
What you do not know, you do not recognize…and you do not improve future patient care…particularly in extracorporeal life support (ECLS) patients
The title of this editorial comes from a statement (“Wat je kent niet, herken je niet”) by Prof. Hein J. J. Wellens, former Head of the Cardiology Department at the Maastricht University Medical Centre, The Netherlands. With this sentence, obviously, he wanted to focus on the importance of accurate and appropriate knowledge and understanding of all aspects and mechanisms of cardiovascular illnesses in advance, had the clinician to recognize what was going wrong in due time in the examined patient. This statement may find a proper and critical place in the management of patients undergoing extracorporeal life support (ECLS). The awareness, suspicion, recognition, and confirmation of what and which kind of adverse events are possibly occurring or ongoing, is paramount in critical patients, but even more important in ECLS subjects, who are, to some extent, amongst the frailest and complex patients due to several circumstances. End-stage or acutely refractory disease state, severe functional derangement of the heart and all other organs, the further injury given by an external artificial device with inevitable foreign surface/blood contact and its related needs and maladaptive changes (anticoagulation, systemic inflammatory reaction, bleeding and thrombosis, left ventricular distension, etc.), and other relevant factors, are all peculiar aspects of ECLS. The factors may intervene in the genesis of complications in an overt way or remain hidden during the ECLS run but always remarkably impacting the ultimate patient outcome. Complications are, unfortunately, very frequent and sometimes devastating in ECLS, including illness- or iatrogenic-related (1-5). Another critical aspect regarding ECLS patients accounts also for the poorly described events characterizing the clinical course and conditions. Indeed, limited information are often provided about timing and causes of death, sometimes merging all patients’ deaths in the “in-hospital outcome” description, not providing any further and useful information whether the final event occurred during or after ECLS weaning. Indeed, complications occurring during or after ECLS are often defined by many investigators as “early outcome” events without any specific mention on time, type of, and circumstances related to the adverse event, thereby impeding any appraisal in this respect. Often, anticipated ECLS termination might be due to physicians’ or family’s decision, or both, situations which may add additional uncertainty on actual conditions and ongoing events of the supported patients.
So, do we always report, realize, understand, achieve comprehensive information, react, and timely, solve, in case, these complications? Do we always have the full spectrum of information on what led to an unfavorable clinical course? Awareness, suspicion, and recognition, are certainly three key players in such a setting, but we need knowledge and strive to enhance such understanding. For the time being, we should understand more about the ECLS/patient interaction, even in the maladaptive changes, and have the precise knowledge what are the actual cause of deaths, the confirmation of suspected events occurring ante-mortem, and discover and understand events unrecognized during the eventually unfavorable ECLS run.
The paper of Jia and associated is extremely relevant and timely according to the above-mentioned aspects (6). Indeed, the critical aspect of the discrepancy, between clinically recognized and diagnosed adverse events and the findings at autopsy, is once again highlighted (6). The authors showed that such a discrepancy was present in all 19 patients who underwent post-mortem examination, with 56% rate of major pathologies not disclosed during the ECLS run and which may have led to a possible therapeutic action and, hence, a potential impact on ultimate patient prognosis (6). Notwithstanding, the most frequent misdiagnosis accounted for cardiovascular events (mainly acute myocardial infarction) or neurological injury (mainly bleeding) (6).
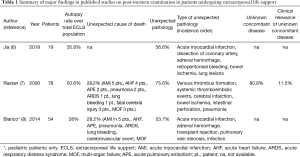
Previously, Rastan and associates have also clearly underlined the importance and extent of unrecognized pre-mortem events (75% of all autopsies), showing that an unexpected cause of death was found in almost 30% of the examined patients (78 over 154 deaths) in a postcardiotomy ECLS series (mainly cardiac and neurologic) (7). Also, in this study, the most frequent unrecognized events were cardiocirculatory (mainly thromboembolic) and neurological (7). Furthermore, they also underlined how the complication rate was, in terms of severity and incidence, directly correlated with the ECLS duration, particularly in terms of thromboembolic events, either in the venous or arterial vasculature (7). Interestingly, the same rate of unexpected cause of death, found at autopsy observed by Rastan and colleagues in adult patients, was found by Blanco and associates in 29 pediatric patients undergoing veno-arterial ECLS for several etiologies (8), with major discrepancy also noted in more than half of the examined patients (Table 1).
Full table
A finding of interest, which has been confirmed in all the three papers reporting results of post-mortem examination in ECLS patients (Table 1), is the incidence of unrecognized acute myocardial infarction in such a setting (6-8). Indeed, myocardial damage was the most common pathology among the unrecognized pathologies, indicating that, while supporting the blood and oxygen delivery to the periphery, the heart might be at danger to some extent during ECLS. This is another well-known negative factor in ECLS patients, since increase in left ventricular afterload may induce a rise in the end-diastolic pressure and generate subendocardial ischemia. Furthermore, the ejected blood from the left ventricle might be deoxygenated due to the poor gas exchange and blood flow through the lungs due to the ECLS physiology. Accordingly, further investigation, either post- or pre-mortem, are certainly necessary to elucidate actual impact of ECLS support of myocardial integrity and condition, which are, at the moment, poorly known.
The discrepancy between ante-mortem diagnosis and post-mortem findings found in ECLS occur also in subjects undergoing other form of mechanical circulatory support (MCS), like left ventricular assist device (LVAD) (9-13). This demonstrates that, most likely, the association between severe cardiocirculatory impairment and artificial devices to sustain it, may induce profound alteration and be responsible of several unrecognized complications, which should therefore always be taken into consideration if the clinical status deteriorates unexpectedly or without apparent explanation.
In all probability, autopsy is the most complete medical procedure. Although it is characterized by limited private interest, it is characterized by an enormous public health importance. Indeed, the post-mortem examination allows a physician to obtain a comprehensive understanding of a given case which may be a wealth of experience for future similar occurrences. Until the 1960s necropsy was one of the key procedures of modern medicine, the center of medical research, and the most efficient way to detect clinical discrepancies (14). In the 1960s, the hospital autopsy rate in Europe and the USA was around 60%, but by the end of the 20th century, the numbers of autopsies performed declined so that is now around 10% or less, and this notwithstanding the fact that this medical practice has the potential to be a major driver of quality improvement (15).
Despite many decades of research, it is still difficult to compare study results with the purpose of quantifying the discrepancies between clinical and autopsy diagnoses. In fact, these studies deal with different groups of patients who may not be comparable and many conditions causing death are different between the various ages, and even between surgical vs. non-surgical patients. In 1983, Goldman et al. showed in their landmark study that, despite the advances in medicine, discrepancy rates between clinical and autopsy diagnoses had been similar over a period of three decades, with about 10% providing a diagnosis that might have led to a change in patient’s treatment and/or prolonged survival (16). From that point on, additional studies have shown similar findings with discrepancy rates ranging from 8% to >30%, depending on the various clinical conditions (14,17). Interestingly, even though global diagnostic sensitivity seems to have remained the same over the years, diagnosis of some conditions has improved, while that of others worsened.
It has been shown that cardiovascular diseases were described as a risk factor for the occurrence of discrepancies, especially of class I. Autopsies performed in individuals undergoing ECLS represent a particular clinicopathological setting where, according to the very few studies on this subject, the number of discrepancies per patients found at post-mortem examination seems to be larger than that in other conditions. The study by Jia et al.—even though encumbered by significant limitations—shows that the large majority of the discrepancies found in autopsy reports were ECLS non-specific and characterized by a striking concentration in each patient (6).
Taken together, all of these considerations allow us a few thoughts:
- Autopsies—whilst on the wane because of clinician and even pathologist indifference—continues to represent an important diagnostic role in the current practice of medicine to highlight undeclared pathologies and, especially, to provide further understanding of diseases that are not yet fully recognized or of the effects of new/relatively new procedures, such as ECLS. As far as this latter case is concerned, autopsies should be highly encouraged in order to investigate large homogeneous populations and enabling statistical exploration;
- The impact of ECLS on myocardial integrity requires ad hoc and detailed investigations, since there are increasing evidences that the heart may be affected by unfavorable hemodynamic and metabolic conditions which will end up in additional injury, often unrecognized;
- New interest of pathologists on autopsy might be created by training figures specifically committed to this procedure and highly qualified to investigate post-mortem aspects;
- Post-autopsy investigations in particular conditions, such as ECLS patients, should necessarily include a histopathological analysis which, as it is known, is capable of highlighting tissue changes otherwise never detectable by the sole classical autopsia (in Latin, “a seeing with one’s own eyes”). Autopsy should also undergo a process of “modernization” by introducing a number of analyses (e.g., molecular or post-mortem imaging) which are currently performed in other pathology fields (17,18);
- Especially in circumstances following complex and invasive procedures, such as ECLS, the referring physicians who have requested a post-mortem examination should not only settle for the relevant pathology report but also actively attend the procedure by providing full information to the dissector and, at the same time, observing with their own eyes the possible tissue/organ modifications.
In conclusion, determination of the cause of death is of outmost importance in medicine, but particularly in ECLS patients, based on the demonstrated high incidence of unrecognized cause and also concurrent major complications not diagnosed ante-mortem. Autopsy, which represents still an invaluable procedure to elucidate or confirm the cause of death, may represent an undisputable asset to enhance and clarify untoward effects of ECLS in critical patients. The already well-known high rate of complications in ECLS, but the likely presence of hidden adverse events, should therefore pose the attending ECLS personnel to be continuously alert for patient evaluation, particularly with advanced imaging modalities of the brain. Difficulty in patient mobilization and transport, as well as family will, are usually limiting factors for pre or post-mortem investigations. Modernization of post-mortem investigations and diagnosing might represent additional steps to provide more information to clinicians avoiding expected denial from the patient families, and maybe reducing time and costs for hospital investigations as well as progress in the understanding of treatment failure or disclose unrecognized events, several leading to death, in complex patients and treatment modalities.
Acknowledgments
None.
Footnote
Conflicts of Interest: Prof. Dr. R Lorusso: consultant for Medtronic and LivaNova, and advisory board member of PulseCath and Eurosets. Prof. D Corradi has no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
References
- Zangrillo A, Landoni G, Biondi-Zoccai G, et al. A meta-analysis of complications and mortality of extracorporeal membrane oxygenation. Crit Care Resusc 2013;15:172-8. [PubMed]
- Cheng R, Hachamovitch R, Kittleson M, et al. Complications of extracorporeal membrane oxygenation for treatment of cardiogenic shock and cardiac arrest: a meta-analysis of 1,866 adult patients. Ann Thorac Surg 2014;97:610-6. [Crossref] [PubMed]
- Lorusso R, Barili F, Mauro MD, et al. In-Hospital Neurologic Complications in Adult Patients Undergoing Venoarterial Extracorporeal Membrane Oxygenation: Results From the Extracorporeal Life Support Organization Registry. Crit Care Med 2016;44:e964-72. [Crossref] [PubMed]
- Lorusso R, Gelsomino S, Parise O, et al. Neurologic Injury in Adults Supported With Veno-Venous Extracorporeal Membrane Oxygenation for Respiratory Failure: Findings From the Extracorporeal Life Support Organization Database. Crit Care Med 2017;45:1389-97. [Crossref] [PubMed]
- Lo Coco V, Lorusso R, Raffa GM, et al. Clinical complications during veno-arterial extracorporeal membrane oxigenation in post-cardiotomy and non post-cardiotomy shock: still the achille's heel. J Thorac Dis 2018;10:6993-7004. [Crossref] [PubMed]
- Jia D, Neo R, Lim E, et al. Autopsy and clinical discrepancies in patients undergoing extracorporeal membrane oxygenation: a case series. Cardiovasc Pathol 2019;41:24-8. [Crossref] [PubMed]
- Rastan AJ, Lachmann N, Walther T, et al. Autopsy findings in patients on postcardiotomy extracorporeal membrane oxygenation (ECMO). Int J Artif Organs 2006;29:1121-31. [Crossref] [PubMed]
- Blanco C, Steigman C, Probst N, et al. Discrepancies between autopsy and clinical findings among patients requiring extracorporeal membrane oxygenator support. ASAIO J 2014;60:207-10. [Crossref] [PubMed]
- Roosen J, Frans E, Wilmer A, et al. Comparison of premortem clinical diagnoses in critically iII patients and subsequent autopsy findings. Mayo Clin Proc 2000;75:562-7. [Crossref] [PubMed]
- Heverly DN, Prayson RA. Neuropathology associated with ventricular assist devices: an autopsy series of 33 patients. Ann Diagn Pathol 2001;5:67-73. [Crossref] [PubMed]
- Rose AG, Park SJ. Pathology in patients with ventricular assist devices: a study of 21 autopsies, 24 ventricular apical core biopsies and 24 explanted hearts. Cardiovasc Pathol 2005;14:19-23. [Crossref] [PubMed]
- Curtis JJ, Walls JT, Boley TM, et al. Autopsy findings in patients on postcardiotomy centrifugal ventricular assist. ASAIO J 1992;38:M688-90. [Crossref] [PubMed]
- Roulson J, Benbow EW, Hasleton PS. Discrepancies between clinical and autopsy diagnosis and the value of post mortem histology; a meta-analysis and review. Histopathology 2005;47:551-9. [Crossref] [PubMed]
- Hooper JE, Williamson AK. Autopsy in the 21st Century. Cham, Switzerland: Springer Nature Switzerland, 2019.
- Tavora F, Crowder CD, Sun CC, et al. Discrepancies between clinical and autopsy diagnoses: a comparison of university, community, and private autopsy practices. Am J Clin Pathol 2008;129:102-9. [Crossref] [PubMed]
- Goldman L, Sayson R, Robbins S, et al. The value of the autopsy in three medical eras. N Engl J Med 1983;308:1000-5. [Crossref] [PubMed]
- Chevallier C, Doenz F, Vaucher P, et al. Postmortem computed tomography angiography vs. conventional autopsy: advantages and inconveniences of each method. Int J Legal Med 2013;127:981-9. [Crossref] [PubMed]
- Szaluś-Jordanow O, Bonecka J, Pankowski F, et al. Postmortem imaging in goats using computed tomography with air as a negative contrast agent. PLoS One 2019;14:e0215758. [Crossref] [PubMed]


