Acute kidney injury: a common prognostic condition for different pathogenetic triggers?
We read with great interest the editorials by Wang et al. (1) and Cagini et al. (2) on our recently published study focusing on acute kidney injury (AKI) after lung cancer surgery (3). We particularly appreciated the editorial consideration reserved for a topic, such as AKI, which is only apparently of relevance for nephrologists.
In our large study population, we prospectively demonstrated a close association between AKI occurrence and worse in-hospital outcomes in a specific surgical setting (lung cancer surgery), which has not been fully investigated thus far. Our findings were not unexpected as the detrimental impact of AKI on outcome has been consistently reported in several other medical and surgical settings. Therefore, it appears evident that, regardless of the patients’ characteristics, initial insult, and clinical context, AKI onset shares the same prognostic meaning and, as properly highlighted in the two editorials, should be appreciated and accurately looked for by all physicians, and not only by nephrologists.
The early identification of patients at high-risk for AKI is critical in all clinical settings, in order to implement preventive strategies that currently represent the only opportunity to minimize the risk of AKI development and its severity. Indeed, treatment of severe AKI with renal replacement therapy is only supportive. High-risk AKI patients can be usually identified on the bases of major determining factors related to the specific underlying acute disease or the scheduled therapeutic procedure and of other factors that seem to be shared by all different etiologically related AKI. For example, the extension of pulmonary resection predicted AKI in our cohort of patients undergoing lung surgery and it can be considered a peculiar AKI correlate of this kind of thoracic surgery (3). Similarly, the use of cardiopulmonary bypass and its duration are well-known risk factors for AKI in patients undergoing cardiac surgery (4). Moving to examples regarding the medical arena, unique risk factors for AKI in patients undergoing percutaneous coronary intervention are represented by the type and volume of administered contrast agent (5). A final example regards patients with acute myocardial infarction, in whom the location and the extent of cardiac injury have been shown to predict AKI (6).
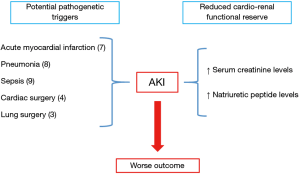
In addition to these risk factors, peculiar to each disease and/or therapeutic procedure, some other predictors are common to all clinical settings. Among them, baseline serum creatinine concentration, or estimated glomerular filtration rate, and levels of natriuretic peptides [B-type natriuretic peptide (BNP) and N-terminal proBNP] recur in all studies investigating them as clinical predictors of AKI, regardless of the context considered (Figure 1) (3,4,7-9). Indeed, in our study performed in lung cancer surgery, as well as in previous studies focusing on other clinical arenas, serum creatinine and natriuretic peptides accurately and independently predicted AKI. Moreover, in our study, when these two parameters were combined together, their pooled predictive accuracy significantly improved, allowing a better discrimination of AKI risk and, ultimately, a more appropriate allocation of patients in their risk category. Mechanisms underlying these observations have not been fully elucidated yet. However, a possible explanation can be proposed. Natriuretic peptides are neurohormones secreted by the ventricles in response to increased myocardial stretch, wall tension, or other myocardial stresses. Large-scale clinical trials have shown that they are elevated in patients with several cardiac diseases, and are powerful predictors of mortality. Moreover, in patients with chronic kidney disease, natriuretic peptides levels are increased due to both reduced renal clearance and augmented production. Therefore, they seem to be critical mediators in the cross-talk between heart and kidneys and their levels directly influenced by impairment in cardiac and/or renal function. On these premises, natriuretic peptides may summarize in a single parameter the clinical information independently provided by the two organs. Thus, it can be speculated that serum creatinine and natriuretic peptides values reflect cardio-renal functional reserve and that patients with high levels of both markers are particularly vulnerable to AKI because of their reduced capacity to adapt to unavoidable cardio-renal stresses induced by the specific triggers of each clinical setting (10).
In brief, AKI is more likely in patients with baseline cardio-renal vulnerability, as reflected by increased creatinine and natriuretic peptides levels, which may be caused by several pathogenetic triggers. Regardless of the precipitating causing factor, specific for each clinical condition, AKI seems to represent a common final pathway leading to a worse prognosis.
Acknowledgments
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
References
- Wang Z, Wang Y. Editorial on: “Acute kidney injury after lung cancer surgery: incidence and clinical relevance, predictors, and role of N-terminal pro B-type natriuretic peptide J Thorac Dis 2019;11:S1423-5. [Crossref] [PubMed]
- Cagini L, Andolfi M. N-terminal pro B-type natriuretic peptide and the risk of acute kidney injury after lung cancer surgery. J Thorac Dis 2018;10:6430-1. [Crossref] [PubMed]
- Cardinale D, Cosentino N, Moltrasio M, et al. Acute kidney injury after lung cancer surgery: Incidence and clinical relevance, predictors, and role of N-terminal pro B-type natriuretic peptide. Lung Cancer 2018;123:155-9. [Crossref] [PubMed]
- Patel UD, Garg AX, Krumholz HM, et al. Preoperative serum brain natriuretic peptide and risk of acute kidney injury after cardiac surgery. Circulation 2012;125:1347-55. [Crossref] [PubMed]
- Marenzi G, Assanelli E, Campodonico J, et al. Contrast volume during primary percutaneous coronary intervention and subsequent contrast-induced nephropathy and mortality. Ann Intern Med 2009;150:170-7. [Crossref] [PubMed]
- Marenzi G, Lauri G, Assanelli E, et al. Contrast-induced nephropathy in patients undergoing primary angioplasty for acute myocardial infarction. J Am Coll Cardiol 2004;44:1780-5. [Crossref] [PubMed]
- Moltrasio M, Cabiati A, Milazzo V, et al. B-type natriuretic peptide and risk of acute kidney injury in patients hospitalized with acute coronary syndromes. Crit Care Med 2014;42:619-24. [Crossref] [PubMed]
- Nowak A, Breidthardt T, Dejung S, et al. Natriuretic peptides for early prediction of acute kidney injury in community-acquired pneumonia. Clin Chim Acta 2013;419:67-72. [Crossref] [PubMed]
- Lentini P, de Cal M, Clementi A, et al. Sepsis and AKI in ICU Patients: The Role of Plasma Biomarkers. Crit Care Res Pract 2012;2012:856401. [Crossref] [PubMed]
- Moltrasio M, Cosentino N, De Metrio M, et al. Brain natriuretic peptide in acute myocardial infarction: a marker of cardio-renal interaction. J Cardiovasc Med (Hagerstown) 2016;17:803-9. [Crossref] [PubMed]