
The clinical significance of the intraoperative pathological examination of bilateral recurrent laryngeal nerve lymph nodes using frozen sections in cervical field lymph node dissection of thoracic esophageal squamous cell carcinoma
Introduction
Advances have recently been made in the development of comprehensive therapies for patients with esophageal cancer including surgery, leading to improved survival rates. However esophageal cancer is still one of the deadliest diseases of digestive tract malignant tumors (1,2). For patients with resectable esophageal cancer, surgery is still the optimal treatment option (3). At home and abroad, the 5-year overall survival rate after conventional esophagectomy is only 20–30% (4), and determination of lymph node (LN) metastasis is a key prognostic factor (5). At present, the range of LN dissection remains controversial. Two-field and three-field LN dissections have been the two most commonly used LN clearance methods in surgical operations. Three-field LN dissection has been the standard procedure for LN dissection in patients with esophageal cancer in some hospitals (6), and has been shown to significantly improve prognosis compared with two-field LN dissection. However, the high incidence rate of postoperative complications caused by three-field LN dissection cannot be completely avoided (7). Therefore, there has always been a debate about whether radical three-field LN dissection should be performed on all patients with esophageal cancer.
Previous studies have shown that esophageal cancer has a high rate of LN metastasis to the recurrent laryngeal nerve LNs, In light of their special location, some researchers have speculated that the bilateral recurrent laryngeal nerve LNs are sentinel nodes of the cervical LNs (8-10), and the decision on whether to perform three-field LN dissection may be determined by studying the relationship between the states of the bilateral recurrent laryngeal nerve LNs and cervical LNs. However, there are still few reports describing the relationship between the intraoperative pathological examinations of left recurrent laryngeal nerve LN, right recurrent laryngeal LN and cervical LN metastases using frozen sections We retrospectively analyzed data from a single center to determine if left or right recurrent laryngeal nerve LN metastasis could be used to predict cervical LN metastasis and thus guide the most appropriate LN dissection.
Methods
General information
We collected clinicopathological data from 69 patients with esophageal squamous cell carcinoma who had undergone intraoperative pathological examination of bilateral recurrent nerve LNs using frozen sections and three-field LN dissection in the Fujian Medical University Union Hospital from December 2015 to April 2018. These patients were diagnosed with esophageal squamous cell carcinoma, using an electronic gastroscope, prior to surgery. Each patient underwent esophagography, chest and abdomen computed tomography (CT) scans, ultrasonography of the abdomen, neck, and clavicle, and ultrasonic gastroscopy, as well as positron emission tomography-CT (PET-CT) scans when needed.
The inclusion criteria for this study were as follows: the lesion was located in the thoracic segment with cT1-3, N0-1 and M0 preoperative staging; there was no distant metastasis; and preoperative evaluation was feasible for minimally invasive surgery; except for other malignancies; no preoperative chemotherapy or radiotherapy; no combined with severe diseases of the heart, liver, lung or kidney disease, no other surgical contraindications; patients could tolerate surgical treatment. The study was approved by the Ethics Committee of Fujian Medical University (No. 2016YF020-02) and all participants gave informed consent before taking part.
The sample comprised 14 women and 55 men, and the average age was 59.9±7.2 years. To compare the complications of three-field with two-field LN dissections, we collected data on 104 patients with two-field LN dissection in our hospital that met the same inclusion criteria as those patients with three-field LN dissection, and compared postoperative complications between the two groups (Table 1).

Full table
Surgical procedures
The scope of dissection in three-field LN dissection included neck, chest, and abdomen. The specific surgical procedures were as follows: insert a single-lumen endotracheal tube, move the patient to the left-prone position (135 degrees), first dissect the middle and lower thoracic esophagus, deal with the inherent oesophageal arteries, dissect the oesophagus up to the T2 level of the thoracic cage, dissect the oesophagus down to the oesophageal hiatus, complete dissecting the oesophagus, expose and protect the right recurrent laryngeal nerve, dissect the right recurrent laryngeal nerve and thoracic paraoesophageal LNs, suspend the oesophageal mesangium, anatomically expose the left recurrent laryngeal nerve, dissect the LNs of the left recurrent laryngeal nerve, dissect the LNs under the carina and completely stop bleeding. Place the patient in the supine and separated leg position for abdominal surgery. Next, expose the small bend in the stomach; deal with the left gastric artery, the back of the stomach and the short gastric artery; meanwhile, dissect the perigastric LNs, separate the oesophageal hiatus and dissect the abdominal oesophagus. Make an incision in the medial margin of the sternocleidomastoid muscle of the left cervical oesophagus, separate the sternocleidomastoid, dissect the LNs in the left lower cervical oesophagus [included left cervical paraesophageal (101) and supraclavicular (104)] and divide the cervical oesophagus. Make an incision in the centre of the abdomen, remove the stomach and shape it into a tube, lift the stomach to the left cervical oesophagus, by way of the oesophageal hiatus and oesophageal bed, to introduce a mechanical anastomosis. Then make an incision in the medial margin of the sternocleidomastoid muscle of the right cervical oesophagus and dissect the LNs in the right lower cervical oesophagus [included right cervical paraesophageal (101) and supraclavicular (104)]. The left and right thoracic recurrent laryngeal nerve LNs were routinely subjected to intraoperative frozen section pathological examination. All LNs were histologically examined using hematoxylin and eosin staining, and pathological reports were obtained from the pathology department.
Grouping of LNs
LN group was established according to the standards of the Japanese Esophageal Cancer Research Group (11). Cervical LNs dissected included cervical paraesophageal (101) and supraclavicular (104). The dissected mediastinal LNs included the upper thoracic paraesophageal (105), thoracic paratracheal (106), subcarinal (107), middle thoracic paraesophageal (108), main bronchus (109), lower thoracic paraesophageal (110), supradiaphragmatic (111), and posterior mediastinal (112). Adjacent LNs (group 106) of the recurrent laryngeal nerves were included in the thoracic paratracheal LNs. Dissected abdominal LNs included the right paracardial (1), left paracardial (2), gastric small bend LNs (3), as well as LNs along the left gastric artery (7), common hepatic artery (anterosuperior group) (8a), and celiac artery (9), as well as LNs at the splenic hilum (10).
Statistical methods
Data were analysed using SPSS 22.0 software. Measured data were expressed as mean ± standard deviation (SD) and differences between groups were analysed by t-tests. Counted data were expressed as number or percent, and differences were analysed using χ2 or Fisher’s exact tests. Univariate logistic regression analysis was carried out to analyze factors that might have affected cervical LN metastasis, and those factors (P<0.05) were further analyzed using multivariate logistic regression. P<0.05 was considered statistically significant.
Results
Relationship between intraoperative frozen and postoperative pathology of recurrent laryngeal nerve LNs
Eleven patients had positive left recurrent laryngeal nerve LNs according to intraoperative frozen pathology, and all these were confirmed as metastatic by postoperative pathology. Fifty-eight patients had negative left recurrent laryngeal nerve LNs by intraoperative frozen pathology, and no LN metastasis was detected in any of these cases by postoperative pathology. The accuracy of intraoperative frozen diagnosis was therefore 100%. Twenty-one patients were positive for right recurrent laryngeal nerve LNs according to intraoperative frozen pathology, all of which were confirmed as metastatic by postoperative pathology. Forty-eight cases were negative for right recurrent laryngeal nerve LNs by intraoperative frozen pathology, one of which showed LN metastasis on postoperative pathology. The accuracy of frozen pathology for detecting right recurrent laryngeal nerve LNs was therefore 98.6%.
LN dissection and metastasis
A total of 1,195 cervical LNs were dissected from 69 patients, with an average of 17.3 LN dissections per patient. Twenty-eight (2.3%) cases had LN metastasis and 15.9% (11/69) of patients had metastasis in the cervical LNs. A total of 552 recurrent laryngeal nerve LNs were dissected, with an average of 8.0 LN dissections per patient. 58 (10.5%) cases had LN metastasis and the rate of recurrent laryngeal nerve LN metastasis was 34.8% (24/69).
Relationships among depth of infiltration, tumor location, and cervical LN metastasis
A total of 15 patients were pathological T1, 8 were T2, 46 were T3, and none were T4. With an increased T stage, the cervical LN metastatic rate also gradually increased. The cervical LN metastatic rate was 6.7% (1/15), 12.5% (1/8), and 19.6% (9/46) in patients with pathological T1, T2, and T3, respectively, although statistical significance was not reached (Table 2). There were 5 cases of tumors located in the upper thoracic segment, 52 cases located in the middle thoracic segment, and 12 cases located in the lower thoracic segment. When the tumor was located in the middle of the thoracic region, the cervical LN metastatic rate was 17.3% (9/52), and it was 16.7% (2/12) when the tumor was located in the lower thoracic segment. When the tumor was in the upper thoracic segment, no cervical LN metastasis occurred, there was no statistically significant difference in metastatic rate between thoracic regions (Table 3).

Full table

Full table
Relationship between recurrent laryngeal nerve LN and cervical LN metastasis
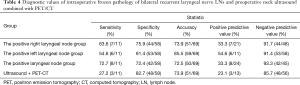
The metastatic rate of cervical LNs with metastasis in the right laryngeal recurrent nerve LN was 33.3% (7/21), while the rate without metastasis was 8.3% (4/48), the difference was statistically significant (P=0.036), and the sensitivity, specificity, accuracy, positive predictive value, and negative predictive value were: 63.6%, 75.9%, 73.9%, 33.3%, and 91.7%, respectively. The metastatic rate of cervical LNs with metastasis in the left laryngeal nerve LN was 54.6% (6/11), while the rate without metastasis was 8.6% (5/58) (P=0.016), and the sensitivity, specificity, accuracy, positive predictive value, and negative predictive value were 54.6%, 91.4%, 85.5%, 54.6%, and 91.4%, respectively. The metastatic rate of cervical LNs with metastases in one of the recurrent laryngeal nerve LNs (left or right recurrent laryngeal nerve LN was positive) was 33.3% (8/24), while the rate without metastasis was 6.7% (3/45) (P=0.017), and the sensitivity, specificity, accuracy, positive predictive value, and negative predictive value were 72.7%, 72.4%, 72.5%, 33.3%, and 93.3%, respectively. The metastatic rate of cervical LNs with metastases in the bilateral recurrent laryngeal nerve LNs was 62.5% (5/8). During the same period, we also measured the sensitivity, specificity, accuracy, positive predictive value, and negative predictive value of preoperative routine cervical ultrasonography combined with PET-CT examination for cervical LN metastasis, and the values were 27.2%, 82.7%, 73.9%, 23.1%, and 85.7%, respectively (Table 4). The results showed that the intraoperative pathological examination of the left recurrent laryngeal nerve LN using frozen sections had the highest accuracy for cervical LN metastasis, and that the intraoperative pathological examination of the bilateral recurrent laryngeal nerve LNs using frozen sections had the highest negative predictive value (Table 4). When the tumor was in the middle and lower segment of the esophagus, the metastatic rate of cervical LNs was high if recurrent laryngeal nerve LNs were positive; the metastatic rate of cervical LNs was low if the recurrent laryngeal nerve LNs were negative, and the difference was statistically significant (P=0.004) (Table 5).
Full table

Full table
Metastasis-related factors
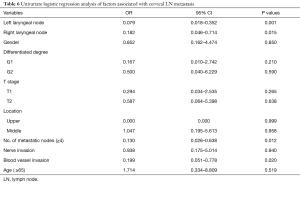
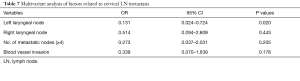
Univariate analysis identified metastasis to the left and right recurrent laryngeal nerve LNs, metastasis number (mediastinal LN + abdominal LN: metastasis number ≥4), and blood vessel invasion as factors associated with cervical LN metastasis (Table 6). Multivariate analysis identified metastasis to the left recurrent laryngeal nerve LNs was the only independent predictor of cervical LN metastasis (P<0.05) (Table 7).
Full table
Full table
Postoperative complications
Incidences of pulmonary infection, chylothorax, anastomotic leakage, and hoarseness were 18.8% (13/69), 2.9% (2/69), 2.9% (2/69), and 8.7% (6/69), respectively. The incidence of postoperative complications was slightly higher in patients who received three-field compared with two-field LN dissection in our hospital during the same period, but the difference was not significant (Table 8).

Full table
Discussion
Lymphatic metastasis is an important metastatic pathway in patients with esophageal carcinomas. The esophageal submucosa includes abundant LNs and longitudinal lymphatic networks (12), and early esophageal cancer invasion into the submucosa may thus have multiple metastatic LN stations (13). Cancer cells can be transferred along with the complex LN system, with the possibility of jump metastasis (3). Regarding radical tumor resection, patients with esophageal cancer require three-field LN radical resection, which helps to improve the accuracy of staging, guiding subsequent treatment, reducing postoperative tumor recurrence, and improving the survival rate of patients. However, compared with two-field LN dissection, three-field LN dissection is a more complicated surgical procedure that requires longer time and exposes the patient to greater trauma. The high rate of postoperative complications, including recurrent laryngeal nerve injury, anastomotic leakage, chylothorax and pulmonary infection, cannot be completely avoided (7,14,15). However, rates of metastasis to the cervical LNs differ depending on the location of the esophageal cancer; the incidence of metastasis to the thoracic esophageal neck LNs was significantly higher in patients with cancer of the upper esophagus compared with cancer of the middle or lower regions, and the necessity of neck LN removal also differed (16). Therefore, paying attention to individualized LN removal and selectively removing only those LNs deemed necessary can help some patients avoid unnecessary trauma, resulting in fewer postoperative complications.
Previous studies showed that the rate of cervical LN metastasis in patients with esophageal cancer was 16–43% and the recurrence rate is 6–16% (17,18). The ability to predict and detect cervical LN metastasis is thus key to improving surgical efficacy in patients with esophageal carcinomas. Previous studies reported that recurrent laryngeal nerve LNs are the common metastatic site of thoracic esophageal carcinomas, and studies have reported that the rate of metastasis to recurrent laryngeal nerve LNs in esophageal cancer is 18–43% (10,19-21). The recurrent laryngeal nerve LNs are located at the junction of the neck and chest, leading some to suggest these LNs may act as sentinel LNs of the neck. Based on intraoperative frozen section pathological examination of recurrent laryngeal nerve LNs, the scope of LN dissection can be determined, which can reduce complications caused by unnecessary removal. The cervical LN metastasis rate in the current study was 33.3% (8/24) in patients with recurrent laryngeal nerve LN metastasis, which was significantly higher than in patients without LN metastasis [6.7% (3/45)] (P=0.017). Analysis of subgroups found that when the tumor was in the middle or lower segment, and a recurrent laryngeal nerve LN was positive, the cervical LN metastatic rate was higher. Conversely, when a recurrent laryngeal nerve LN was negative, the cervical LN metastatic rate was lower (P=0.004). The predictive value of recurrent laryngeal nerve LN metastasis was more evident when the tumor was located in the middle or lower esophagus, in accord with the results of Ma et al. and Shiozaki et al. (3,9). In contrast, upper thoracic esophageal carcinomas are located close to the neck, making it easy for cells to pass through the lymphatic vessels at the junction of the neck and chest, leading to early cervical LN metastasis in the absence of recurrent laryngeal nerve LN metastasis. The Chinese Society of Esophageal Cancer, Chinese Anti-Cancer Association 2011 clinical practice guidelines for the diagnosis and treatment of esophageal cancer clearly indicated that patients with upper thoracic esophageal cancer should undergo three-field LN dissection (22), while Japanese scholars also recommend that supraclavicular LN dissection for upper thoracic esophageal cancer (23). In the current study, there was no cervical LN metastasis in patients with an upper thoracic esophageal carcinoma (0/5), which may be related to the small number of cases available and selection bias.
Recurrent laryngeal nerve LNs have previously been reported to have predictive value for cervical LN metastasis, and bilateral recurrent laryngeal nerve LNs was considered as a single variable in statistical analysis (9,24), however the relationships between frozen pathology results for the left or right recurrent laryngeal nerve LNs respectively, and cervical LN metastasis remain unclear. According to the current data, the left recurrent laryngeal nerve LN had the highest accuracy for predicting cervical LN metastasis, which was 85.5%, and that the intraoperative pathological examination of the bilateral recurrent laryngeal nerve LNs using frozen sections had the highest negative predictive value, which was 93.3%, multivariate analysis was performed and only metastasis to the left recurrent laryngeal LN was determined to be an independent risk factor for cervical LN metastasis (P=0.02), while metastasis to the right recurrent laryngeal nerve LNs was not (P=0.443).
This study has the following limitations: first, the design of this study was retrospective, and there may have been a risk of selection bias, however all the enrolled patients strictly met the inclusion criteria, thus reducing this risk. Second, this study only included a small number of cases and further prospective multicenter studies with larger sample sizes are needed to confirm the predictive value of intraoperative pathological examination of the right and left laryngeal nerve LNs using frozen sections.
Previous reports have indicated that postoperative complications were more likely to occur following three-field LN compared with two-field LN dissections; however, with improvements in perioperative care and surgical techniques, the incidence of postoperative complications in patients with esophageal cancer has been reduced to some extent (25). Although the current study found more postoperative complications with three-field LN compared with two-field LN dissections, the difference was not statistically significant.
In conclusion, intraoperative pathological examination of the left recurrent laryngeal nerve LNs using frozen sections has some value for predicting cervical LN metastasis, and can be used as a reference standard for guiding on cervical-field LN dissection. If intraoperative frozen section pathological examination is positive, we can decide whether three-field LN dissection should be performed combined with preoperative examination, tumor location, and other factors, some patients can avoid unnecessary trauma, reduce postoperative complications. However, further follow-up is needed to evaluate local postoperative recurrence rates and long-term survival rates.
Acknowledgments
We thank Mark Abramovitz, PhD, from Liwen Bianji (Edanz Group, China; www.liwenbianji.cn/ac), for editing the English text of a draft of this manuscript.
Funding: The study was supported by Fujian Provincial Key Project (2014Y0024) and Fujian Provincial Joint Research Project of Health Care and Education (WKJ2016-2-09).
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was approved by the Ethics Committee of Fujian Medical University (No. 2016YF020-02) and all participants gave informed consent before taking part.
References
- Li H, Yang S, Zhang Y, et al. Thoracic recurrent laryngeal lymph node metastases predict cervical node metastases and benefit from three-field dissection in selected patients with thoracic esophageal squamous cell carcinoma. J Surg Oncol 2012;105:548-52. [Crossref] [PubMed]
- Chen WQ, Zheng RS, Zhang SW, et al. Report of Cancer Incidence and Mortality in China, 2013. J Bulletin of Chinese Cancer 2017;26:1-7.
- Ma L, Xiang J, Zhang Y, et al. Characteristics and clinical significance of recurrent laryngeal nerve lymph node metastasis in esophageal squamous cell carcinoma. J BUON 2017;22:1533-9. [PubMed]
- Straatman J, Joosten PJ, Terwee CB, et al. Systematic review of patient-reported outcome measures in the surgical treatment of patients with esophageal cancer. Dis Esophagus 2016;29:760-72. [Crossref] [PubMed]
- Cho JW, Choi SC, Jang JY, et al. Lymph node metastases in esophageal carcinoma: an endoscopist’s view. Clin Endosc 2014;47:523-9. [Crossref] [PubMed]
- Udagawa H, Ueno M, Shinohara H, et al. The importance of grouping of lymph node stations and rationale of three-field lymphoadenectomy for thoracic esophageal cancer. J Surg Oncol 2012;106:742-7. [Crossref] [PubMed]
- Matsuda S, Takeuchi H, Kawakubo H, et al. Three-field lymph node dissection in esophageal cancer surgery. J Thorac Dis 2017;9:S731-40. [Crossref] [PubMed]
- Taniyama Y, Nakamura T, Mitamura A, et al. A strategy for supraclavicular lymph node dissection using recurrent laryngeal nerve lymph node status in thoracic esophageal squamous cell carcinoma. Ann Thorac Surg 2013;95:1930-7. [Crossref] [PubMed]
- Shiozaki H, Yano M, Tsujinaka T, et al. Lymph node metastasis along the recurrent nerve chain is an indication for cervical lymph node dissection in thoracic esophageal cancer. Dis Esophagus 2001;14:191-6. [Crossref] [PubMed]
- Taniyama Y, Miyata G, Kamei T, et al. Complications following recurrent laryngeal nerve lymph node dissection in oesophageal cancer surgery. Interact Cardiovasc Thorac Surg 2015;20:41-6. [Crossref] [PubMed]
- Pennathur A, Gibson MK, Jobe BA, et al. Oesophageal carcinoma. Lancet 2013;381:400-12. [Crossref] [PubMed]
- Liebermann-Meffert D. Anatomical basis for the approach and extent of surgical treatment of esophageal cancer. Dis Esophagus 2001;14:81-4. [Crossref] [PubMed]
- Mizutani M, Murakami G, Nawata S, et al. Anatomy of right recurrent nerve node: why does early metastasis of esophageal cancer occur in it? Surg Radiol Anat 2006;28:333-8. [Crossref] [PubMed]
- Ye T, Sun Y, Zhang Y, et al. Three-field or two-field resection for thoracic esophageal cancer: a meta-analysis. Ann Thorac Surg 2013;96:1933-41. [Crossref] [PubMed]
- Ma GW, Situ DR, Ma QL, et al. Three-field vs two-field lymph node dissection for esophageal cancer: a meta-analysis. World J Gastroenterol 2014;20:18022-30. [Crossref] [PubMed]
- Tachimori Y, Ozawa S, Numasaki H, et al. Supraclavicular node metastasis from thoracic esophageal carcinoma: a surgical series from a Japanese multi-institutional nationwide registry of esophageal cancer. J Thorac Cardiovasc Surg 2014;148:1224-9. [Crossref] [PubMed]
- Murakami H, Nishikawa K, Hirao M, et al. A Case of Combined Modality Therapy for a Cervical Lymph Node Recurrence after Surgery for Esophageal Cancer. Gan To Kagaku Ryoho 2015;42:1626-8. [PubMed]
- Kosugi S, Kawaguchi Y, Kanda T, et al. Cervical lymph node dissection for clinically submucosal carcinoma of the thoracic esophagus. Ann Surg Oncol 2013;20:4016-21. [Crossref] [PubMed]
- Watanabe H, Kato H, Tachimori Y. Significance of extended systemic lymph node dissection for thoracic esophageal carcinoma in Japan. Recent Results Cancer Res 2000;155:123-33. [Crossref] [PubMed]
- Law S, Wong J. Two-field dissection is enough for esophageal cancer. Dis Esophagus 2001;14:98-103. [Crossref] [PubMed]
- Ye K, Xu JH, Sun YF, et al. Characteristics and clinical significance of lymph node metastases near the recurrent laryngeal nerve from thoracic esophageal carcinoma. Genet Mol Res 2014;13:6411-9. [Crossref] [PubMed]
- Chinese Society of Esophageal Cancer of Chinese Anta-cancer Association. Clinical practice guidelines for the diagnosis and treatment of esophageal cancer. Beijing: China Union Medical University Press, 2011:153-4.
- Tachimori Y, Ozawa S, Numasaki H, et al. Efficacy of lymph node dissection by node zones according to tumor location for esophageal squamous cell carcinoma. Esophagus 2016;13:1-7. [Crossref] [PubMed]
- Ueda Y, Shiozaki A, Itoi H, et al. Intraoperative pathological investigation of recurrent nerve nodal metastasis can guide the decision whether to perform cervical lymph node dissection in thoracic esophageal cancer. Oncol Rep 2006;16:1061-6. [PubMed]
- Lagergren J, Mattsson F, Zylstra J, et al. Extent of Lymphadenectomy and Prognosis After Esophageal Cancer Surgery. JAMA Surg 2016;151:32-9. [Crossref] [PubMed]


