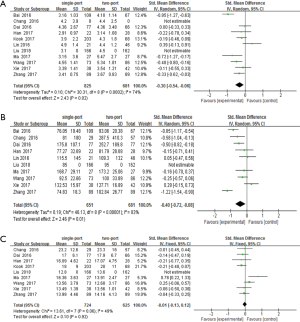
Eleven studies, including a combined total of 1,592 patients, reported comparable data relating to the operating time in the treatment of early NSCLC. We detected high heterogeneity between the single-port and two-port groups (P=0.0002, I2=74%), and used random models for analysis. A forest plot suggested that single-port VATS was associated with less operative time than the two-port VATS groups. There was a significant difference between the single-port and two-port VATS groups (SMD =−0.30; 95% CI: −0.54, −0.06; P=0.02). The detailed results of this analysis are shown in Figure 3A.
Bleeding volume
A total of 10 studies reported comparable data relating to bleeding volume, with a combined total of 1,332 patients. High heterogeneity was detected between the single-port and two-port VATS groups (P<0.00001, I2 =83%), and a random effects model was used to finish the analysis. From the forest plot, we discovered that single-port VATS was associated with a reduced bleeding volume when compared with two-port VATS. The difference between the groups was statistically significant (SMD =−0.40; 95% CI: −0.72, −0.08; P=0.01). The specific results are given in Figure 3B.
Number of lymph nodes retrieved
Comparable data from a combined total of 1,349 patients from 9 studies were used for statistical analysis. Moderate heterogeneity was observed between the single-port and two-port VATS (P=0.06, I2 =49%). Therefore, a fixed effects model was used for analysis. As shown in the forest plot, there was no significant difference between the single-port and two-port VATS groups (SMD =−0.01; 95% CI: −0.13, 0.12; P=0.92). The detailed results of this analysis are shown in Figure 3C.
Duration of postoperative drainage
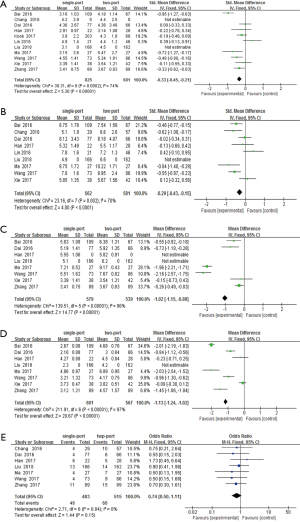
Eleven studies reported comparable data relating to the duration of postoperative drainage, with a combined total of 1,506 patients. High heterogeneity was detected between the single-port and two-port VATS groups (P=0.0002, I2 =74%), and a random effects model was used to finish the analysis. A forest plot suggested that single-port VATS was associated with less operative time than two-port VATS groups. There was significant difference between the single-port and two-port VATS groups (SMD =−0.33; 95% CI: −0.45, −0.21; P<0.00001). The specific results are given in Figure 4A.
Postoperative hospital-stay
Data relating to hospital stay were obtained from 9 articles, including a combined total of 1143 patients. We detected high heterogeneity between the single-port and two-port groups (P=0.002, I2 =70%), and used random effects models for analysis. Compared with the two-port VATS groups, single-port VATS had a shorter postoperative hospital stay. The difference between the groups was statistically significant (SMD =−0.29; 95% CI: −0.43, −0.15; P<0.0001). The results of this analysis are summarized in Figure 4B.
VAS 24 h after operation
We respectively extracted data relating to VAS 24 h after operation from 8 articles. High heterogeneity was detected at 24 h between the single-port and two-port VATS groups (24 h: P<0.00001; I2 =96%), and we used a random effects model for analysis. The forest plot showed that single-port VATS was significantly associated with lower VAS 24 h after operation (24 h: SMD = −1.02; 95% CI: −1.15, −0.88; P<0.00001). The specific results are given in Figure 4C.
VAS 72 h after operation
We extracted data relating to VAS 72 h after operation from eight articles. High heterogeneity was detected at 72 h between the single-port and two-port VATS groups (72 h: P<0.00001; I2 =97%), and we used a random effects model for analysis. The forest plot showed that single-port VATS was significantly associated with lower VAS 72 h after operation (72 h: SMD = −1.13; 95% CI: −1.24, −1.02; P<0.00001). We also found from the forest plot that single-port VATS was correlated with a lower VAS 24 h and 72 h after operation (24 h: SMD = −1.02; 95% CI: −1.15, −0.88; P<0.00001; 72 h: SMD = −1.13; 95% CI: −1.24, −1.02; P<0.00001). The results of this analysis are summarized in Figure 4D.
Complications
Seven studies included comparable data related to the rate of complications, with a combined total of 998 patients. No heterogeneity was detected between the single-port and two-port VATS groups (P=0.84; I2 =0%), and a fixed effects model was therefore used for analysis. There was no significant difference between the single-port and two-port VATS groups in terms of complications (single-port: 9.5%, two-port: 12.8%), and there was no significant difference between the single-port and two-port VATS groups (OR =0.74; 95% CI: 0.50, 1.11; P=0.15). The results of this analysis are summarized in Figure 4E.
Discussion
Endoscopic surgery for non-small cell lung cancer is currently the mainstream method for the treatment of this disease. Due to the traditional surgical trauma caused by traditional porous laparoscopic techniques, even postoperative rehabilitation is affected due to severe trauma. Therefore, the single-port, two-port, and other less traumatic endoscopic surgical methods have been vigorously developed (22). Single-port thoracoscopic surgery has only one operation hole. The thoracoscope and the surgical instruments all enter from one incision site. Surgeons who perform single-port thoracoscopic surgery generally have extensive experience in minimally invasive surgery and gradually shift from three-port to two-port and then into the field of single-port thoracoscopic surgery; this familiarizes them with the structure of the thoracoscopic lung anatomy. Due to the limited operating space and lack of fine operation on blood vessels, the incidence of major bleeding complications is relatively high in the early stage of learning. Therefore, the rate of conversions to thoracotomy or multiport thoracoscopic is relatively high. With the accumulation of experience, the need to place the second or the third port to fix the pulmonary veins gradually reduces. Therefore, the success rate of single-port VATS lobectomy has significantly improved, while the operation time remains relatively fixed (23,24).
Single-port thoracoscopic surgery may have certain restrictions on the operating angle, but it also has advantages. First, the visual field is the same as the projection surface of the instrument, and the optical depth is preserved. Second, vision and operation surface are on the same sagittal plane, which helps to accurately operate at the distance. Last, the operation fulcrum is located in the chest, forming an operation triangle near the target area, and the operation effect is similar to the traditional thoracotomy (25). However, there are still concerns about the thoroughness of single-port thoracoscopic treatment of lung cancer, and it is believed that there may be a risk of incomplete resection of the lesion. To clarify the feasibility of clinical application and the advantages of single-port thoracoscopic surgery, this study compared it with two-port thoracoscopic surgery, specifically in terms of macroscopic surgical efficiency.
In the treatment of early NSCLC, surgeons are increasingly using single-port VATS as a minimally invasive alternative to two-port VATS. From the meta-analysis, we can conclude that there is a statistically significant reduction in the duration of the operation time, bleeding volume, length of postoperative drainage, postoperative hospital-stay, VAS 24 h after operation, and VAS 72 h after operation in patients who underwent single-port VATS compared with two-port VATS. However, there were no significant differences in the number of lymph nodes retrieved and the rate of complication. This suggests that single-port VATS can achieve relatively similar or better results during perioperative periods than two-port VATS.
In theory, because of the small incision, the limited intercostal space, and the inevitably substantial interference between the thoracoscope and the instrument, what is considered to be the main disadvantage of single-port VATS arises: patients may have a longer operation time (5). However, in our meta-analysis, findings indicated that single-port VATS was associated with a shortened duration of surgery. One possible reason for this is that a single-port thoracoscopic approach can provide direct vision, just like thoracotomy. Also, the surgery in the single-port VATS group was performed by skilled surgeons due to the difficulty involved in operating thoracic surgery through one intracostal space, while the surgery in the two-port VATS group was performed by less skilled surgeons due to the ease afforded through being able to use both hands.
Duration of operation and bleeding volume are the two main aspects we are concerned with. Our meta-analysis shows that single-port VATS is associated with less length of operation time and bleeding volume. Although the difference was statistically significant (duration of operation: P=0.0002; bleeding volume: P<0.00001), clinical differences may not be apparent. We also found that single-port VATS has a shorter duration of postoperative drainage and postoperative hospital stay, indicating that single-port VATS is beneficial for patient recovery. The method of placing the drainage tube under the subcutaneous ribs in the original incision of the single-hole group can still retain the advantage of the single incision and can also effectively reduce the postoperative tube time and improve the infection of the incision. These are in line with the concept of enhanced recovery after surgery (ERAS) (26). Huang (27) conducted a preliminary study of fast track surgery combined with single-port thoracoscopic surgery for lung cancer. The clinical data of 83 patients with early stage non-small cell lung cancer were retrospectively analyzed. Among these patients, 38 patients in the ERAS group underwent single-port VATS and completed a series of ERAS measures. The control group underwent three-well VATS and routine perioperative measures. The results showed that all patients completed the operation. The visual analog scale (VAS) was better on the third day after operation in the ERAS group, and the chest tube indwelling time and hospital stay were shorter (P<0.05). ERAS combined with single-port VATS is considered safe and feasible for the treatment of non-small cell lung cancer, and can promote the recovery of patients and shorten the length of hospital stay.
However, the accuracy of these parameters is difficult to evaluate because there are no gold standard criteria, and it is challenging to have the same or similar surgical procedures in different national medical institutions.
Lymph node dissection in lung cancer surgery is an essential part of radical resection. Surgical cleaning of a sufficient number of lymph nodes can better control staging and primary tumors and has guiding significance for diagnosis and adjuvant therapy. Single-port VATS lymph node dissection can meet the minimum requirements (28), reduce the damage to patients, reduce the inhibition of lymphocytes, inhibit the reaction of pro-inflammatory cytokines, and play an essential role in protecting the cellular immune function of postoperative patients.
Pain score is an essential factor affecting the overall treatment effect, the patient’s subjective comfort level, and postoperative recovery rate. The pain score of thoracotomy is significantly higher than that of thoracoscopic surgery, and the traumatic effects of different operations in thoracoscopic surgery are also quite different. Single-port thoracoscopic incision takes into account the location of the lesion and drainage of the incision, which reduces the chest wall incision and reduces tissue trauma without increasing the difficulty of surgery. Single-port VATS is superior to two-port VATS in terms of duration of VAS 24 h after operation and VAS 72 h after operation. This may be due to the single incision: the damage to the surrounding tissue and the intercostal nerve is relatively small, so the inflammatory response is weaker, which is beneficial to the postoperative recovery of the patient. Although our results show a reduction in pain scores (measured by VAS) (VAS 24 h after operation: P<0.00001; VAS 72 h after operation: P<0.00001), it is clear that standardized and objective pain management programs are needed to assess the advantages of the single-port VATS for the pain management approach.
The primary complications of lung surgery include prolonged air leak, pneumonia, atelectasis, wound infection, etc. It has been found that to reduce the incision, the infection rate of the incision is increased after the drainage tube is directly placed in the traditional single-hole group. The healing time is prolonged, and the drainage tube placement time is longer than that of the two-hole group. The method of placing the drainage tube under the subcutaneous ribs in the original incision of the single-hole group can still retain the advantage of the single incision, and can also effectively reduce the postoperative tube time while improving the infection of the incision. The results of our study showed that the incidence of postoperative complications was lower in the single-port group than in the two-port group, but there was no significant difference between the two groups (P>0.05).It indicates that single-port VATS is independent of higher surgical risk and can meet safety requirements. Single-port VATS can be a first-line approach for elective thoracoscopic surgery (29).
Despite our considerable efforts, there are still several shortcomings in our systematic review and meta-analysis. First, it has the time limit, with a mortality rate of 0% in both groups. Since most of the single-port VATS cases that we statistically calculated were recently performed, systematic review and meta-analysis of long-term survival rates have not yet been carried out. Second, these data were indirectly extracted from the original article. Due to the lack of raw data of lobectomy and segmentectomy, there may still be some subjective bias and error. Third, geographical limitations are a factor that cannot be ignored. All the documents selected for this analysis are from Asia (China and Korea). Due to differences in physician experience and technology, our analysis results might have been greatly affected. Therefore, the results of this meta-analysis cannot necessarily be universally applied, and the value of the study for surgeons worldwide will vary. Fourth, this paper contains a total of 11 articles, with only 5 of these (11-13,19,21) indicating that all the operations were performed by one surgeon, with the other six (14-20) not clearly stating the surgeon number. Also, whether the surgeon had extensive experience in performing single-port and two-port thoracoscopic surgery was not mentioned, and this may have a significant impact on our analysis results. Another limitation is the specification of surgical procedure type, including lobectomy, segmentectomy, and sub-segmental resection of the lung. Because of the lack of uniform standards in the choice of surgical methods in each region, our system analysis may not be representative. Finally, of all the studies we analyzed, only 3 were prospective studies while 8 were retrospective studies. The small number of prospective studies included in this metanalysis, along with the high heterogeneity found in the analysis of the results between the two groups for each of the outcome variable selected, may represent strong biases regarding a correct interpretation of the results. In the future, we need to collect more prospective and randomized controlled studies to arrive at more objective and accurate conclusions.
Conclusions
In summary, our meta-analysis provides crucial evidence that single-port VATS anatomical lung resection may be superior to two-port VATS in terms of duration of operation, bleeding volume, duration of postoperative drainage, postoperative hospital-stay, VAS 24 h after the operation, and VAS 72 h after operation. Our results suggest that single-port VATS anatomical lung resection for non-small cell lung cancer may be a better treatment choice for skilled thoracic surgeons because of its better perioperative efficacy.
Acknowledgments
Funding: This work was supported by the National Natural Science Foundation of China (Grant No. 81370118, 81770018) (www.nsfc.gov.cn/).
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
References
- Lewis RJ, Caccavale RJ, Sisler GE, et al. Video-assisted thoracic surgical resection of malignant lung tumors. J Thorac Cardiovasc Surg 1992;104:1679-85. [PubMed]
- Palade E, Guenter J, Kirschbaum A, et al. Postoperative pain in the acute phase after surgery: VATS lobectomy vs. open lung resection - results of a prospective randomised trial. Zentralbl Chir 2014;139 Suppl 1:S59-66. [PubMed]
- Higuchi M, Yaginuma H, Yonechi A, et al. Long-term outcomes after video-assisted thoracic surgery (VATS) lobectomy versus lobectomy via open thoracotomy for clinical stage IA non-small cell lung cancer. J Cardiothorac Surg 2014;9:88. [Crossref] [PubMed]
- Yamamoto H, Okada M, Takada M, et al. Video-assisted thoracic surgery through a single skin incision. Arch Surg 1998;133:145-7. [Crossref] [PubMed]
- Gonzalez-Rivas D, Paradela M, Fernandez R, et al. Uniportal video-assisted thoracoscopic lobectomy: two years of experience. Ann Thorac Surg 2013;95:426-32. [Crossref] [PubMed]
- Ocakcioglu I, Alpay L, Demir M, et al. Is single port enough in minimally surgery for pneumothorax? Surg Endosc 2016;30:59-64. [Crossref] [PubMed]
- Yang HC, Noh D. Single incision thoracoscopic lobectomy through a 2.5 cm skin incision. J Thorac Dis 2015;7:E122-5. [PubMed]
- Rocco G, Martucci N, La Manna C, et al. Ten-year experience on 644 patients undergoing single-port (uniportal) video-assisted thoracoscopic surgery. Ann Thorac Surg 2013;96:434-8. [Crossref] [PubMed]
- Carter BW, Lichtenberger JP 3rd, Benveniste MK, et al. Revisions to the TNM Staging of Lung Cancer: Rationale, Significance, and Clinical Application. Radiographics 2018;38:374-91. [Crossref] [PubMed]
- Yang X, Li M, Yang X, et al. Uniport versus multiport video-assisted thoracoscopic surgery in the perioperative treatment of patients with T1-3N0M0 non-small cell lung cancer: a systematic review and meta-analysis. J Thorac Dis 2018;10:2186-95. [Crossref] [PubMed]
- Liu Z, Yang R, Shao F. Comparison of Postoperative Pain and Recovery between Single-Port and Two-Port Thoracoscopic Lobectomy for Lung Cancer. Thorac Cardiovasc Surg 2019;67:142-6. [Crossref] [PubMed]
- Han KN, Kim HK, Choi YH. Midterm outcomes of single port thoracoscopic surgery for major pulmonary resection. PloS One 2017;12:e0186857. [Crossref] [PubMed]
- Dai F, Meng S, Mei L, et al. Single-port video-assisted thoracic surgery in the treatment of non-small cell lung cancer: A propensity-matched comparative analysis. J Thorac Dis 2016;8:2872-8. [Crossref] [PubMed]
- Wang L, Liu D, Lu J, et al. The feasibility and advantage of uniportal video-assisted thoracoscopic surgery (VATS) in pulmonary lobectomy. BMC Cancer 2017;17:75. [Crossref] [PubMed]
- Lin F, Zhang C, Zhang Q, et al. Uniportal video-assisted thoracoscopic lobectomy: An alternative surgical method for pulmonary carcinoma. Pak J Med Sci 2016;32:1283-5. [PubMed]
- Chang JM, Kam KH, Yen YT, et al. From biportal to uniportal video-assisted thoracoscopic anatomical lung resection: A single-institute experience. Medicine (Baltimore) 2016;95:e5097. [Crossref] [PubMed]
- Zhang WG, Gu DL, Fang X, et al. Effect comparison of single-port and single-port operation video—-assisted thoracoscopic lobectomy in patients with early stage non-small cell lung cancer. Biomed Eng Clin Med 2017;21:390-4.
- Bai Y, Lv DS, Li M, et al. The analysis of clinical value between uniportal and two-port video-assisted thoracoscopic surgery for non-small cell lung cancer. Med Philoso 2016;37:31-3.
- Xie JJ, Chen MD, Chen QH, et al. Efficacy comparison of uniportal video-assisted, single utility port video-assisted and 3-portal video assisted thoracic surgery in patients with early non-small cell lung cancer. Guangzhou Med J 2017;48:32-5.
- Ma HB, Huang W, Luo F, et al. Comparison of clinical effects between single-port video assisted versus single—incision thoracoscopic pulmonary lobectomy. Guangxi Med J 2017;39:971-3.
- Han XQ, Lei YY, Zeng B, et al. Clinical research of single-incision VATS, single utility port VATS and conventional three-portal VATS in radical resection of lung cancer. J Trop Med 2017;17:569-73.
- Cai K, Yan Y, Feng S, et al. Unidirectionally progressive resection of lower left lung carcinoma under video-associated thoracoscopy. J Thorac Dis 2015;7:2371-5. [PubMed]
- Drevet G, Ugalde Figueroa P. Uniportal video-assisted thoracoscopic surgery: safety, efficacy and learning curve during the first 250 cases in Quebec, Canada. Ann Cardiothorac Surg 2016;5:100-6. [Crossref] [PubMed]
- Liu X, Chen X, Shen Y, et al. Learning curve for uniportal video-assisted thoracoscopic surgery lobectomy-results from 120 consecutive patients. J Thorac Dis 2018;10:5100-7. [Crossref] [PubMed]
- Cai K, Zhao H, Wu H, et al. Unidirectionally progressive resection of left upper pulmonary lobe under video-assisted thoracoscopy. J Thorac Dis 2014;6:1843-7. [PubMed]
- Kehlet H, Wilmore DW. Evidence-based surgical care and the evolution of fast-track surgery. Ann Surg 2008;248:189-98. [Crossref] [PubMed]
- Huang H, Chen S. Enhanced recovery after surgery using uniportal video-assisted thoracic surgery for lung cancer: A preliminary study. Thorac Cancer 2018;9:83-7. [Crossref] [PubMed]
- Delgado Roel M, Fieira Costa EM, González-Rivas D, et al. Uniportal video-assisted thoracoscopic lymph node dissection. J Thorac Dis 2014;6:S665-8. [PubMed]
- Chen CH, Chang H, Lee SY, et al. Single-port thoracoscopic surgery can be a first-line approach for elective thoracoscopic surgery. Rev Port Pneumol 2012;18:278-84. [Crossref] [PubMed]



