
Chest wall reconstruction using a new titanium mesh: a multicenters experience
Introduction
Chest wall reconstruction is a challenging area of thoracic surgery. The integrity of the chest wall is fundamental for correct respiratory dynamics and in protecting the organs contained in the thorax (1,2). The first chest wall reconstruction has been reported in the 1896 by Tensini using a pedicle latissimus dorsi flap to cover an anterior chest wall defect (3). The earlier attempts of chest wall surgery were limited by the availability of suitable materials to guarantee a durable and effective reconstruction. The last decade has seen improvements in surgical techniques and the introduction of different synthetics or biological materials allowing extensive chest wall resection and reconstruction with acceptable morbidity and mortality (2,4-8). Titanium has been introduced in surgical practice in the last twenty years. It is a very useful material because of optimal biocompatibility, resistance and low specific weight (2,9). We report our experience using a new titanium mesh for chest wall reconstruction in different pathological settings.
Methods
Patients
Between January 2014 to September 2018, 26 patients underwent chest wall reconstruction with the titanium mesh (MDF Medica S.r.l) at four different Italian Thoracic Surgery Departments. This retrospective multicenter study was approved by the Institutional Review Board of Ferrara S. Anna Hospital and implemented and approved by the other centers committees, the written informed consent was obtained from all patients. Patients’ demographics, past medical history, preoperative risk profile, anatomical location and size of the defect, the number of resected ribs, the associated surgical procedures and the operative time were recorded prospectively. Procedure-related complications, 30-day mortality, length of intensive care stay and postoperative hospital stay were also collected. All elective patients underwent pulmonary function test, chest X-ray and blood tests. CT-scan was performed in all patients, PET-scan was used in neoplastic cases. Preoperative histological evaluation was achieved with core needle biopsy, incisional biopsy or trans-bronchial biopsy in all neoplastic patients. Patients with sternal dehiscence were treated previously with antibiotic therapy on the basis of isolated germs and with negative pressure topic therapy. Surgery was planned after three consecutive negative wound cultures. In chest wall trauma and sternal dehiscence cases a CT-scan before surgery to evaluate the extension of the defect was performed.
Surgical treatment
All the operations were performed under general anesthesia. The double lumen intubation was used in case of planned associated lung resection otherwise the operation was performed with single lumen intubation. In oncological patients, care was taken to leave at least 2.5 cm of macroscopic margins during chest wall resection in lung cancer invading the chest wall or in case of chest wall metastases from other tumors; a minimum of 4 cm macroscopic margins was considered optimal in case of primary chest wall malignant tumors. The timing of surgery in trauma patients and patients with post sternotomy dehiscence must be made in the context of the patients overall clinical condition. A left- sided double-lumen tube was only used in patients with suspected active intrathoracic bleeding or with lung laceration. Lateral or posterior decubitus positioning allows access to most rib fractures. Supine position provides optimal exposure for anterior and antero-lateral fractures. Exposure of fractures is usually performed through a single incision above the fractured ribs. Chest wall muscles were spared whenever possible.
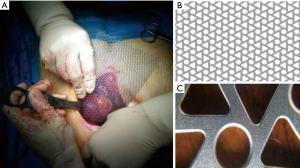
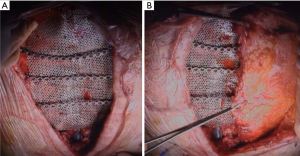
The mesh (MDF Medica S.r.l, Italy) is made of pure titanium, for medical use, grade 2. It could be produced in a custom fashion but usually two mesh thicknesses are available: a 0.6 mm thick used for reconstruction requiring greater rigidity, such as sternal replacement or anterolateral huge chest wall defects. The 0.4-mm thick mesh can be used for reconstructions requiring a more flexible material. The mesh is produced in only one size of 200×140 mm. The titanium mesh has a special triangle design that gives it non-deformability and mechanical resistance in the face of excellent elasticity, in addiction the special production technique (Photochemical Etching) under temperature control eliminate thermal risks and preserve metallurgical properties, it provides constant device performance during and after surgery. The mesh could be simply tailored using mayo or heavier scissors. It is flexible and easily modeled with hands. After achieving the desired shape, the mesh can be fixed to the defect using steel wires or thick polypropylene stiches, or even with screws through the triangular shape holes of the mesh (Figure 1).
Postoperative care and follow-up
Follow-up was performed by outpatient visit and chest roentgenogram performed one week after surgery and 15 days after discharge in all uncomplicated cases. Oncological cases underwent thoracic contrast CT scan 3 months after surgery and then every 6 months. All the other patients underwent a CT scan evaluation after 3 months from the operation and after one year. New onset or unusual chest pain and/or swelling at the site of implant were an indication for dedicated chest roentgenograms. In case of suspected failure of the implant, a CT-scan with multiplanar reconstruction was then performed.
Results
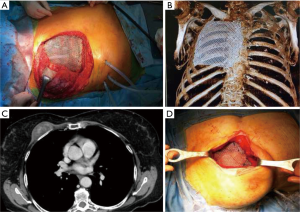
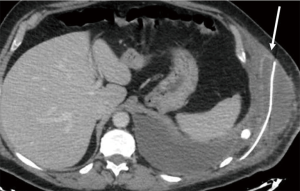
Twenty-six patients were included in the analysis. There were 19 males (73%) and 7 females (27%) with a mean age of 65.5 years (range, 17 to 81 years). Twenty-five patients (96%) underwent elective surgery; only one patient (4%) after chest wall trauma was operated urgently (4%). Patients’ characteristics are reported in Table 1. The indications for surgery included neoplastic diseases in 18 cases (69%): ten patients (38%) were found affected by primary or secondary chest wall tumors, eight patients (31%) by chest wall infiltration from lung cancer (Table 2). Two patients (8%) were treated because of massive sternal dehiscence after sternotomy, two patients (8%) underwent chest wall reconstruction after thoracic trauma, and two patients (8%) had a severe chronic pulmonary herniation, one after a previous trauma and one after previous lung surgery. Furthermore, two patients (8%) underwent surgery because of failure of the previous chest wall reconstruction: one had failure of sternal reconstruction for chondrosarcoma using marlex mesh with methyl methacrylate sandwich with damage to the ascending aorta and the latter failed after lateral chest wall reconstruction using a bioprosthesis for primary chest wall sarcoma. The site of the defect was anterolateral in 12 patients (46%) (Figure 2A,B), lateral in 6 patients (23%), posterior in 2 patients (8%), anterior (Figure 2C,D) in 5 patients (19%) and posterolateral in one patient (4%) (Table 2). Patients with chest trauma had a mean of 4.5 ribs fractures (range, 3–7). The average size of the defect was 9.3×7.8 cm (range, 4×3 to 20×15 cm). The median number of resected ribs was 3.6 (range, 3–7). The titanium mesh was trimmed from standard size of 20×14 cm. The 0.4 mm thick mesh was used in three patients: one case with an antero-inferior defect and two patients with lateral defects. In all the other patients, the 0.6 mm thick prosthesis was adopted. Table 3 summarizes the operative and postoperative outcomes. In case of large chest wall defects, in order to give more rigidity, titanium bars were placed above the mesh. Additional titanium bars and screws were used in 8 patients (31%): in lateral chest wall reconstruction in three patients, in anterior position in two patients, anterolateral in two patients and posterolateral in one patient. The mean number of bars was 1.8 per patient (range, 1–3 per patient). Mean operative time was 315 minutes (range, 70–659 minutes). Primary repair of the soft tissue (muscle and subcutaneous layers) and skin above the titanium mesh was performed in 19 patients (73%). Muscle-flap was required in 7 patients (27%): pectoralis major flap in five cases and latissimus dorsi muscle flap in two cases. Associated procedures were lung resection in 11 patients (42%), superior vena cava resection and reconstruction in one patient (4%), ascending aorta repair in one patient (4%) and one (4%) omentum transposition to the mediastinum. Thirteen patients (50%) after the operation were transferred in the intensive care unit as planned before surgery. No perioperative deaths occurred. The mean time to removal chest drains were 8.5 days (range, 5–13 days). The mean ICU stay was 9.3 days (range, 2–24 days). The mean in-Hospital stay was 11.9 days (range, 4–29 days). Major post-operative complications occurred in five patients (19%), including one re-exploration for bleeding (4%), two post-operative pneumothorax requiring drainage (8%) and one pulmonary embolism due to deep vein thrombosis (8%). Furthermore, during hospitalization, one patient who had lateral chest wall resection for T3 lung cancer, suffered of surgical wound suppuration treated with open debridement, antibiotics and VAC-therapy (8 days), but without need of implant removal. One patient, who was operated because of thoracic trauma, was readmitted in hospital 23 days after discharge because of fever, mild pleural effusion and peri-prosthetic fluid collection with dehiscence of the implanted mesh (Figure 3). This patient was treated with drainage of chest cavity and mesh reattachment with steel wires passed around the ribs followed by antibiotics without the need of prosthesis explant. He was discharged after 19 days in good clinical condition without clinical or radiological signs of infection and the subsequent follow-up was free of complications. We reported one case of 0.4 mm mesh fracture in antero-inferior position after four months from the operation treated conservatively. One patient, who underwent an anterolateral 4 ribs resection for chest wall sarcoma, complained of chronic thoracic pain at the follow-up interview. Oncological resection was radical in all patients except in one case (sarcomatoid lung carcinoma) with infiltration of surgical margins who underwent adjuvant radiotherapy. The mean follow-up was 22.4 months (median 21 months; range, 4–32 months) and no patient was lost during the follow-up period. Four patients died for tumor recurrence after a mean period of 16.8 months (range, 11–28 months) from the operation.
Full table
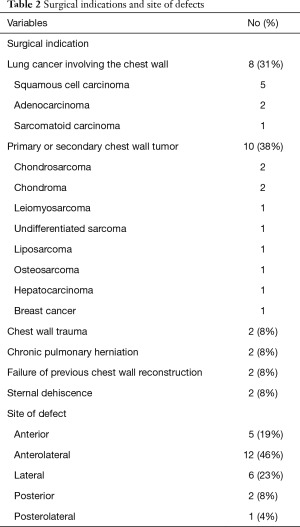
Full table
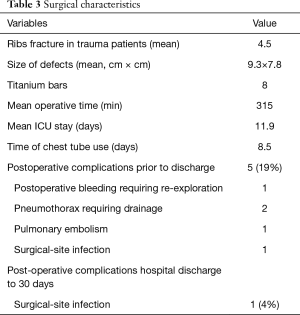
Full table
Discussion
Many surgical techniques have been described over the years, involving different materials for chest wall reconstruction or stabilization, but none of them are yet considered a gold standard procedure (2). The choice of the better method for the individual case is a matter of experience. What is mandatory, in particular after extensive chest wall resection for cancer or massive chest wall deformities after trauma, is to guarantee an optimal stabilization and support of the thoracic cage to avoid paradoxical respiratory movement and thus respiratory failure, pain, thoracic organs herniation or damage and then good cosmetic results. Generally, optimal results are achieved with a combination of rigid biological or synthetic materials and soft tissue coverage (2,4-9). Recently, there has been introduced for clinical use a new titanium mesh (MDF Medical S.r.l., Italy), to date only a few case reports have described its use (9,10). Titanium is a well know material for reconstructive surgery not only for the thorax. The most used titanium transformations are bars, plates and screws (2,11). Titanium is highly biocompatible with low density, resistant to corrosion, ductile, diamagnetic and compatible with magnetic resonance imaging (2,4,8,9). Titanium is as resistant as steel but 40% lighter; it weights 60% more than aluminum but with a double strength. All these positive features justify the large use of this material in surgery, moreover recently new 3D printed titanium prosthesis are applied with success in different surgical fields (12). We started to use titanium mesh in 2014 to reconstruct or stabilize chest wall defects with good results. In some case such as sternal reconstruction or huge chest wall defects the mesh was reinforced with a variable number of titanium bars (Figure 4A) (4). In our experience, we had only one mesh fracture 4 months after implantation. In this case, the mesh used was a 0.4 mm thick implanted on the antero-inferior portion of the thorax cage. Probably, the continuous stress on the mesh related to the flexion and rotation torso and the thickness too thin are the causes of the failure. Berthet et al. (11) reported that after the chest wall stabilization with titanium implants, there was a prevalence of rupture in the anterior and lower position. The authors hypothesized that this may be related to the substantial displacement of the rib cage during inspiration in the cranial, lateral and ventral directions. In all cases we cover the titanium implant with well-vascularized surrounding tissue (muscles and subcutaneous tissue) whenever possible or muscular/musculocutaneous flap when indicated (Figure 4B). In our opinion, it’s very important to improve stability, to bring vascularized tissue preventing infections, to guarantee the tropism of subcutaneous and cutaneous tissue, avoid prosthesis decubitus on the skin and to achieve better cosmetic results. Unfortunately, despite these measures, we had two cases (8%) of surgical wound infection one early and one late after surgery. Both cases were treated with open drainage, targeted antibiotic and VAC therapy in the earlier case, but without removing the titanium mesh “a priori”. In fact, among the synthetic materials used for the reconstruction of the chest wall, titanium is the most resistant to bacterial colonization as reported in animal and human studies (13,14). The specific surface/interface design of titanium is known to make the surface of biomaterial less interactive (15). Lans et al. (16) reported 41 of the 220 patients (18.6%) with postoperative wound infection or wound necrosis after chest wall surgery. Berthet et al. reported very promising results using titanium bars for rib osteosynthesis in infected operative site (17). Therefore, our results describe a relatively acceptable risk to leave the mesh in an infected site when the surrounding tissue were judged well vascularized or when VAC therapy was applied to improve tissue vascularization. Obviously, we were ready to remove it in case of infection worsening. Weyant et al. (18) in a large series of chest wall reconstruction using methyl methacrylate sandwich or non-rigid repair reported an incidence of surgical wound infection about 5.3% but only 3.8% required the prosthesis removal. In the second of these patients the mesh became dehiscent due to fixing failure. In this case we used braided non- absorbable stitches (size-1) that was cut from the mesh itself. This complication has never happened again using non-absorbable monofilament suture (size-1 or -2) or using steel wires.
Limitations
This study was unavoidably limited by its retrospective nature and by the small sample size. Furthermore, the study population was heterogeneous, including patients with both traumatic as well as neoplastic causes. Furthermore, the surgical stabilization was performed using additional titanium bars based on the surgeon’s preference.
Conclusions
In conclusion, we find this new product very useful for chest wall repair or stabilization. This mesh has excellent biomechanical characteristics between rigid and malleable materials, it’s easy to trim and fix for optimal adaptation without necessity of dedicated instruments and is magnetic resonance compatible with minimal diffraction and artifact during computed tomography. The intrinsic resistance of titanium to bacterial colonization is also a feature that makes this material very useful for thoracic wall reconstruction even in potentially infected site such as post sternotomy sternal dehiscence. Moreover, in very complex cases, based on CT scan images, it is possible to order a custom-tailored mesh for dimension and thickness based in 3D printing model.
Acknowledgments
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. This retrospective multicenter study was approved by the Institutional Review Board of Ferrara S. Anna Hospital (No. CTOOB-3-F) and implemented and approved by the other centers committees, the written informed consent was obtained from all patients.
References
- Geissen NM, Medairos R, Davila E, et al. Number of Ribs Resected is Associated with Respiratory Complications Following Lobectomy with en bloc Chest Wall Resection. Lung 2016;194:619-24. [Crossref] [PubMed]
- Sanna S, Brandolini J, Pardolesi A, et al. Materials and techniques in chest wall reconstruction: a review. J Vis Surg 2017;3:95. [Crossref] [PubMed]
- Tensini I. Sopra il mio nuovo processo di amputazione della mammella. Gazzetta Med Ital 1906;57:141-2.
- Dell'Amore A, Cassanelli N, Dolci G, et al. An alternative technique for anterior chest wall reconstruction: the sternal allograft transplantation. Interact Cardiovasc Thorac Surg 2012;15:944-7. [Crossref] [PubMed]
- Mansour KA, Thourani VH, Losken A, et al. Chest wall resections and reconstruction: a 25-year experience. Ann Thorac Surg 2002;73:1720-5; discussion 1725-6.
- Deschamps C, Tirnaksiz BM, Darbandi R, et al. Early and long-term results of prosthetic chest wall reconstruction. J Thorac Cardiovasc Surg 1999;117:588-91; discussion 591-2. [Crossref] [PubMed]
- Leuzzi G, Nachira D, Cesario A, et al. Chest wall tumors and prosthetic reconstruction: A comparative analysis on functional outcome. Thorac Cancer 2015;6:247-54. [Crossref] [PubMed]
- Marulli G, Dell'amore A, Calabrese F, et al. Safety and Effectiveness of Cadaveric Allograft Sternochondral Replacement After Sternectomy: A New Tool for the Reconstruction of Anterior Chest Wall. Ann Thorac Surg 2017;103:898-905. [Crossref] [PubMed]
- Iarussi T, Pardolesi A, Camplese P, et al. Composite chest wall reconstruction using titanium plates and mesh preserves chest wall function. J Thorac Cardiovasc Surg 2010;140:476-7. [Crossref] [PubMed]
- Dell'Amore A, Campisi A, Giunta D, et al. Surgical options to treat massive sternal defect after failed Robicsek procedure. J Thorac Dis 2018;10:E410-5. [Crossref] [PubMed]
- Berthet JP, Gomez Caro A, Solovei L, et al. Titanium Implant Failure After Chest Wall Osteosynthesis. Ann Thorac Surg 2015;99:1945-52. [Crossref] [PubMed]
- Aragón J, Pérez Méndez I. Dynamic 3D printed titanium copy prosthesis: a novel design for large chest wall resection and reconstruction. J Thorac Dis 2016;8:E385-9. [Crossref] [PubMed]
- Berthet JP, Solovei L, Tiffet O, et al. Chest-wall reconstruction in case of infection of the operative site: is there any interest in titanium rib osteosynthesis? Eur J Cardiothorac Surg 2013;44:866-74. [Crossref] [PubMed]
- Arens S, Schlegel U, Printzen G, et al. Influence of materials for fixation implants on local infection. An experimental study of steel versus titanium DCP in rabbits. J Bone Joint Surg Br 1996;78:647-51. [Crossref] [PubMed]
- Harris LG, Richards RG. Staphylococci and implant surfaces: a review. Injury 2006;37 Suppl 2:S3-14. [Crossref] [PubMed]
- Lans TE, van der Pol C, Wouters MW, et al. Complications in wound healing after chest wall resection in cancer patients; a multivariate analysis of 220 patients. J Thorac Oncol 2009;4:639-43. [Crossref] [PubMed]
- Berthet JP, Solovei L, Tiffet O, et al. Chest-wall reconstruction in case of infection of the operative site: is there any interest in titanium rib osteosynthesis? Eur J Cardiothorac Surg 2013;44:866-74. [Crossref] [PubMed]
- Weyant MJ, Bains MS, Venkatraman E, et al. Results of chest wall resection and reconstruction with and without rigid prosthesis. Ann Thorac Surg 2006;81:279-85. [Crossref] [PubMed]


