Feasibility and validity of double-arm specimen extraction method after partial lung resection in single-port thoracoscopic surgery
Introduction
Single-port thoracoscopic partial pulmonary resection is safe and reliable (1). However, after partial pulmonary resection, it is often necessary to use a specimen extractor to assist with lung specimen extraction from the thoracic cavity. Currently, most clinical specimen extractors are single-arm operated and are associated with several drawbacks during single-port thoracoscopic specimen removal, including: (I) the specimen is easily deformed and distorted; (II) the extractor does not hold specimens tightly; and (III) it is difficult to load large specimens because of the small size of the opening in the specimen bag.
To our knowledge, few reports have evaluated specimen extractors or how to improve lung specimen extraction method. In this study, we evaluated an improved double-arm lung specimen extraction method using two curved- and oval-tipped forceps holding a modified sterile rubber glove. The purpose of this study was to evaluate the feasibility and surgical advantages of this double-arm specimen extraction method by comparing extraction time with the double-arm vs. single-arm method.
Methods
Patients
This study was a retrospective analysis of data for 268 patients undergoing partial lung resection with single-port thoracoscopy and a specimen extractor in the Union Medical College Hospital of Fujian Medical University from November 2017 to June 2018. Patients included 108 men and 160 women with 144 patients undergoing double-arm specimen extraction and 124 patients undergoing single-arm specimen extraction. Patient’s age (mean ± standard deviation) was 57.09±11.09 years in the double-arm group and 57.61±10.98 years in the single-arm group. We further divided patients into three groups based on the specimen location as follows: upper-lobe group (group I), lower-lobe group (group II), and lung-segment group (group III). We then performed a subgroup analysis based on the degree of collapse of the lung lobe specimens, classed as good in groups IA and IIA and poor in groups IB and IIB. Exclusion criteria included: (I) cases in which using a specimen extractor was abandoned during the process of specimen extraction; (II) specimens were too large to place in the specimen bag and could only be removed after extending the incision; and (III) surgical video recording was lost or incomplete making it impossible to accurately calculate the time required for specimen removal. By reviewing patients' medical records and surgical videos, we collected patients’ general data as well as the time required for lung specimen removal. We defined the time required for pulmonary specimen removal as the time from when the specimen removal device entered the thoracic cavity to the complete removal of the lung specimen from the thoracic cavity. During the period of this study, all specimens were taken out by experienced doctors in our treatment group, who were able to use two different methods to remove specimens effectively and quickly.
We distinguish the degree of collapse of the lung according to the situation of pulmonary expansion during operation. We mainly pay attention to the following three points: (I) color: the pulmonary lobe is light red and the collapsed lobe is dark red; (II) shape: the pulmonary lobe surface is full and round, but the collapsed pulmonary lobe stool is wrinkled and uneven; (III) tension: the pulmonary lobe surface tension is large, but the collapsed pulmonary lobe surface tension is small.
Operation
All patients underwent single-port thoracoscopic surgery under general anesthesia. At the beginning of the operation, a 3.5–4.5-cm-long incision was made between the anterior axillary line and the axillary midline between the 4th or 5th intercostal space on the affected side of the chest wall, and a single-port thoracoscopic lap-protector was inserted. Segmentectomy or lobectomy was then performed based on the preoperative plan. After resection, lung specimens were completely free from the thoracic cavity.
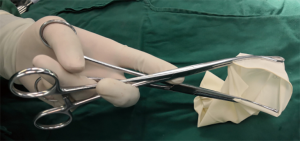
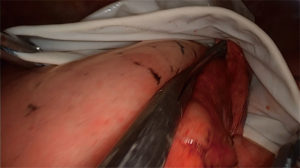
Double-arm specimen extraction method: A size 8 aseptic, powder-free, rubber glove was tied with silk suture at the palm-finger junction and a cylindrical specimen bag was created. Next, we clamped one curved, oval-tipped forceps to each side of the edge of the glove opening to make a double-arm specimen extractor. This extractor was then placed in the thoracic cavity through the single operating port. The operator held the two crossed forceps in one hand while separating the ends of the forceps, then the glove was opened to form the specimen bag (Figure 1). The operator’s other hand held the surgical instrument to place the lung specimen into the specimen bag. During specimen removal, to prevent the specimen sliding out, the operator held the specimen with the two curved, oval-tipped forceps in one hand while using the other hand to continue to place the remaining lung specimen into the glove with the surgical instrument until the lung specimen was fully packed into the glove (Figure 2). The two curved, oval-tipped forceps were brought together, which closed the glove specimen bag, and the lung specimen was then pulled out of the thoracic cavity thought the surgical incision.
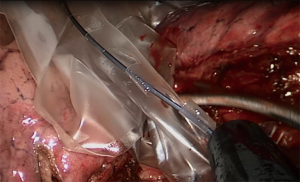
Single-arm specimen extraction method: we use different types of specimen extractor for different size specimens, so that the specimen bag is most suitable for the size of specimens. The operator placed the extractor into the thoracic cavity through the single operating port with one hand, and pushed the ring at the top of the center wire of the extractor to open the specimen bag (Figure 3) while using the other hand with the surgical instrument to hold the lung specimen. The specimen was then placed in the specimen bag. The assistant used a pair of curved, oval-tipped forceps to clamp the soft steel wire ring at the mouth of the lung specimen bag to prevent the specimen bag from being compressed, deformed, and twisted while the specimen was placed in the bag (Figure 4). Once the bag was full, the operator pulled the ring at the top of the center wire in the single-arm specimen remover to close the specimen bag, then pulled out the specimen remover through the single operating port and removed the lung specimen from the bag.
Statistical analysis
Numerical data were expressed as mean ± standard deviation and measurement data were expressed as percentage. SPSS 20.0 data analysis system (IBM Corp., Armonk, NY, USA) was used to analyze the data. We used the independent samples t-test and chi-square test to analyze the data. P<0.05 indicated statistical significance.
Results
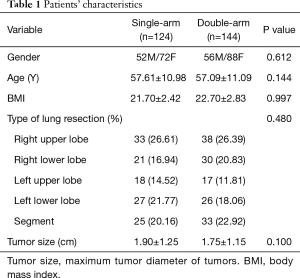
In our study, all lung specimens were successfully removed by double-arm or single-arm extraction method. No bags ruptured, we encountered no incisional infection postoperatively, and no tumor dissemination occurred at the incision during follow-up. We analyzed patients’ age, sex, body mass index (BMI), tumor location, and maximum tumor diameter. We saw no significant difference between the single-arm and double-arm groups for these measurements. The cost (YUAN) of double-arm and single-arm specimens removal devices were (2 vs. 364.5) respectively (Table 1).
Full table
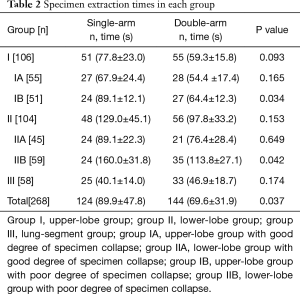
In group I, 55 patients had a good degree of specimen collapse (group IA). Among these, 28 patients had undergone double-arm extraction method, and 27 patients had undergone single-arm extraction method. Fifty-one patients had a poor degree of specimen collapse (group IB) had a poor degree of specimen collapse. Among these, 27 patients had undergone double-arm extraction method, and 24 had undergone single-arm extraction method. Forty-five patients in group II had a good degree of specimen collapse (group IIA). Among these, 21 patients had undergone double-arm extraction method, and 24 had undergone single-arm extraction method. Fifty-nine patients in group II had a poor degree of specimen collapse (group IIB). Among these, 35 patients had undergone double-arm extraction method, and 24 had undergone single-arm extraction method. Fifty-eight patients in group III had a poor degree of specimen collapse, of which 33 patients had undergone double-arm extraction method, and 25 had undergone single-arm extraction method (Table 2).
Full table
Lung specimen extraction time for double-arm vs. single-arm extraction method was (69.6±31.9 vs. 89.9±47.8 s, respectively, P=0.037). Pulmonary specimens were extracted in group I by double-arm vs. single-arm extraction method in (59.3±15.8 vs. 77.8±23.0 s, respectively, P=0.093). Pulmonary specimens were extracted in group IA by double-arm vs. single arm extraction method in (54.4±17.4 vs. 67.9±24.4 s, respectively, P=0.165) and by double-arm vs. single-arm extraction method in group IB in (64.4±12.3 vs. 89.1±12.1 s, respectively, P=0.034). Pulmonary specimens were extracted in group II by double-arm vs. single-arm extraction method in (97.8±33.2 vs. 129.0±45.1 s, respectively, P=0.153). Pulmonary specimens were extracted by double-arm vs. single-arm extraction method in group IIA in (76.4±28.4 vs. 89.1±22.3 s, respectively, P=0.649) and by double-arm vs. single-arm extraction method in group IIB in (113.8±27.1 vs. 160.0±31.8 s, respectively, P=0.042). Specimen removal time for double-arm vs. single-arm extraction method in group III was (46.9±18.7 vs. 40.1±14.0 s, respectively, P=0.174) (Table 2).
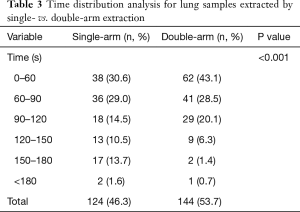
We also analyzed extraction times for lung samples over different time periods. The extraction time for most lung samples with double-arm extraction was <120 s in 91.7% of patients, compared with single-arm extraction time of <120 s in only 74.1% of patients (P<0.001), there is a statistically significant difference (Table 3).
Full table
Discussion
Single-port thoracoscopic surgery is a safe and feasible minimally invasive surgical method. The technique allows for various surgical methods, including sleeve lobectomy (1-3). After partial lung resection using single-port thoracoscopy, specimens should be removed from the thoracic cavity. Mayer et al. reported that crushing rupture and subsequent spillage of tumor tissue during endoscopic surgery may be related to the spread of malignant tumors and disease progression (4). Repeated manipulation during lung specimen extraction with single-port thoracoscopic surgery may increase the risk of tumor dissemination, so appropriate lung specimen extraction methods should be adopted to reduce lung specimen extraction time. Small wedge resection or segmentectomy lung specimens may be extracted directly if the specimens are not obviously squeezed when they are extracted through a single port. For lobectomy and larger segmentectomy lung specimens, compression by the incision is obvious when these larger specimens are extracted directly through the incision; therefore, a specimen extractor is recommended.
Currently, the most commonly used specimen extractor in abdominal surgery is a single-arm extractor. Takase et al., Sagae et al. and Clark et al. reported using single-arm specimen extractors to remove specimens via the vagina after laparoscopic splenectomy, laparoscopic partial hepatectomy, and laparoscopic hysterectomy respectively (5-7). Binsaleh et al. reported using a single-arm specimen extractor after laparoscopic radical nephrectomy to remove specimens through an abdominal incision (8). The purpose of these studies was to report different methods of specimen extraction and introduce the use of specimen extractors. However, to our knowledge, no relevant studies have discussed improved specimen-removal devices especially for lung specimen extraction methods in single-port thoracoscopic surgery.
In our center, the single-port thoracoscopic approach is routinely used in patients undergoing lung surgery. The incision size for the single-port thoracoscopic approach is 3.5–4.5 cm (1). A single-arm specimen extractor can be used to extract lung specimens in single-port thoracoscopic surgery; however, the method is inconvenient. First, the top of the specimen bag is a soft metal ring, which is easily deformed and distorted during the loading process, and which leads to repeated specimen loading. Second, for lobe specimens with poor collapse, because of the smooth and curved surface of the specimen, the single-arm specimen extractor cannot hold the specimen in the specimen bag during the loading process; therefore, specimens slide easily out of the specimen bag repeatedly during loading. Third, the size of the specimen bag is limited, and large specimens are difficult to load. Fourth, during single-port thoracoscopy, if the specimen is not satisfactorily placed in the specimen bag, an assistant is often required to use another instrument to clamp the specimen bag closed through the same single-port laparoscopic incision, which causes inter-operator interference.
Considering the shortcomings of single-arm specimen extraction method in single-port thoracoscopic surgery, we use a double-arm specimen extraction method. We use a double-arm specimen extractor consisting of two curved, oval-tipped forceps holding a modified glove, and long oval-tipped forceps for specimen extraction. The advantages of this method are as follows: First, the two poles of the double arm specimen extraction method cross and prop up the two corners of the specimen bag, which is similar to the chopstick’s propping effect. The specimen bag is not easy to slide and the size and shape of the specimen bag are relatively fixed. Second, the two oval-tipped forceps can be used to hold the specimen during specimen loading to prevent the specimen from sliding out, which reduces time associated with repeated bagging. Third, the glove mouth is large area, and the glove stretches, so it is more suitable for loading large specimens. Fourth, the operation of the double-arm specimen extraction method is performed by the operator alone, and there is no interference between the operator and the assistant.
In this study, the double-arm method was statistically significantly faster than the single-arm method. Furthermore, comparing patient groups based on the type of lung specimens (upper lobe, lower lobe, and lung segment), we found no significant statistical difference for specimen extraction time using the double-arm vs. single-arm method in each group. In our subgroup analysis based on degree of specimen collapse, we found no significant difference in extraction time between the two methods in group IA (upper lobe, good degree of collapse). In group IB (upper lobe, poor degree of collapse), the extraction time for double-arm extraction was statistically significantly shorter compared with single-arm extraction. There was no significant difference in extraction time between the two methods in group IIA (lower lobe, good degree of collapse). In group IIB (lower lobe, poor degree of collapse), extraction time by double-arm extraction was also statistically significantly shorter compared with single-arm extraction.
During the study period, the number of patients with tumors in the right middle lobe was small; therefore, we did not analyze data for these patients. Additionally, the degree of collapse in lung segment-resection specimens was poor. In segmentectomy, in order to identify the discontinuous plane and completely resect the target lung segment, we used the pulmonary expansion-collapse method (9) to make the target lung segment expand and the rest of the lung tissue collapse. The resected lung segments were all in a expended state, so there was no grouping on the degree of collapse in group III.
We found no significant difference between the two methods for lung specimen extraction time for segmentectomy or for lobectomy, with good degree of specimen collapse. The possible reasons are as follows: the size of lung specimens was small, and the weight was relatively light; pressure on the specimen bag was minimal during loading; and the specimen bag did not easily deform. Lung segment specimens can also be smoothly packed into the specimen bag even if the single-arm specimen extractor cannot hold specimens intraoperatively. Lung lobe specimens with good degree of collapse were relatively small in size in our study, and their surfaces were not curved, so they did not slide easily. Even if the single-arm specimen extractor could not hold the specimen intraoperatively, the specimen did not easily slide out of the specimen bag repeatedly during loading.
Considering the cost of surgery (YUAN), the double-arm specimens extractor is also significantly better than the single-arm specimens extractor (2 vs. 364.5). The two-arm specimens’ extractor only consumes a pair of sterile gloves, and the other instruments are conventional surgical instruments. The double-arm specimens remover we use reduces the financial burden of patients and saves medical resources.
The following limitations are present in this study: First, this was a retrospective study, and data did not include measurements of lung specimen volume. Additionally, lung specimen size was limited by the type of lung specimen. Second, we included only cases with well-preserved video, which may have introduced selection bias. Third, because of the small number of patients with right middle lobe tumors during the study period, relevant grouping research and analysis were not performed for this group of patients.
Conclusions
In single-port thoracoscopic partial lung resection, double-arm specimen extraction method is more convenient and can shorten sample extraction time, especially for upper and lower lung lobes with poor degree of collapse. Double-arm specimen extraction method is feasible and effective after single-port thoracoscopic partial lung resection.
Acknowledgments
We thank Cai Rui, from Liwen Bianji, Edanz Droup China (www.liwenbianji.cn/ac) for editing the English text of a draft of this manuscript.
Funding: The study was supported by Fujian Provincial Key Project (2014Y0024), Fujian Provincial Joint Research Project of Health Care and Education (WKJ2016-2-09), Joint Funds for the innovation of science and Technology, Fujian province (Grant number 2018Y9058).
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was approved by ethics committee of Fujian Medical University Fujian Union Hospital (No. 2018020) and written informed consent was obtained from all patients.
References
- Zhu Y, Liang M, Wu W, et al. Preliminary results of single-port versus triple-port complete thoracoscopic lobectomy for non-small cell lung cancer. Ann Transl Med 2015;3:92. [PubMed]
- Gonzalez-Rivas D, Delgado M, Fieira E, et al. Double sleeve uniportal video-assisted thoracoscopic lobectomy for non-small cell lung cancer. Ann Cardiothorac Surg 2014;3:E2. [PubMed]
- Wang G, Wang Z, Sun X, et al. Uniportal video-assisted thoracoscopic anatomic segmentectomy for small-sized lung cancer. J Vis Surg 2016;2:154. [Crossref] [PubMed]
- Mayer C, Miller DM, Ehlen TG. Peritoneal implantation of squamous cell carcinoma following rupture of a dermoid cyst during laparoscopic removal. Gynecol Oncol 2002;84:180-3. [Crossref] [PubMed]
- Takase Y, Tomizawa N, Enokida Y, et al. A case of splenic metastasis of ovarian cancer treated with complete laparoscopic splenectomy and transvaginal specimen extraction. Surg Case Rep 2016;2:26. [Crossref] [PubMed]
- Sagae UE, Orso IR, Matsumoto HM, et al. Scarless hepatectomy: natural orifice specimen extraction after left lateral sectionectomy. Arq Bras Cir Dig 2014;27:291-3. [Crossref] [PubMed]
- Clark LE, Menderes G, Tower AM, et al. A Simple Approach to Specimen Retrieval via Posterior Colpotomy Incision. JSLS 2015. [Crossref] [PubMed]
- Binsaleh S, Alomar M, Madbouly K. Pfannenstiel incision for intact specimen extraction in laparoscopic transperitoneal radical nephrectomy: a longitudinal prospective outcome study. Clinics (Sao Paulo) 2015;70:475-80. [Crossref] [PubMed]
- Chen L, Wu W. Zhongguo Fei Ai Za Zhi 2016;19:377-81. [The Main Technical Points of Thoracoscopic Anatomical Lung Segment Resection]. [PubMed]