Nonintubated anesthesia for thoracic surgery
In recent years, with the techniques and managements of thoracic surgery increasingly improved, better lung separation and hypoxemia treatment as well as widely-used lung protective strategy have obtained proud achievement (1-3). On the other hand, to fit in with the needs of the fast track and enhanced recovery after surgery, nonintubated anesthesia for thoracic surgery has been intensively researched, reported and advocated (4-8).
Background
There are a lot of studies showing that nonintubated anesthesia for thoracic surgery is superior to the conventional general anesthesia in patients’ outcomes. Nevertheless, some patients who are supposed to under nonintubated anesthesia still need intubated during the thoracic surgery (9). In 2004, Pompeo and his coworkers evaluated the feasibility of awake thoracoscopic resection of solitary pulmonary nodules in 30 patients under sole thoracic epidural anesthesia. Comparing to patients with intubated general anesthesia, their results showed that awake technique was safely feasible with better patient satisfaction, less nursing care and shorter in-hospital stay. However, it is important to note that two of the patients in the awake group were converted to intubated general anesthesia because of lung cancer requiring lobectomy via thoracotomy approach (10-12). Therefore, anesthesiologists should emphasize and balance the indication, contradiction, advantages, disadvantages, risks and benefits of nonintubated anesthesia for thoracic surgery, in order to choose better way to perform the anesthesia safely.
Indication
According to recent evidence and experience, several thoracic surgery procedures have been proved suitable for nonintubated anesthesia, such as pleural/pericardial effusion, empyema thoracis, bullous emphysema, non-resectional lung volume reduction surgery, spontaneous pneumothorax, biopsy of interstitial lung disease, wedge resection of lung nodules, segmentectomy and lobectomy for lung cancer, mediastinal biopsy and tumor excision (6,13-22).
The patients under nonintubated anesthesia should have well-evaluation and well-preparation without contraindications and should not reject to receive it. It is worth noting that Wu and colleagues had evaluated the feasibility of geriatric patients (age ranging from 65 to 87) undergoing lobectomy, which showed comparable safety profile with control group. This study opened up the possibility of nonintubated video-assisted thoracoscopic surgery (VATS) on the old age group (23).
Contraindication
The general patients exclusion criteria includes American Society of Anesthesiologists (ASA) physical status 4 and higher, bleeding disorders, sleep apnea, unfavorable airway or spinal anatomy, strict contralateral lung isolation, clinically significant sputum production, bronchiectasis, asthma, extreme of body mass index (BMI), preoperative decompensated heart disease, severe pleural adhesion over targeted hemithorax, and noncompliance to the procedure or patient refusal (6,24).
The implement of anesthesia
Nonintubated anesthesia for thoracic surgery refers to the operation performed under regional anesthetic techniques in spontaneously breathing patients, with or without conscious sedation. Conscious sedation is safe and effective for patients using sedative or dissociative agents such as propofol, midazolam, with or without analgesics such as fentanyl to keep patient tolerate unpleasant procedures while maintaining cardiorespiratory function. That is an induced depressed level of consciousness in which a patient retains the ability to independently and continuously maintain an open airway and a regular breathing pattern, and to respond appropriately and rationally to physical stimulation and verbal commands.
Psychological preparation
Preoperative communication for reassuring the patients, intraoperative coaching, mental support, verbal communication with medical personnel, and comfortable environment with low-volume music might all contribute to calm the patients down with acceptable respiration (25,26).
Monitoring
Standard monitoring with pulse oximeter, electrocardiogram, sphygmomanometer, and end-tidal CO2 should always be in place. In addition, invasive arterial pressure monitor is often set for its versatility on monitoring arterial blood gas, real-time hemodynamic index, and fluid status inclination. For the occasion in which sedation is part of the planning, bispectral index (BIS) is highly recommended for evaluation of sedation level and advanced judgment of the anesthesia/sedation depth.
Anesthesia techniques
The anesthetic techniques consist of local anesthesia, intercostal nerve blocks, paravertebral blocks, thoracic epidural anesthesia, and spontaneous breathing anesthesia with laryngeal mask airway (LMA). Intravenous narcotics and conscious sedation are often combined with the techniques as above. After intravenous administration of fentanyl 25 to 50 mcg, target controlled infusion of propofol and/or remifentanil is started, aiming for BIS over 50 to 70 (24). Among them, thoracic epidural anesthesia is the most popular and can be enough.
Thoracic epidural anesthesia
The use of thoracic epidural anesthesia in awake thoracic surgery was first proposed in 1950 by Buckingham et al. (27,28). Recent studies have reported that thoracic surgery under epidural anesthesia can be easily and safely carried out with less charges and hospital-stay (10,24,29,30). However, it is a novel field to explore and investigate the benefits, risks and disadvantages of thoracic epidural anesthesia in nonintubated thoracic surgery, although the technique has been used in other surgeries for many decades.
Thoracic paravertebral block
Paravertebral block is an alternative technique that may offer a comparable analgesic effect and a better side-effect profile, which is associated with a reduction in pulmonary complications (31). Komatsu et al. found that paravertebral block could greatly contribute to enhanced recovery after thoracic surgery owing to effective and fewer side effects in a retrospective observational study (32). Katayama et al. suggested that paravertebral block was safe in patients ineligible for epidural block and could contribute to their pain relief following pulmonary resection procedure including VATS (33). However, the study of Messina et al. showed that epidural analgesia was more efficient than paravertebral continuous block at reducing pain after thoracic surgery (34).
Percutaneous or thoracoscopic intercostal nerve block
Hung and his colleagues reported that nonintubated thoracoscopic surgery using internal intercostal nerve block, vagal block and targeted sedation was technically feasible and safe in surgical treatment of lung, mediastinal and pleural tumors in selected patients (9). Wurnig et al. suggested that pain management by intercostal block was superior during the first 24 h after surgery whereas on the second day after surgery pain control was significantly better achieved by the epidural catheter in relaxed position. A combination of intercostal block and epidural block seems to be an ideal pain management in patients undergoing thoracic surgery (35).
Spontaneous breathing anesthesia with LMA
Cai and his colleagues found that thoracoscopic bulla resection under laryngeal mask anesthesia with low tidal volume high-frequency lung ventilation was safe and feasible and resulted in better patient satisfaction and shorter in-hospital stay than procedures performed under intubation anesthesia with one-lung ventilation (36). Ambrogi et al. suggested that thoracoscopic wedge resection of lung nodule was safe and feasible under spontaneous breathing anesthesia with LMA. It is a new technique permitted a confident manipulation of lung parenchyma and a safe stapler positioning without cough, pain, or panic attack described for awake epidural anesthesia, avoiding the risks of tracheal intubation and mechanical ventilation (37). However, it is influenced by surgical personal skills and patients with tenacious pleural adhesions or with nodule unsuitable for VATS resection must be excluded.
Cough control
Preoperative inhalation of aerosolized lidocaine and ipsilateral stellate ganglion block had been proposed to reach cough control in some extent (15,38). Chen and colleagues have routinely performed intraoperative thorascopic vagal block, and it has been proved effective on cough reflex suppression without causing hemodynamic instability (16). In some more cases, incremental intravenous fentanyl can be applied in place of vagal block to decrease cough suppression duration (24).
Respiration management
During the whole operation, nasopharyngeal airway and face mask are required for oxygen inhalation, with an oxygen flow of 3-5 L/min. After the pleural cavity is closed and the wound is sutured, the patients are assisted via a face mask in ventilation to inflate the lung tissue.
In sedated patients, premedication with opioid agent followed by deliberate titration had been proved to control respiratory rate effectively. Meticulous use of nasal airway can be of great benefit if upper airway obstruction raises clinical concerns. If significant hypoventilation happens, modest assisted ventilation by a mask may be required after notification of the surgical team. Oxygenation can be facilitated with O2 supplement by nasal cannula 3-4 L/min or by Venturi Mask. Overly hypercapnia should be avoided; a good-quality end-tidal CO2 trace and serial arterial blood sampling before/after iatrogenic open pneumothorax should suffice for close monitoring (24,28).
Postoperative analgesia
Thoracic epidural block is still the preferable standard for thoracic surgery analgesia with traumatic procedure. However, some anesthesiologists have some concern for epidural analgesia. Anticoagulant therapy with low molecular weight heparin has been increasingly used in surgical patients, which may make it difficult to safely manage the epidural analgesia. Bang and his colleagues reported a case of epidural hematoma in a 55-year-old male patient who had a thoracic epidural catheter placed under general anesthesia preceding a cardiac surgery. Epidural catheter insertion in a patient anticoagulated with heparin may increase the risk of epidural hematoma (39).
Ding and his colleagues reviewed the updated meta-analysis comparing the analgesic efficacy and side effects of paravertebral and epidural block for thoracotomy, showing that paravertebral block can provide comparable pain relief to traditional epidural block, and may have a better side-effect profile for pain relief after thoracic surgery (29). Recently, the systematic review of Steinthorsdottir et al. suggested that thoracic epidural block and especially paravertebral block showed some effect on pain scores for VATS in comparative studies (40). Certainly, a specified catheter for continuous paravertebral block would be more beneficial.
Ishikawa et al. have reported that for minimally invasive thoracoscopic surgery, intrapleural analgesia could be one of the good postoperative analgesia for its efficacy, safety, and benefit of easy placement of the catheter (41). Fibla et al. showed that the analgesic regimen combining paravertebral block and non-steroid anti-inflammatory drugs (NSAIDs) provided an excellent level of pain control for thoracoscopic surgery through a prospective randomized study (42).
The promising analgesia, including continuous intercostal-intrapleural analgesia or narcotic-based intravenous patient controlled analgesia combining with NSAIDs still need more attention and further study.
Advantages
Nonintubated anesthesia allows thoracic surgery patients to avoid the potential risks of tracheal intubation including the impacts from the manipulation, various anesthetic drugs and mechanical ventilation etc., particularly for the high-risk patients (43).
Liu et al. recently compared two groups of patients who received thoracic surgery under epidural anesthesia and those under general anesthesia with double lumen tube, the results showed significant differences in postoperative fasting time, duration of postoperative antibiotic use, and duration of postoperative hospital stay (30).
Mineo and his colleagues studied the quality of life after nonintubated versus intubated VATS talc pleurodesis using case-matched study recruited 391 patients, showing that two groups achieved similar results in pleural effusion and nonintubated VATS got earlier improvement of some quality-of-life domains as well as better mortality, morbidity, hospital stay, and costs (12).
Moreover, Vanni and his coworkers demonstrated that when compared with conventional thoracoscopic surgery under general anesthesia with single-lung ventilation, awake thoracoscopic surgery attenuated the surgical stress responses and had a smaller impact on the postoperative lymphocyte responses (44,45).
Disadvantages
Once mentioned of thoracic surgery just under epidural block, some anesthesiologists will recall the discomfort, irritation, and respiratory depression of the patients and the hustle and frustration of the anesthesiologists during upper abdominal surgery under epidural block decades years ago, even the anesthetics and monitor machines have made great developments. In addition, the thoracic epidural block has been abandoned in lots of hospitals. With heavy labor intensity and various degree of anxiety, anesthesiologists should keep monitoring without distractions and absences.
Some thoracic surgeons also disapprove with the nonintubated anesthesia, because they require that the patient should be unconscious, and are not satisfied with the surgical condition, worry about the position limitation and the possible body movement of the patient (46).
Some patients are not comfortable and even scared about being awake during the surgery, hearing the discussion and noises in the operating room, which may cause mental stress and post-traumatic stress disorder (PTSD). Although there is no related study, a normal human response to such an exceptional situation can for instance be the delayed appearance of unintentional distressing recollections of the event despite the patients’ satisfaction concerning the procedure (41,47).
Inexperienced and poorly cooperative surgical team may be the difficulties in performing the nonintubated anesthesia for thoracic surgery. The coordination and cooperation between surgeons and anesthesiologists are very important in operating room. The weak teamwork and poor communication could induce lots of problems even mistakes, seriously endangering the patients’ safety.
Hypercapnia can develop during nonintubated thoracic surgery and correlates with the operative time directly. Whereas it is worth noting that clinical study has shown that perioperative hypercapnia without hypoxemia rarely becomes clinically dangerous (13,48). Anyway, airway support and preparation for conversion to intubated general anesthesia should always be in hand in case of respiration depression, insufficient anesthesia and significant bleeding (15,24).
The charge of nonintubated anesthesia is quite lower than that of general anesthesia with double lumen endobronchial tube, and the anesthesiologists in some hospitals may get less economic benefits, for example, in the current bonus distribution system in China.
The advantages and disadvantages of nonintubated anesthesia for thoracic surgery are listed in the Table 1.
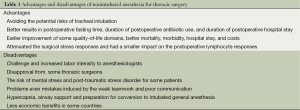
Full table
Future directions
In a modern era of minimally invasive thoracoscopic surgery, we are encouraged that tracheal intubation with double lumen tube or bronchial blocker is no longer regarded as a prerequisite for single lung ventilation in series of reported studies. Nonintubated thoracoscopic surgery is feasible and safe in a variety of thoracic procedures, including pulmonary resection, empyema, and excision of pleural and mediastinal tumors. Although the risks and benefits of this technique are not clear yet, it seems to offer an equally effective and safe alternative for those patients with high risks to intubated general anesthesia, and the postoperative recovery is faster with less complication rates.
Summary
The psychological preparation and physical evaluation of the patients, the applying of suitable techniques, intraoperative management and communication with surgeons are important for the safety and practicality of nonintubated anesthesia for thoracic surgery. Nevertheless, more evidence and studies are needed to ascertain the risks and benefits of this technique.
Acknowledgements
Disclosure: The authors declare no conflict of interest.
References
- Della Rocca G, Langiano N, Baroselli A, et al. Survey of thoracic anesthetic practice in Italy. J Cardiothorac Vasc Anesth 2013;27:1321-9. [PubMed]
- Ruetzler K, Grubhofer G, Schmid W, et al. Randomized clinical trial comparing double-lumen tube and EZ-Blocker for single-lung ventilation. Br J Anaesth 2011;106:896-902. [PubMed]
- Campos JH. Progress in lung separation. Thorac Surg Clin 2005;15:71-83. [PubMed]
- Komatsu T, Kino A, Inoue M, et al. Paravertebral block for video-assisted thoracoscopic surgery: analgesic effectiveness and role in fast-track surgery. Int J Surg 2014;12:936-9. [PubMed]
- Markar SR, Karthikesalingam A, Low DE. Enhanced recovery pathways lead to an improvement in postoperative outcomes following esophagectomy: systematic review and pooled analysis. Dis Esophagus 2014. [Epub ahead of print]. [PubMed]
- Hung MH, Hsu HH, Cheng YJ, et al. Nonintubated thoracoscopic surgery: state of the art and future directions. J Thorac Dis 2014;6:2-9. [PubMed]
- Klijian AS, Gibbs M, Andonian NT. AVATS: Awake Video Assisted Thoracic Surgery--extended series report. J Cardiothorac Surg 2014;9:149. [PubMed]
- Englbrecht JS, Pogatzki-Zahn EM. Perioperative pain management for abdominal and thoracic surgery. Schmerz 2014;28:265-81. [PubMed]
- Hung MH, Hsu HH, Chan KC, et al. Non-intubated thoracoscopic surgery using internal intercostal nerve block, vagal block and targeted sedation. Eur J Cardiothorac Surg 2014;46:620-5. [PubMed]
- Pompeo E, Mineo D, Rogliani P, et al. Feasibility and results of awake thoracoscopic resection of solitary pulmonary nodules. Ann Thorac Surg 2004;78:1761-8. [PubMed]
- Pompeo E, Rogliani P, Tacconi F, et al. Randomized comparison of awake nonresectional versus nonawake resectional lung volume reduction surgery. J Thorac Cardiovasc Surg 2012;143:47-54. [PubMed]
- Mineo TC, Sellitri F, Tacconi F, et al. Quality of life and outcomes after nonintubated versus intubated video-thoracoscopic pleurodesis for malignant pleural effusion: comparison by a case-matched study. J Palliat Med 2014;17:761-8. [PubMed]
- Mineo TC. Epidural anesthesia in awake thoracic surgery. Eur J Cardiothorac Surg 2007;32:13-9. [PubMed]
- Pompeo E, Tacconi F, Mineo TC. Awake video-assisted thoracoscopic biopsy in complex anterior mediastinal masses. Thorac Surg Clin 2010;20:225-33. [PubMed]
- Pompeo E, Mineo TC. Awake operative videothoracoscopic pulmonary resections. Thorac Surg Clin 2008;18:311-20. [PubMed]
- Chen JS, Cheng YJ, Hung MH, et al. Nonintubated thoracoscopic lobectomy for lung cancer. Ann Surg 2011;254:1038-43. [PubMed]
- Pompeo E, Rogliani P, Cristino B, et al. Awake thoracoscopic biopsy of interstitial lung disease. Ann Thorac Surg 2013;95:445-52. [PubMed]
- Pompeo E, Tacconi F, Mineo D, et al. The role of awake video-assisted thoracoscopic surgery in spontaneous pneumothorax. J Thorac Cardiovasc Surg 2007;133:786-90. [PubMed]
- Pompeo E, Mineo TC. Awake pulmonary metastasectomy. J Thorac Cardiovasc Surg 2007;133:960-6. [PubMed]
- Rocco G, Romano V, Accardo R, et al. Awake single-access (uniportal) video-assisted thoracoscopic surgery for peripheral pulmonary nodules in a complete ambulatory setting. Ann Thorac Surg 2010;89:1625-7. [PubMed]
- Rocco G, La Rocca A, Martucci N, et al. Awake single-access (uniportal) video-assisted thoracoscopic surgery for spontaneous pneumothorax. J Thorac Cardiovasc Surg 2011;142:944-5. [PubMed]
- Tseng YD, Cheng YJ, Hung MH, et al. Nonintubated needlescopic video-assisted thoracic surgery for management of peripheral lung nodules. Ann Thorac Surg 2012;93:1049-54. [PubMed]
- Wu CY, Chen JS, Lin YS, et al. Feasibility and safety of nonintubated thoracoscopic lobectomy for geriatric lung cancer patients. Ann Thorac Surg 2013;95:405-11. [PubMed]
- Yang JT, Hung MH, Chen JS, et al. Anesthetic consideration for nonintubated VATS. J Thorac Dis 2014;6:10-3. [PubMed]
- Lepage C, Drolet P, Girard M, et al. Music decreases sedative requirements during spinal anesthesia. Anesth Analg 2001;93:912-6. [PubMed]
- Bradt J, Dileo C, Shim M. Music interventions for preoperative anxiety. Cochrane Database Syst Rev 2013;6:CD006908. [PubMed]
- Buckingham WW, Beatty AJ, Brasher CA, et al. An analysis of 607 surgical procedures done under epidural anesthesia. Mo Med 1950;47:485-7. [PubMed]
- Pompeo E. Awake thoracic surgery--is it worth the trouble? Semin Thorac Cardiovasc Surg 2012;24:106-14. [PubMed]
- Ding X, Jin S, Niu X, et al. A comparison of the analgesia efficacy and side effects of paravertebral compared with epidural blockade for thoracotomy: an updated meta-analysis. PLoS One 2014;9:e96233. [PubMed]
- Liu J, Cui F, Li S, et al. Nonintubated Video-Assisted Thoracoscopic Surgery Under Epidural Anesthesia Compared With Conventional Anesthetic Option: A Randomized Control Study. Surg Innov 2014. [Epub ahead of print]. [PubMed]
- Wenk M, Schug SA. Perioperative pain management after thoracotomy. Curr Opin Anaesthesiol 2011;24:8-12. [PubMed]
- Komatsu T, Kino A, Inoue M, et al. Paravertebral block for video-assisted thoracoscopic surgery: analgesic effectiveness and role in fast-track surgery. Int J Surg 2014;12:936-9. [PubMed]
- Katayama T, Hirai S, Kobayashi R, et al. Safety of the paravertebral block in patients ineligible for epidural block undergoing pulmonary resection. Gen Thorac Cardiovasc Surg 2012;60:811-4. [PubMed]
- Messina M. A comparison of epidural vs. paravertebral blockade in thoracic surgery. Minerva Anestesiol 2009;75:616-21. [PubMed]
- Wurnig PN, Lackner H, Teiner C, et al. Is intercostal block for pain management in thoracic surgery more successful than epidural anaesthesia? Eur J Cardiothorac Surg 2002;21:1115-9. [PubMed]
- Cai K, Wang X, Ye J, et al. Laryngeal mask anesthesia in video-assisted thoracoscopic surgery for pulmonary bulla: comparison with intubation anesthesia. Nan Fang Yi Ke Da Xue Xue Bao 2013;33:756-60. [PubMed]
- Ambrogi MC, Fanucchi O, Korasidis S, et al. Nonintubated thoracoscopic pulmonary nodule resection under spontaneous breathing anesthesia with laryngeal mask. Innovations (Phila) 2014;9:276-80. [PubMed]
- Guarracino F, Gemignani R, Pratesi G, et al. Awake palliative thoracic surgery in a high-risk patient: one-lung, non-invasive ventilation combined with epidural blockade. Anaesthesia 2008;63:761-3. [PubMed]
- Bang J, Kim JU, Lee YM, et al. Spinal epidural hematoma related to an epidural catheter in a cardiac surgery patient -A case report-. Korean J Anesthesiol 2011;61:524-7. [PubMed]
- Steinthorsdottir KJ, Wildgaard L, Hansen HJ, et al. Regional analgesia for video-assisted thoracic surgery: a systematic review. Eur J Cardiothorac Surg 2014;45:959-66. [PubMed]
- Ishikawa Y, Maehara T, Nishii T, et al. Intrapleural analgesia using ropivacaine for postoperative pain relief after minimally invasive thoracoscopic surgery. Ann Thorac Cardiovasc Surg 2012;18:429-33. [PubMed]
- Fibla JJ, Molins L, Mier JM, et al. The efficacy of paravertebral block using a catheter technique for postoperative analgesia in thoracoscopic surgery: a randomized trial. Eur J Cardiothorac Surg 2011;40:907-11. [PubMed]
- Kiss G, Claret A, Desbordes J, et al. Thoracic epidural anaesthesia for awake thoracic surgery in severely dyspnoeic patients excluded from general anaesthesia†. Interact Cardiovasc Thorac Surg 2014;19:816-23. [PubMed]
- Vanni G, Tacconi F, Sellitri F, et al. Impact of awake videothoracoscopic surgery on postoperative lymphocyte responses. Ann Thorac Surg 2010;90:973-8. [PubMed]
- Tacconi F, Pompeo E, Sellitri F, et al. Surgical stress hormones response is reduced after awake videothoracoscopy. Interact Cardiovasc Thorac Surg 2010;10:666-71. [PubMed]
- Nakanishi R, Yasuda M. Awake thoracoscopic surgery under epidural anesthesia: is it really safe? Chin J Cancer Res 2014;26:368-70. [PubMed]
- Milian M, Tatagiba M, Feigl GC. Patient response to awake craniotomy - a summary overview. Acta Neurochir (Wien) 2014;156:1063-70. [PubMed]
- Laffey JG, O'Croinin D, McLoughlin P, et al. Permissive hypercapnia--role in protective lung ventilatory strategies. Intensive Care Med 2004;30:347-56. [PubMed]


