Unexpectedly long intravenous and intracardiac extension of a small-sized pulmonary pleomorphic carcinoma
Introduction
Secondary cardiac malignancies, especially symptomatic ones, are uncommon, serious conditions. The routes by which neoplasms spread to the heart include direct invasion, hematogenous metastasis, lymphatic metastasis and transvenous extension. As for transvenous extension, renal cell carcinoma and hepatocellular carcinoma sometimes extend into the inferior vena cava and grow into the right atrium (1,2), but intracardiac extension of lung cancers via the pulmonary vein is rare, particularly when the lung tumor is small-sized and distant from the heart.
According to the 2004 World Health Organization (WHO) classification of the lung tumors (3), sarcomatoid carcinoma group of the lung are classified into five types: pleomorphic carcinoma, spindle cell carcinoma, giant cell carcinoma, carcinosarcoma and pulmonary blastoma. These neoplasms are uncommon histological types of lung carcinomas, comprising 0.3-1.3% of all pulmonary malignancies (3). Pleomorphic carcinoma is defined as squamous cell carcinoma, adenocarcinoma or large cell carcinoma containing spindle cells and/or giant cells, or carcinoma consisting only of spindle and giant cells. On the other hand, non-small cell carcinoma consisting only of spindle cells is called spindle cell carcinoma, and non-small cell carcinoma composed only of giant cells is named giant cell carcinoma. The behavior of tumors of this group is reported to be more aggressive than conventional non-small cell lung carcinomas (4-6).
Here we report a case of a pulmonary pleomorphic carcinoma of small size which showed unexpectedly long intravenous extension to the left atrium, resulting in fatal obstruction of the mitral valve.
Case report
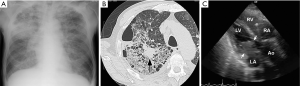
A 64-year-old male was admitted to the hospital because of dyspnea at rest and fever. He reported a history of 10-kg weight loss for six months, cough for two weeks, and fatigue, dysphagia and muscle weakness for one week. He smoked three packs of cigarettes per day for over 40 years. On admission, the height was 167 cm and the weight 55 kg, the blood pressure 97/70 mmHg, the pulse 115 beats per minute, the temperature 37.1 degree C and SpO2 92%. Chest radiograph showed pulmonary congestion and opacity in the right upper lung (Figure 1A). Chest CT scan revealed opacity in the right upper lung with a tumor of approximately two cm in diameter in it (Figure 1B). Electrocardiogram showed no specific abnormality. Treatment with antibiotics and oxygen were started but his condition and respiration was progressively worsened next four days. Echocardiogram on third hospital day showed a large mass in the left atrium that caused obstruction of the mitral inflow of left ventricle (Figure 1C). Surgical removal of the mass was not selected because of his condition. He died of cardiac inflow obstruction four days after the admission. An autopsy was performed.
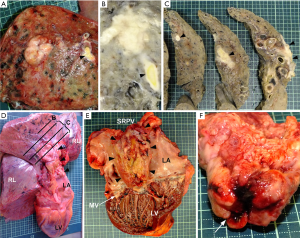
Grossly, a white, well-circumscribed nodule of 22 mm in diameter was found in the peripheral region of the upper lobe of the right lung (Figure 2A). The tumor showed direct invasion to the pulmonary vein branch (Figure 2B), and the tumor tissue extended intravenously and continuously from the lung nodule to the left atrium through the superior right pulmonary vein (Figure 2C,D). The distance between the lung nodule and the left atrium was approximately ten cm, and therefore the tumor tissue was elongated for this distance intravenously. In the lumen of the left atrium, the tumor tissue formed a mass of 8 cm × 5 cm × 3 cm (Figure 2E). The surface of the mass facing the mitral valve was indented as a mold of the shape of the mitral cusps (Figure 2F), suggesting that the mass obstructed the mitral valve. The morphology of the mitral valve itself was almost normal. Neither distant metastasis nor nodal involvement was observed. Systemic embolism of the tumor fragments was not found.
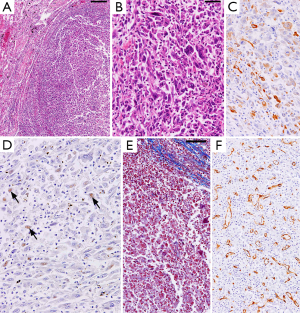
Histologically, the lung nodule as well as the intravenous and intraatrial portion of the tumor was composed of atypical spindle cells and giant cells (Figure 3A,B). Neutrophil infiltration was observed. Component of conventional non-small cell lung carcinoma (squamous cell, adeno-, or large cell carcinoma) was not found. Immunohistochemically, the spindle and giant cells were positive for cytokeratin AE1/AE3 (Figure 3C) and cytokeratin 7, and a small number of these cells were positive for TTF-1 (Figure 3D). These cells were negative for cytokeratin 20. Mallory-azan stain (which stains fibrous tissue blue) (Figure 3E) and CD34 immunostain (an endothelial marker) (Figure 3F) revealed that the tumor tissue had scant fibrous stroma and abundant small blood vessels, respectively. These findings indicate that the tumor was pleomorphic carcinoma of the lung with marked intravenous extension to the left atrium, resulting in fatal obstruction of the mitral valve. The non-neoplastic lung tissue around the nodule of the right upper lobe showed congestion and edema with marked intra-alveolar fibrin and organization. Mild emphysema was also found.
Discussion
In the present case, one of the clinical problems was the relation between the intracardiac mass and lung nodule detected by echocardiography and chest CT, respectively. Several hypotheses were considered: these tumors might be independent primaries; the former might be metastasis of the latter, and vice versa; both of them might be metastasis of an unknown primary neoplasm. At autopsy, the continuity of these two tumors via the pulmonary vein, and immunoreactivity to TTF-1 (a specific marker for primary lung carcinoma) and cytokeratin clearly indicated that the lung nodule was the primary site and the intracardiac mass was the leading edge of endovascular extension of the carcinoma.
Pleomorphic carcinoma is a rare histological type of lung carcinoma. Patients of pleomorphic carcinoma are reported to be predominantly male smokers with a mean age of 66 years (4-7). It tends to arise as a peripheral mass with a predilection for the upper lobes (5,7). The clinical course of this tumor is reported to be aggressive, compared to conventional non-small cell lung carcinomas (4-6). Histologically, pleomorphic carcinoma can be divided into two subgroups: (I) a conventional non-small cell carcinoma admixed with malignant spindle cells and/or giant cells; and (II) a carcinoma composed only of malignant spindle and giant cells. The present case corresponds to the subgroup (II), and the patient’s age, smoking habit and location of the lung tumor are thought to be typical of pleomorphic carcinoma.
Intravenous extension to the left atrium is a rare complication of lung carcinomas, and several cases including small cell carcinoma (8,9) and conventional non-small cell carcinomas (10-14) were reported previously. Among them, intracardiac extension of sarcomatoid carcinoma group is extremely rare, and only one case of giant cell carcinoma (10) and one case of pleomorphic carcinoma composed of adenocarcinoma and spindle-cell components [subgroup (I), see above] (15) were described (Table 1). Thus, our paper is the second report of pulmonary pleomorphic carcinoma extending intravenously to the left atrium.

Full table
As shown in Table 1, common symptoms of these patients include weight loss and cough, which probably resulted from the lung tumor itself. Dyspnea, palpitations and arrhythmia might represent signs caused by an intracardiac tumor. The present case showed these common symptoms including dyspnea while muscle weakness, the pathophysiology of which was not clear, was a peculiar symptom to this case.
In the previously reported cases of sarcomatoid carcinomas (Table 1) and other histological types (8-14), the primary tumors in the lungs were advanced, large masses and therefore invaded near the heart. However, one of the remarkable findings of the present case is disproportionately long intravenous extension compared to the small size of the lung tumor. In fact, the lung tumor of the present case is much smaller than the previous cases (Table 1), and the intravenous component of the present tumor running from the lung nodule to the left atrium is markedly long (approximately 10 cm in length). This made clinical diagnosis difficult because the lung tumor was so distant from the heart that the intracardiac extension of the lung tumor seemed very unlikely. The histological features of the present tumor might explain this unexpectedly long extension in the pulmonary vein. First, the histological type of the lung cancer is pleomorphic carcinoma, which is biologically more aggressive than ordinary non-small cell carcinomas. Secondly, the tumor tissue had abundant blood vessels and lacked desmoplasia, which might facilitate smooth elongation in the venous lumen without necrotic collapse of the tumor tissue or hard adhesion to the surrounding structure. Hypervascularity and scant fibroplasia are shared features of other cancers with high propensity for intravenous extension, for example, hepatocellular carcinoma and renal cell carcinoma.
In summary, the present case teaches us that when a patient with a lung carcinoma even of a small size and located distantly from the heart presents with dyspnea, we should consider the possibility of intracardiac extension of the pulmonary neoplasm.
Acknowledgements
Disclosure: The authors declare no conflict of interest.
References
- Amano J, Nakayama J, Yoshimura Y, et al. Clinical classification of cardiovascular tumors and tumor-like lesions, and its incidences. Gen Thorac Cardiovasc Surg 2013;61:435-47. [PubMed]
- Goldberg AD, Blankstein R, Padera RF. Tumors metastatic to the heart. Circulation 2013;128:1790-4. [PubMed]
- Travis WD, Brambilla E, Mueller-Hermelink HK, et al. eds. World Health Organization Classification of tumours, pathology and genetics of tumours of the lung, pleura, thymus and heart. Lyon, France: IARC Press, 2004.
- Rossi G, Cavazza A, Sturm N, et al. Pulmonary carcinomas with pleomorphic, sarcomatoid, or sarcomatous elements: a clinicopathologic and immunohistochemical study of 75 cases. Am J Surg Pathol 2003;27:311-24. [PubMed]
- Yuki T, Sakuma T, Ohbayashi C, et al. Pleomorphic carcinoma of the lung: a surgical outcome. J Thorac Cardiovasc Surg 2007;134:399-404. [PubMed]
- Mochizuki T, Ishii G, Nagai K, et al. Pleomorphic carcinoma of the lung: clinicopathologic characteristics of 70 cases. Am J Surg Pathol 2008;32:1727-35. [PubMed]
- Ito K, Oizumi S, Fukumoto S, et al. Clinical characteristics of pleomorphic carcinoma of the lung. Lung Cancer. 2010;68:204-10. [PubMed]
- Brandt RR, Rubin J, Reeder GS, et al. Intracardiac extension of a lung tumor causing left ventricular inflow obstruction. J Am Soc Echocardiogr 1995;8:930-3. [PubMed]
- Lin MT, Ku SC, Wu MZ, et al. Intracardiac extension of lung cancer via the pulmonary vein. Thorax 2008;63:1122. [PubMed]
- Kodama K, Doi O, Tatsuta M. Unusual extension of lung cancer into the left atrium via the pulmonary vein. Int Surg 1990;75:22-6. [PubMed]
- Mehan VK, Deshpande J, Dalvi BV, et al. Direct extension of bronchogenic carcinoma through pulmonary veins into the left atrium mimicking left atrial myxoma. Chest 1992;101:1722-3. [PubMed]
- Watanabe N, Kubo K. Images in cardiology: Intra-left atrial invasive mass extended via the pulmonary vein. Heart 2001;85:271. [PubMed]
- Khan N, Golzar J, Smith NL, et al. Intracardiac extension of a large cell undifferentiated carcinoma of lung. Heart 2005;91:512. [PubMed]
- Costache VS, Lantuejoul S, Stoica S, et al. Giant intracardiac neoplasic thrombus of a large cell neuroendocrine carcinoma of the lung. Cardiovasc Pathol 2010;19:e85-7. [PubMed]
- Ng SW, Lim CH, Wang CW, et al. Primary pulmonary sarcomatoid carcinoma with intracardiac extension. Jpn J Thorac Cardiovasc Surg 2006;54:416-9. [PubMed]


