
An assessment of the distance between the phrenic nerve and major intrathoracic structures
Introduction
The phrenic nerves are the only motor innervation of the diaphragm; they also provide major sensory innervation to the central tendon of the diaphragm, mediastinal pleura, pericardium and some viscera of the upper abdomen. This pair of nerves descend through the thorax in close proximity to major structures such as the heart, pericardium, esophagus, vena cava, and aorta. Embryologically, phrenic axon projection is closely related to diaphragm primordium migration within the developing thorax; thus, adult variation may indicate unique diaphragmatic/thoracic development (1,2). Insight into variations in phrenic nerve position will provide physicians with essential anatomical information to reduce iatrogenic phrenic nerve injury during procedures that require intrathoracic intervention.
Each phrenic nerve innervates the ipsilateral half of the diaphragm and, if damaged, ipsilateral paralysis of the diaphragm will result in compromised pulmonary function (3). Phrenic nerve identification and preservation during invasive thoracic procedures are critical to prevent diaphragmatic impairment as well as other potential complications (4-6). Specifically, studies have shown a correlation in phrenic nerve injury to: (I) open heart coronary artery bypass grafting (4,7); (II) thoracic endovascular cardiac repair (8); (III) traditional cardiac repair (9); (IV) thoracic aortic aneurysm. Exploratory laparotomy has also been shown to cause phrenic nerve damage resulting in diaphragm paralysis (10). Phrenic nerve injury has also been documented secondary to thoracostomy tube placement (11,12).
With increasing use of minimally invasive procedures that limit direct visualization of the phrenic nerve, such as laparoscopy and endoscopy, it is of extreme importance to recognize the proximity of the phrenic nerves to major thoracic structures to prevent complicating patient outcomes. A recent study has provided data on phrenic nerve position relative to upper thoracic structures in the context of limiting complications from cardiac intervention (13). The purpose of this study was to assess the site of diaphragmatic innervation by the phrenic nerves relative to lower thoracic structures in order to provide positional data critical to thoracic surgeons that perform laparotomy, laparoscopic, and other invasive procedures.
Methods
Subjects
This study was performed using deidentified human cadavers and as these are not considered human subjects by our institution, institutional review board approval was not needed. Dissection of the thoracic cavity was performed bilaterally on 43 embalmed human cadavers (25 males; 18 females) at Edward Via College of Osteopathic Medicine, Virginia and Carolina campuses. Data was gathered from 43 cadavers; 33 left phrenic nerves and 40 right phrenic nerves were intact. The specimens consisted of 41 Caucasians and 2 African Americans.
Design
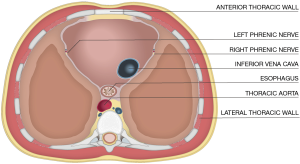
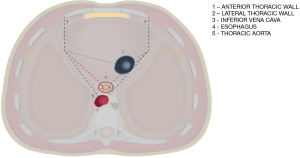
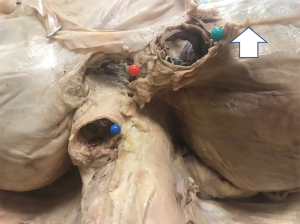
The site of phrenic nerve penetration into the diaphragm was identified then designated by a pin. The distances were measured from each phrenic nerve to surgically relevant thoracic cavity structures: (I) lateral wall of the inferior vena cava (IVC); (II) esophagus; (III) descending aorta; (IV) lateral thoracic wall; (V) anterior thoracic wall (Figure 1). The external surface of these structures was pinned at the closest distance to the phrenic nerve diaphragmatic insertion. Calipers were then used to measure the distance from each phrenic nerve as it enters the diaphragm to each thoracic structure (Figures 2,3). Thoracic horizontal distance, defined as the distance from right lateral rib cage to left lateral rib cage at the level of the diaphragm, was taken to standardize phrenic nerve location due to individual size differences. Measurements were taken by multiple investigators to ensure accuracy.
Statistical analysis
Continuous data were analyzed and tested for normality using means ± standard deviation for each variable. Quantitative analyses comparing males with females was performed using unpaired t test for those variables that were normally distributed, and the Wilcoxon Sum Rank Test was used for non-normal comparisons. The level of significance was set at the 0.05 level.
Results
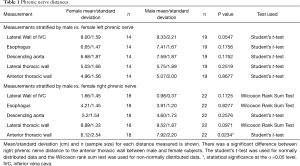
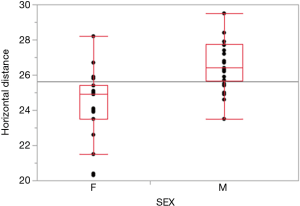
Analyses of male/female mean, standard deviation and sample size (n) according to left and right phrenic nerves are represented in Table 1. As expected, the mean thoracic horizontal diameter of male cadavers was significantly larger than that of female cadavers (P value <0.0001) (Figure 4). Due to statistically greater thoracic cavity diameter in males, distances from phrenic nerves to visceral structures were expected to be greater in males. However, there was no statistically significant difference between the males and females except at the right phrenic nerve to anterior thoracic wall distance (male 7.92 cm; female 6.12 cm; P value =0.0234).
Full table
Discussion
Knowledge of variation of phrenic nerve location in the thorax is essential to reduce the incidence of iatrogenic injury during invasive procedures, especially in situations without the opportunity to assess these patterns before intervention. The phrenic nerve is of special interest since it courses deep in the thorax, is critical for diaphragm function and is situated in close proximity to major thoracic structures critical to life. Variation in phrenic nerve proximity to major thoracic structures has been documented (13); however, to our knowledge, no study has been conducted to assess variation in the distance between phrenic nerve penetration of the diaphragm and the distances to major thoracic structures.
Our data revealed that there was no statistically significance difference between males and females in regards to both phrenic nerve distances to the IVC, aorta and esophagus. Since it was shown that thoracic wall diameter was statistically larger in males versus females (P value <0.0001), we expected that males would have a greater distance between the phrenic nerves and major thoracic structures. However, this was not the case and the only significant relationship identified was the right phrenic nerve being at a greater intrathoracic depth from the anterior thoracic wall in males. The right phrenic nerves increased intrathoracic depth in males may cause it to be within proximity of visceral thoracic structures and expose it to damage associated with pathology such as aortic aneurysm. It has been reported that right phrenic nerve palsy may occur due to thoracic aortic aneurysm in males and this may be due to the closer proximity of the right phrenic nerve in males to the thoracic aorta (14). This possible correlation between right phrenic palsy due to aortic aneurysm and right phrenic nerve intrathoracic depth was a unique finding in our investigation and to our knowledge has not been documented in scientific literature previously. Future studies comparing the incidence of right phrenic nerve palsy in males and females due to thoracic aortic aneurysm would provide important information for thoracic surgeons.
The goal of this study was to provide thoracic interventionalists with baseline data regarding phrenic nerve proximity to thoracic structures in order to prevent iatrogenic nerve injury during surgery. Although many procedures may result in nerve damage, chest tube placement is one of the most commonly performed procedures in hospital and phrenic nerve injury has been associated with mal placement (11). It has been recommended to use ultrasound guided thoracostomy tube placement as this may improve patient outcomes by lowering incidence of phrenic nerve palsy (15). If phrenic nerve palsy is suspected, immediate partial withdrawal may reduce impairment of hemidiaphragm function (16). As demonstrated in this study, phrenic nerve distance from the lateral thoracic wall may allow for better estimates regarding proper tube insertion depth; and could reduce incidence of nerve injury, especially in patients where ultrasound guided technique is inadequate.
In sum, this study provides data on phrenic nerve proximity to major thoracic structures that may be used to lower incidence of nerve injury during thoracic intervention. To note, even though males had significantly larger thoracic diameter than females; the only significant difference was that males had greater depth to the right phrenic nerve as measured from the anterior thoracic wall. This may explain an increase incidence of right phrenic nerve palsy in males with aortic and visceral pathology when compared to females and warrants further investigation.
Acknowledgments
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. This study was performed using deidentified human cadavers and institutional review board approval was not needed.
References
- Merrell AJ, Ellis BJ, Fox ZD, et al. Muscle connective tissue controls development of the diaphragm and is a source of congenital diaphragmatic hernias. Nat Genet 2015;47:496-504. [Crossref] [PubMed]
- Sefton EM, Gallardo M, Kardon G. Developmental origin and morphogenesis of the diaphragm, an essential mammalian muscle. Dev Biol 2018;440:64-73. [Crossref] [PubMed]
- Xu WD, Gu YD, Lu JB, et al. Pulmonary function after complete unilateral phrenic nerve transection. J Neurosurg 2005;103:464-7. [Crossref] [PubMed]
- Aguirre VJ, Sinha P, Zimmet A, et al. Phrenic nerve injury during cardiac surgery: mechanisms, management and prevention. Heart Lung Circ 2013;22:895-902. [Crossref] [PubMed]
- McAlister VC, Grant DR, Roy A, et al. Right phrenic nerve injury in orthotopic liver transplantation. Transplantation 1993;55:826-30. [Crossref] [PubMed]
- Sheridan PH Jr, Cheriyan A, Doud J, et al. Incidence of phrenic neuropathy after isolated lung transplantation. The Loyola University Lung Transplant Group. J Heart Lung Transplant 1995;14:684-91. [PubMed]
- Canbaz S, Turgut N, Halici U, et al. Electrophysiological Evaluation of Phrenic Nerve Injury during Cardiac Surgery – a Prospective, Controlled, Clinical Study. BMC Surg 2004;4:2. [Crossref] [PubMed]
- Matsumura JS, Lee WA, Mitchell RS, et al. The Society for Vascular Surgery Practice Guidelines: management of the left subclavian artery with thoracic endovascular aortic repair. J Vasc Surg 2009;50:1155-8. [Crossref] [PubMed]
- Peterson BG, Eskandari MK, Gleason TG, et al. Utility of left subclavian artery revascularization in association with endoluminal repair of acute and chronic thoracic aortic pathology. J Vasc Surg 2006;43:433-9. [Crossref] [PubMed]
- Summerhill EM, El-Sameed YA, Glidden TJ, et al. Monitoring Recovery from Diaphragm Paralysis with Ultrasound. Chest 2008;133:737-43. [Crossref] [PubMed]
- Kwiatt M, Tarbox A, Seamon MJ, et al. Thoracostomy Tubes: A Comprehensive Review of Complications and Related Topics. Int J Crit Illn Inj Sci 2014;4:143-55. [PubMed]
- Nahum E, Ben-Ari J, Schonfeld T, et al. Acute Diaphragmatic Paralysis Caused by Chest-Tube Trauma to Phrenic Nerve. Pediatr Radiol 2001;31:444-46. [Crossref] [PubMed]
- Sánchez-Quintana D, Cabrera JA, Climent V, et al. How Close Are the Phrenic Nerves to Cardiac Structures? Implications for Cardiac Interventionalists. J Cardiovasc Electrophysiol 2005;16:309-13. [Crossref] [PubMed]
- Akhtar J, Siddiqui MA, Khan NA, et al. Right Phrenic Nerve Palsy: A Rare Presentation of Thoracic Aortic Aneurysm. Malays J Med Sci 2013;20:98-101. [PubMed]
- Laws D, Neville E, Duffy J. BTS guidelines for the insertion of a chest drain. Thorax 2003;58 Suppl 2:ii53-9. [Crossref] [PubMed]
- Salon JE. Reversible Diaphragmatic Eventration Following Chest Tube Thoracostomy. Ann Emerg Med 1995;25:556-8. [Crossref] [PubMed]


