
Local consolidative therapy in metastatic non-small cell lung cancer
The existence of an oligometastatic cancer state has been supported by theoretical considerations (1) and clinical observations (2) for several decades. Defining oligometastatic disease is challenging. A relevant (though vague) description might be “that some patients so affected should be amenable to a curative therapeutic strategy” (2). Long-term cure of selected patients with metastatic disease has been achieved in selected settings, typically using surgical approaches (3,4). Even for patients whose disease will not be cured, local therapy for limited metastatic disease can prolong survival (5). Advances in systemic therapy to eradicate microscopic disease and the availability of non-surgical techniques to eliminate visible metastatic tumors (6,7) could be expected to expand the pool of patients who will benefit from radical treatment of metastatic disease. We now have randomized trial data suggesting that the addition of local therapy to systemic treatment for oligometastatic non-small cell lung cancer (NSCLC) could improve outcomes.
Gomez et al. recently published updated results of a multi-institutional, randomized controlled phase II study that investigated the potential benefit of aggressive local consolidative therapy (LCT) compared to maintenance or observation for patients with oligometastatic NSCLC (up to 3 metastatic sites) who did not have disease progression after initial first-line systemic therapy (8). The trial was terminated after 49 subjects were randomized, due to a planned interim analysis that revealed a dramatic improvement in progression-free survival (PFS) (the primary study endpoint) for patients who received LCT. The first publication from this trial revealed that LCT prolonged PFS duration and delayed the development of new sites of disease, which was an early signal that local therapy could yield wide-ranging benefits (9). Now, with a median follow-up duration of 29 months, we see that LCT provided a significant overall survival (OS) benefit (median 41 vs. 17 months, P=0.017) (8). This is particularly impressive in light of the fact that nine out of 20 subjects on the control arm who developed disease progression crossed over to receive LCT. A separate phase II trial yielded similar findings (10) (see Table 1), and a confirmatory phase II/III trial (NRG-LU002) is ongoing. In NRG-LU002, approximately 378 subjects with stable or improving and oligometastatic disease after four cycles of first-line chemotherapy and/or immunotherapy will be randomized to receive maintenance systemic therapy with or without LCT, will be enrolled, and OS is a primary endpoint. The study is powered to detect an improvement in median OS duration of approximately 10 months.
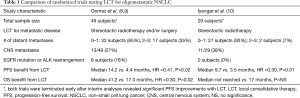
Full table
The Gomez trial has several limitations that will prevent its findings from immediately changing practice patterns. Most of these have already been acknowledged by the authors (8,9). The sample size was limited, and the trial included subjects who received both four cycles of first-line chemotherapy (n=41) and subjects who received three months of targeted therapy for EGFR mutations (n=6) or ALK rearrangements (n=2). The primary objective of prolonging PFS with aggressive local therapy could be viewed as a “low bar”, unless there was a concern that LCT could cause treatment-related toxicity or interfere with subsequent systemic therapy. Additionally, the landscape of metastatic NSCLC has changed, and many patients are now treated with first-line immunotherapy or immunotherapy plus chemotherapy, which was not the case when the Gomez study was performed (2012 to 2016).
As the evidence supporting aggressive local therapy for oligometastatic NSCLC grows, we will face new questions in clinical practice:
- Who will benefit from aggressive local therapy for metastatic NSCLC? Both the Gomez trial and NRG-LU002 include subjects with any number of metastatic lesions at the time of diagnosis who have three or fewer sites of disease after systemic therapy. Potential predictors of benefit from local therapy could include disease burden at the time of diagnosis, number of disease sites at the time of local therapy, specific organs harboring metastatic disease (11), and extent of response to systemic therapy. Future work may identify biomarkers for treatment success, such as clearance of circulating tumor DNA (12);
- What is the optimal local therapy for treating oligometastatic NSCLC? Should we choose between surgical resection, stereotactic radiotherapy, or some other form of ablation based on toxicity risks and convenience, or could specific local treatments synergize with ongoing systemic therapy (13-15)? Do all sites of metastatic disease require treatment, or can local therapy to a single site of disease (16) or a subset of involved sites yield clinical benefit?
- When is the best time to implement local therapy for oligometastatic NSCLC? Upfront use of local therapy would address the sites of disease most likely to cause disease progression during systemic therapy. Treatment at the time of best response to systemic therapy, if that can be identified, could minimize the risk of serious toxicity related to local therapy (17). Applying local therapy in cases of limited disease progression might prolong the benefits of ongoing systemic therapy.
The Gomez study and other recent efforts have set the stage for a generation of clinical trials (18), not necessarily specific to NSCLC, that aim to answer the questions above. Importantly, these studies are being performed in the era of immunotherapy, where long-term survival for a portion of patients with metastatic NSCLC is now expected (19). In parallel with trials testing comprehensive consolidative radiotherapy (17,20), many groups are testing radiotherapy to one or a few cancerous lesions as a tool to potentiate the effects of immunotherapy to treat disease in unirradiated sites (21-24). Based on early results with these two approaches, we expect that local radiotherapy will play a critical role as we aim to convert advanced NSCLC from a uniformly fatal condition into a chronic disease.
Acknowledgments
None.
Footnote
Conflicts of Interest: N Ohri: consulting fees from Merck and AstraZeneca. Dr. Halmos: Grant/Research Support: Boehringer Ingelheim, AstraZeneca, Merck, BMS, Novartis, Eli Lilly, Takeda, AbbVie, Mirati, Novartis, GSK, Guardant Health; Consultant: Boehringer Ingelheim, Astra Zeneca, Novartis, Pfizer, Genentech, Guardant Health, Spectrum, Ignyta. Turning Point Therapeutics. The other authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
References
- Withers HR, Lee SP, editors. Modeling growth kinetics and statistical distribution of oligometastases. Elsevier: Seminars in radiation oncology, 2006.
- Hellman S, Weichselbaum RR. Oligometastases. J Clin Oncol 1995;13:8-10. [Crossref] [PubMed]
- Nordlinger B, Guiguet M, Vaillant JC, et al. Surgical resection of colorectal carcinoma metastases to the liver: a prognostic scoring system to improve case selection, based on 1568 patients. Cancer 1996;77:1254-62. [Crossref] [PubMed]
- Billingsley KG, Burt ME, Jara E, et al. Pulmonary metastases from soft tissue sarcoma: analysis of patterns of disease and postmetastasis survival. Ann Surg 1999;229:602. [Crossref] [PubMed]
- Patchell RA, Tibbs PA, Walsh JW, et al. A randomized trial of surgery in the treatment of single metastases to the brain. N Engl J Med 1990;322:494-500. [Crossref] [PubMed]
- Andrews DW, Scott CB, Sperduto PW, et al. Whole brain radiation therapy with or without stereotactic radiosurgery boost for patients with one to three brain metastases: phase III results of the RTOG 9508 randomised trial. Lancet 2004;363:1665-72. [Crossref] [PubMed]
- Rusthoven KE, Kavanagh BD, Cardenes H, et al. Multi-institutional phase I/II trial of stereotactic body radiation therapy for liver metastases. J Clin Oncol 2009;27:1572-8. [Crossref] [PubMed]
- Gomez DR, Tang C, Zhang J, et al. Local consolidative therapy vs. maintenance therapy or observation for patients with oligometastatic non–small-cell lung cancer: long-term results of a multi-institutional, phase II, randomized study. J Clin Oncol 2019;37:1558-65. [Crossref] [PubMed]
- Gomez DR, Blumenschein GR Jr, Lee JJ, et al. Local consolidative therapy versus maintenance therapy or observation for patients with oligometastatic non-small-cell lung cancer without progression after first-line systemic therapy: a multicentre, randomised, controlled, phase 2 study. Lancet Oncol 2016;17:1672-82. [Crossref] [PubMed]
- Iyengar P, Wardak Z, Gerber DE, et al. Consolidative radiotherapy for limited metastatic non-small-cell lung cancer: A phase 2 randomized clinical trial. JAMA Oncol 2018;4:e173501. [Crossref] [PubMed]
- Poleszczuk JT, Luddy KA, Prokopiou S, et al. Abscopal benefits of localized radiotherapy depend on activated T-cell trafficking and distribution between metastatic lesions. Cancer Res 2016;76:1009-18. [Crossref] [PubMed]
- Merriott D, Chaudhuri A, Jin M, et al. Circulating Tumor DNA Quantitation for Early Response Assessment of Immune Checkpoint Inhibitors for Lung Cancer. Int J Radiat Oncol Biol Phys 2017;99:S20-1. [Crossref]
- Shaverdian N, Lisberg AE, Bornazyan K, et al. Previous radiotherapy and the clinical activity and toxicity of pembrolizumab in the treatment of non-small-cell lung cancer: a secondary analysis of the KEYNOTE-001 phase 1 trial. Lancet Oncol 2017;18:895-903. [Crossref] [PubMed]
- Chu KF, Dupuy DE. Thermal ablation of tumours: biological mechanisms and advances in therapy. Nat Rev Cancer 2014;14:199. [Crossref] [PubMed]
- Kabarriti R, Guha C. The Immunobiology of Tumor Ablation. Management of Urologic Cancer: Focal Therapy and Tissue Preservation. Wiley-Blackwell, 2017;7:33.
- Postow MA, Callahan MK, Barker CA, et al. Immunologic correlates of the abscopal effect in a patient with melanoma. N Engl J Med 2012;366:925-31. [Crossref] [PubMed]
- Palma DA, Olson R, Harrow S, et al. Stereotactic ablative radiotherapy versus standard of care palliative treatment in patients with oligometastatic cancers (SABR-COMET): a randomised, phase 2, open-label trial. Lancet 2019;393:2051-8. [Crossref] [PubMed]
- Al-Shafa F, Arifin AJ, Palma DA, et al. A review of ongoing trials of stereotactic ablative radiotherapy for oligometastatic cancers: where will the evidence lead? Front Oncol 2019;9:543. [Crossref] [PubMed]
- Gettinger S, Horn L, Jackman D, et al. Five-year follow-up of nivolumab in previously treated advanced non–small-cell lung cancer: results from the CA209-003 study. J Clin Oncol 2018;36:1675-84. [Crossref] [PubMed]
- Ost P, Reynders D, Decaestecker K, et al. Surveillance or metastasis-directed therapy for oligometastatic prostate cancer recurrence: a prospective, randomized, multicenter phase II trial. J Clin Oncol 2018;36:446-53. [Crossref] [PubMed]
- Theelen WS, Peulen HM, Lalezari F, et al. Effect of pembrolizumab after stereotactic body radiotherapy vs pembrolizumab alone on tumor response in patients with advanced non–small cell lung cancer: results of the PEMBRO-RT phase 2 randomized clinical trial. JAMA Oncol 2019. [Epub ahead of print]. [Crossref] [PubMed]
- Ohri N, Halmos B, Cheng H, et al. Abstract CT005: FLT3 ligand (CDX-301) and stereotactic radiotherapy for advanced non-small cell lung cancer. Chicago, IL: AACR Annual Meeting 2018.
- Twyman-Saint Victor C, Rech AJ, Maity A, et al. Radiation and dual checkpoint blockade activate non-redundant immune mechanisms in cancer. Nature 2015;520:373. [Crossref] [PubMed]
- Seung SK, Curti BD, Crittenden M, et al. Phase 1 study of stereotactic body radiotherapy and interleukin-2—tumor and immunological responses. Sci Transl Med 2012;4:137ra74. [Crossref] [PubMed]


