
Autopsy examination after extracorporeal membrane oxygenation: ‘Mortuis vivos docent’
Post-mortem examination is an important tool and one of the most consistent methods to corroborate clinical diagnoses. While autopsy studies in adult intensive care units (ICUs) have reported discrepancy rates between clinical and post-mortem findings ranging between 7% and 32% (1), major post-mortem discrepancies in other acute care settings, such as emergency departments, have been as high as 60% (2), underlining the fact that errors are more likely to happen when patients are sicker, and there is limited time to diagnose and treat their illnesses.
We read with interest the editorials written by Aludaat et al. (3) and Lorusso et al. (4) on our case series on autopsy and clinical discrepancies in adult patients who underwent extracorporeal membrane oxygenation (ECMO) at our institution (5). We agree with the authors that the challenges of making definitive diagnoses while the patient is on ECMO are considerable. We need to be vigilant and cognizant of subtle clinical changes that would otherwise escape attention, but even this may not be enough. We believe that post-mortem studies can add value and improve the quality of ECMO programmes by providing invaluable feedback, helping to ensure appropriate standards of clinical practice are maintained (6). Autopsy in ECMO patients can unravel some of the mysteries of rapid deterioration and highlight other contributory pathologies leading to better introspection by the clinical team with enhanced peer review learning.
Our analysis demonstrated that the incidence of major (class I/II) discrepancies was as high as 56%, with cardiovascular events being the most commonly missed entity. Myocardial infarction (MI) accounted for 63% of the discrepancies during autopsy (5). It has been shown that although critically ill patients are more vulnerable to cardiovascular events, the index of suspicion for cardiac etiology may be inappropriately low (1). Perkins et al. reported that only 55% of critically ill patients who had autopsies done actually had an electrocardiogram (ECG) performed during their stay in the ICU (7). However, ECG is performed and analysed almost every day in our ICU patients during ward rounds, yet autopsy still revealed MI as a major discrepancy in our series, which correlates with other published literature on MI as an autopsy discrepancy in non-ECMO patients (1). It has also been demonstrated that cardiovascular events were the leading cause of death in patients in other acute care settings, especially those who died within 48 hours of admission to emergency departments (2). The authors showed that cardiovascular diseases can present with diagnostic conundrums; acute aortic dissection and MI accounted for a great majority of class I missed diagnoses in their cohort (80% and 66.7% respectively). Major discrepancy rates for MI range between 13% and 28.3% of all autopsy cases outside the ICU setting (8). A recent study published earlier this year showed that type II MI, resulting from an improper myocardial oxygen supply-demand ratio, accounted for 85% of the patients with MI in this series (8). We believe that type II MI could be exacerbated in critically ill patients needing ECMO in multiple ways. First, the severity of disease presentation and rapidity of deterioration can contribute to the mismatch between oxygen supply and demand. Six out of the 19 patients in our series (32%) had ECMO during cardiopulmonary resuscitation, or a near arrest scenario. Second, patients on venoarterial ECMO are susceptible to differential hypoxemia during cardiac recovery resulting in Harlequin syndrome, which can lead less oxygenated blood circulating in the coronary arteries compared to the lower half of the body. The myocardium is especially vulnerable to this because of its physiologically high oxygen extraction ratio. Timely detection of this phenomenon would lead to a change in cannulation strategy (e.g., hybrid mode of ECMO) at an appropriate time to enhance oxygenated blood supply to the coronary arteries. We speculate that both these factors could have contributed to a higher incidence of MI in our series.
All our peripheral ECMO patients underwent femoro-femoral cannulation. Four patients had conversion from peripheral to central ECMO, or vice versa, in our series. These patients had significantly more discrepancies than those on central, or peripheral ECMO. Interestingly, three of these patients had peripheral ECMO initiated during cardiac arrest and needed conversion to central ECMO in view of severe left ventricular distension and poor ECMO flows (Table 1). The only patient who had central ECMO initiated, following a coronary artery bypass grafting with mitral valve replacement complicated by a ventricular tear that was appropriately detected and treated, had slight improvement in ventricular function that prompted conversion to axillo-femoral cannulation; however, the patient died from a massive stroke.
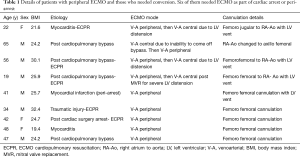
Full table
While we acknowledge the fact that autopsy rates have been declining in the last few decades, it can be partially attributed to the lack of incentives for performing it, in addition to a reduced number of expert pathologists who are trained to do it (9). Also, it is difficult to quantify the scientific benefits of autopsy in extremely sick patients who need extracorporeal life support. In addition, there are cultural and religious barriers to perform post-mortem examination, particularly in Asia. Higher rates of ECMO autopsies can be achieved by educating ICU staff as part of the teaching and quality assurance programs (6). Autopsy reports should be discussed in ECMO mortality meetings whenever available and learning points should be summarised for further action. Post mortem computerised tomography scans and magnetic resonance imaging scans have been found to be useful in analysing the cause of death (6). In combination with targeted biopsies, these ‘minimally invasive autopsy’ techniques may define the future of how we learn more about patients who die despite ECMO. Some of the autopsy discrepancies, or errors, represent accepted limitations of currently available investigations. The importance of autopsy and autopsy-detected diagnostic errors in the management of ECMO patients in an ICU setting cannot be overlooked. ‘Mortuis vivos docent’—The dead teach the living.
Acknowledgments
Funding: None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Tejerina E, Esteban A, Fernandez-Segoviano P, et al. Clinical diagnoses and autopsy findings: discrepancies in critically ill patients*. Crit Care Med 2012;40:842-6. [Crossref] [PubMed]
- Liu D, Gan R, Zhang W, et al. Autopsy interrogation of emergency medicine dispute cases: how often are clinical diagnoses incorrect? J Clin Pathol 2018;71:67-71. [Crossref] [PubMed]
- Aludaat C, Sarsam M, Doguet F, et al. Autopsy and clinical discrepancies in patients undergoing extracorporeal membrane oxygenation: a case series—a step towards understanding “Why”? J Thorac Dis 2019;11:S1865-8. [Crossref] [PubMed]
- Lorusso R, Corradi D. What you do not know, you do not recognize…and you do not improve future patient care…particularly in extracorporeal life support (ECLS) patients. J Thorac Dis 2019;11:S1930-4. [Crossref] [PubMed]
- Jia D, Neo R, Lim E, et al. Autopsy and clinical discrepancies in patients undergoing extracorporeal membrane oxygenation: a case series. Cardiovasc Pathol 2019;41:24-8. [Crossref] [PubMed]
- Wong A, Osborn M, Waldmann C. Autopsy and critical care. J Intensive Care Soc 2015;16:278-81. [Crossref] [PubMed]
- Perkins GD, McAuley DF, Davies S, et al. Discrepancies between clinical and postmortem diagnoses in critically ill patients: an observational study. Crit Care 2003;7:R129-32. [Crossref] [PubMed]
- Sathirareuangchai S, Shimizu D. Reaffirming the Value of the Autopsy. Am J Clin Pathol 2019;152:377-83. [Crossref] [PubMed]
- Shojania KG, Burton EC. The vanishing nonforensic autopsy. N Engl J Med 2008;358:873-5. [Crossref] [PubMed]


