Developing antitussives the clinician’s pipeline—what do we need?
Cough hypersensitivity as a target in drug development
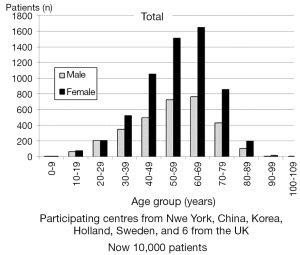
There is an urgent need to develop antitussive medications which are effective and safe. The size of the problem is hard to minimise with an estimated incidence of approximately one in ten of the population suffering from a chronic cough and about half of these subjects reporting that the cough interferes with activities of daily living (1). Recently an international survey was undertaken of 10,000 patients presenting to cough clinics throughout the world (2). As can be seen in Figure 1 chronic cough comes on in the middle age and twice as many women as men cough. The smaller numbers of the younger people are probably due to the fact that other diagnostic labels such as asthma are used. In older people it may be a problem with access (3). In each clinic the profile was very similar except in China where the population was younger.
The fact that patients present throughout the world with a similar demographic profile infers that there may be a single disease causing chronic cough. This has been termed the cough hypersensitivity syndrome (4). Patients with chronic cough often have a very similar clinical history. The question is what is the cause of this condition since this may provide us with the clues as to the best management strategy?
The unifying concept is that airway inflammation leads to a state which gives rise to chronic cough. The cause of this inflammation may be many and varied. Both internal and external factors may be responsible for the stimulus to inflammation. Infections with both viruses and bacteria may be the original cause and secondary factors may then continue the inflammatory process. An emerging cause is that of non-acid gastro-oesophageal reflux. This is because the clinical history that patients give suggests that this is a common aetiological mechanism (4,5). However whatever the ultimate cause, the concept is that there is a precipitant of chronic cough associated inflammation. This then causes a pathological process leading to the production of cough. This simple paradigm then provides a straightforward explanation for what is sometimes regarded as a mysterious symptom (6).
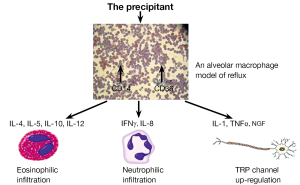
To illustrate this model we have shown the effect of reflux on an alveolar macrophage cell line. Red stained cells which have ingested the lipid content of the reflux lead to changes in the cellular expression of markers. The external presentation of these markers then causes the production of a variety of cytokines leading to an inflammatory cascade. What form the inflammatory cascade takes depends on the individual’s genetic predisposition. Thus, in patients who are prone to allergic disease there is a production of cytokines of the Th2 family. This gives rise to airway inflammation of the asthmatic type which can be variously categorised as cough variant asthma, eosinophilic bronchitis, atopic asthma or even just severe asthma.
When the person produces a neutrophilic inflammation in response to the precipitant then a different set of cytokines are responsible. Finally in almost all patients who develop a chronic cough there is upregulation of afferent nerves probably mediated by cytokines of the nerve growth factor (NGF) family. An illustration of this paradigm of airway inflammation leading to chronic cough is given in Figure 2.
New drugs working on airway inflammation
If it is accepted that a number of patients, perhaps the majority, have non-acid reflux then a simple way of inhibiting cough would be to reduce the reflux. Currently drugs such as metoclopramide, baclofen, and azithromycin are used in the clinic. Derivatives of these agents will shortly become available. These include lesogaberan (7), novel motility agents, and non-antibiotic macrolides.
A characteristic feature of patients with chronic cough, as opposed to classic asthma, is that there appears to be little or no bronchoconstriction. This is probably because of the different distribution of inflammation to that seen in asthma. This was shown by Brightling et al. in a classic paper demonstrating the distribution of mast cells surrounding bronchial smooth muscle in classical asthma whereas in the cough variant asthma mast cells are located near afferent nerves (8).
There are a number of new anti-inflammatory agents currently in development and clinical trials looking at the effects of cytokine antagonists of eosinophilic inflammation are in progress. These drugs have mainly been developed for asthma. My own experience with omalizumab is that it is a very potent agent against eosinophilic cough. The effects of the more modern agents such as mepolizumab (9) are awaited however their high price is probably going to be a barrier to widespread use.
In patients having a neutrophilic response there are no existing agents available specifically for this form of inflammation. Since this is the commonest type of inflammation present in chronic cough the poor record of current treatments is explained. Recent work has demonstrated that some bronchodilator agents particularly the modern generation of long acting anti-muscarinic agents may have a valuable role in reducing cough in the neutrophilic bronchitis (10).
Targeting the neuronal hypersensitivity
Blocking the cytokines which lead to the described proliferation of airway sensory nerves may be an attractive future strategy. Antagonists of NGF have been used successfully in clinical trials of pain due to osteoarthritis (11) but have yet to be tried in chronic cough. Rather than the simple proliferation of the nerves perhaps the most important and universal feature of chronic cough is the hypersensitivity of airway nerves.
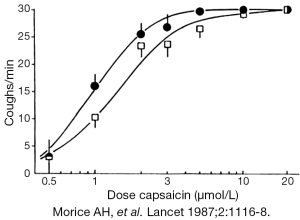
The production of airway hypersensitivity by ACE inhibitors is illustrated in Figure 3 (12). This is not airway hyperresponsiveness with increase in muscle spasm but rather an increase in the sensitivity of the airway nerves. Here the precipitant is the antihypertensive ACE inhibitor captopril which causes a shift to the left in the dose response curve to inhaled capsaicin.
One of the most interesting unresolved questions in chronic cough is where in the does this hypersensitivity reside? One suggestion is that it could be at the nerve terminals in the form of an up-regulation of nociceptors. Alternatively a more central location would be responsible for the hypersensitivity.
The mechanism of whereby sensory nerves detect changes in the external environment is through specific receptors often of the TRP channel family. The TRP channels of interest in cough are mainly temperature receptors which responded to a variety of different agonists (13). The first to be described as a “cough receptor” was TRPV1, which responds to the pungent extract of peppers capsaicin. As was demonstrated in Figure 3, it is a potent tussive agent in man and naturally inhibition of this receptor was seen as a primary target for drug development. Unfortunately the TRPV1 antagonist SB-705498 (GSK) whilst highly effective at blocking evoked cough with capsaicin challenge proved to have no effect on cough counts in patients with chronic cough (14). Unfortunately as with many TRPV1 antagonists there was also the negative side effect of a change in core body temperature. Other TRPV1 antagonists continue in clinical development, however this negative result in a well performed study has caused drug development by some companies to be abandoned. Clinical trials with TRPA1 antagonists are ongoing and results are awaited with great interest. The fact that agents such as GRC 17536 are capable of inhibiting induced cough in animal models does not predict efficacy in the clinic. Similar efficacy was seen with the neurokinin antagonists and here again drug development has been abandoned because of the lack of efficacy in the clinic.
Other members of the TRP family such as TRPM8 or the cold menthol receptor appears to have its action by inhibiting cough rather than to provoke. In studies it has been demonstrated that it is mainly afferents within the nose which are responsible for the antitussive activity of menthol (15). Thus nasal application of menthol and its derivatives or even the use of herbal remedies may be a novel route for the development of potent antitussives.
An alternative site of action of the antitussives on the airway hypersensitivity is through more central pathways, blocking neuronal traffic either by effects on the axon or on the nerve terminals. Recently we have completed a large randomised controlled clinical trial, the first of its type in chronic cough, using the drug theobromine. Theobromine has been demonstrated to act through inhibition of neurotransmission sensory fibres (16). Preliminary results suggest a modest suppression of cough in patients attending the cough clinic.
A further agent that has activity on the peripheral nerves is thalidomide. Thalidomide has now been shown to suppress cough in patients with idiopathic pulmonary fibrosis in two studies (17). The primary outcome was to subjectively assess cough which was, in some patients, dramatically reduced. The side effect profile was the main obstacle to continue the treatment.
Finally and perhaps of most interest almost complete abolition of excessive coughing was demonstrated in a pilot study. A late breaking abstract by Abdulqawi et al. at the recent ERS meeting in Barcelona showed that the antagonist of the P2X3 receptor AF 219 had a dramatic effect on objective cough counts in patients with chronic cough (18). The receptor is located on afferent sensory neurones and is normally stimulated by adenosine triphosphate (ATP), possibly released by inflammation. The study was done over two weeks in patients with long-standing chronic cough and the most dramatic reduction in cough was seen. These findings suggest that modulation of this ATP channels may be a major mechanism of hypersensitivity in man.
Acknowledgements
Disclosure: The author declares no conflict of interest.
References
- Ford AC, Forman D, Moayyedi P, et al. Cough in the community: a cross sectional survey and the relationship to gastrointestinal symptoms. Thorax 2006;61:975-9. [PubMed]
- Morice AH, Jakes AD, Faruqi S, et al. A worldwide survey of chronic cough: a manifestation of enhanced somatosensory response. Eur Respir J 2014. [Epub ahead of print]. [PubMed]
- Everett CF, Kastelik JA, Thompson RH, et al. Chronic persistent cough in the community: a questionnaire survey. Cough 2007;3:5. [PubMed]
- Morice AH, Faruqi S, Wright CE, et al. Cough hypersensitivity syndrome: a distinct clinical entity. Lung 2011;189:73-9. [PubMed]
- Everett CF, Morice AH. Clinical history in gastroesophageal cough. Respir Med 2007;101:345-8. [PubMed]
- Chung KF, Pavord ID. Prevalence, pathogenesis, and causes of chronic cough. Lancet 2008;371:1364-74. [PubMed]
- Shaheen NJ, Denison H, Björck K, et al. Efficacy and safety of lesogaberan in gastro-oesophageal reflux disease: a randomised controlled trial. Gut 2013;62:1248-55. [PubMed]
- Brightling CE, Bradding P, Symon FA, et al. Mast-cell infiltration of airway smooth muscle in asthma. N Engl J Med 2002;346:1699-705. [PubMed]
- Haldar P, Brightling CE, Hargadon B, et al. Mepolizumab and exacerbations of refractory eosinophilic asthma. N Engl J Med 2009;360:973-84. [PubMed]
- Beier J, Kirsten AM, Mróz R, et al. Efficacy and safety of aclidinium bromide compared with placebo and tiotropium in patients with moderate-to-severe chronic obstructive pulmonary disease: results from a 6-week, randomized, controlled Phase IIIb study. COPD 2013;10:511-22. [PubMed]
- Lane NE, Schnitzer TJ, Birbara CA, et al. Tanezumab for the treatment of pain from osteoarthritis of the knee. N Engl J Med 2010;363:1521-31. [PubMed]
- Morice AH, Lowry R, Brown MJ, et al. Angiotensin-converting enzyme and the cough reflex. Lancet 1987;2:1116-8. [PubMed]
- Bandell M, Macpherson LJ, Patapoutian A. From chills to chilis: mechanisms for thermosensation and chemesthesis via thermoTRPs. Curr Opin Neurobiol 2007;17:490-7. [PubMed]
- Dicpinigaitis PV, Fontana GA, Lee LY, et al. Summary of papers presented at the 2012 seventh international cough symposium. Cough 2013;9:13. [PubMed]
- Buday T, Brozmanova M, Biringerova Z, et al. Modulation of cough response by sensory inputs from the nose - role of trigeminal TRPA1 versus TRPM8 channels. Cough 2012;8:11. [PubMed]
- Usmani OS, Belvisi MG, Patel HJ, et al. Theobromine inhibits sensory nerve activation and cough. FASEB J 2005;19:231-3. [PubMed]
- Horton MR, Santopietro V, Mathew L, et al. Thalidomide for the treatment of cough in idiopathic pulmonary fibrosis: a randomized trial. Ann Intern Med 2012;157:398-406. [PubMed]
- Abdulqawi R, Dockry R, Holt K, et al. Inhibition of ATP-gated P2X3 channels by AF-219: An effective anti-tussive mechanism in chronic cough. Eur Respir J 2013;42:1965.


