|
Brief Report
Efficacy of percutaneous pigtail catheters for thoracostomy at bedside
Critical Care, Jersey City Medical Center, Jersey City, New Jersey, USA
|
|
Abstract
Objective: Given the potential morbidity of traditional chest tube insertion, use of pigtail is desirable. The purpose of this case series is to determine the efficacy of bedside pigtail thoracostomy catheters in Adult population by using bedside ultrasound by the pulmonologists. Methods: It is a retrospective case series, which describes the importance of bedside pigtail catheters placements for emergent symptomatic relief for the patients. Predicting a successful drainage, procedure is a complex and multifactorial process based on size, location, character and configuration of the abscess. Results: Our experience shows that the use of standard size (7-8.5 F) pigtail catheters is usually very successful in draining of the pleural fluids. Less time consumption, lower cost and bedside technique makes it superior to conventional chest tube placement in many aspects. Conclusion: Percutaneous pigtail catheters are useful in the drainage of pleural fluids. The pigtail catheters can be placed successful at bedside by the pulmonologists under ultrasound guidance with minimal complications and marked clinical improvement. The cost effectives of this procedure over the conventional chest tube placement, makes this procedure more desirable in most of the hospital settings. Key words
Pigtail thoracostomy catheters; bedside procedure; cast effective
J Thorac Dis 2012;4(3):292-295. DOI: 10.3978/j.issn.2072-1439.2011.12.01
|
|
Introduction
Thoracostomy tubes are a mainstay of treatment for removing fluid or air from the pleural space. Placement of a chest tube is, however, an invasive procedure with potential morbidity. Complications include hemothorax, perforation of intrathoracic organs, diaphragmatic laceration, empyema, pulmonary edema, and Horner’s syndrome (1-3). In an effort to reduce these complications, Fuhrman et al. (4) and subsequently Lawless et al. (5) described the use of percutaneous pigtail catheters in place of traditional large-bore tubes for thoracostomy and pleural drainage. The Seldinger needle-guide wire method of placement and smaller, more flexible catheters avoid the force required to place a large-bore chest tube by the dissection of trocar methods.
|
|
Materials and methods
Here, we will describe 5 cases in which successful bedside pigtail thoracostomy catheters were used.
Technique
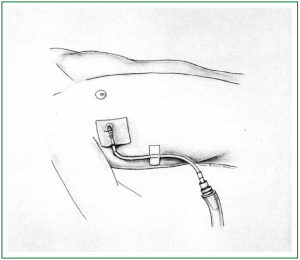
Percutaneous pigtail catheters were all single-lumen polyurethane coiled catheters, 7 to 8.5 F, used in conjunction with a wire and dilator, connected to a negative-pressure drainage system. The catheters were inserted using the modified Seldinger technique, with insertion of needle and syringe over a rib, with gentle aspiration of a syringe to locate either fluid or air in the pleura space. A J-tipped wire was then inserted and the needle removed. A dilator and scalpel were used to enlarge the insertion site, and the catheter was then inserted over the wire. Finally, the wire was removed and the catheter was attached to a drain. The procedure was placed under ultrasound guidance at bedside by the pulmonologist (Figure 1). No radiological or surgical help was requested.
Figure 1. Pigtail catheter allows less tension on the chest tube to decrease kinking of the catheter. The catheter is
sutured at the skin. A clear dressing is placed over the catheter.
Case description
Case I
44-year old African American male with a past medical history of HIV and hypertension presented to hospital with complaints
of shortness of breath at rest associated with fevers and chills
for past 1-2 days and no cough or sputum. On examination
patient was found to be in mild respiratory distress with no use
of accessory muscles and dullness of percussion throughout left
lung fields with minimal air entry in left lung field. Chest X ray
and CT chest revealed a massive pleural effusion of left lung and
associated lung collapse. A Fuhrman’s catheter was inserted at
bedside, under ultrasound guidance and a total of 2650 cc of
purulent fluid was drained over next 48 hours.
Pleural fluid analysis revealed it to be an exudative fluid
(LDH of 963 U/L, T protein 5.4 G/DL) with 31 polys and 56
lymphocytes. Pleural fluid culture grew Streptococci viridians.
Patient showed a rapid clinical improvement, but the catheter
stopped draining completely after 48 hrs. Persistence of effusions
on Chest X ray and Positive pleural cultures gave rise to a high
possibility of adhesions secondary to empyema. So TPA was
instilled into pleura, after which 750 cc more fluid drained out
in next 24 hrs. Catheter was removed after a total of 4 days,
after fluid stopped draining completely even after instillation
of another dose of TPA. Patient had an uneventful follow up
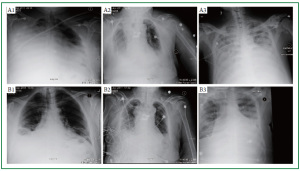
without any recurrence of symptoms (Figure 2A1, B1).
Case II
72-year old African American female with past medical history of
Non-squamous cell carcinoma of lung treated with radiotherapy
8 years back, and ischemic stroke with right sided hemiparesis
and dementia was admitted to hospital for shortness of breath
and found to have right lung mass obstructing right trachea
and positive for non small cell carcinoma on VATS. During
hospitalization patient was found to be in respiratory distress
and was found to have moderate amount of pleural effusion on
right side. All management options were discussed with family
who opt to change the patient’s code status to DNR/DNI but to
pursue all other aggressive measures for treatment.
Various modalities to deal with patient’s respiratory distress
were considered. Pigtail catheter was inserted at bedside under
ultrasound guidance. A total of 1400 cc of transudative fluid was drained in the next 24 hours and patient rapidly showed clinical
improvement and reached her baseline functional status (Figure 2A2, B2).
Case III
51-year old Hispanic male with past medical history of HIV,
Renal amyloidosis presents to ER with complaints of fever and
chills for past 3 days. Chest X ray revealed a right-sided pleural
effusion, which was showing possible loculations on the CT
chest suggesting empyema.
A pigtail was inserted at bedside and 800 cc of straw colored
pleural fluid was obtained. Pleural fluid analysis revealed
transudative fluid. Pleural effusion completely resolved on
subsequent Chest X rays. Patient was a febrile for rest of the
hospitalization and pigtail catheter was removed on 3rd day
without any complication.
Case IV
87-year old African American female with no significant past
medical history admitted to MICU for lower GI bleed stabilized
after 6 units of Packed Red blood cells and 2 units of Fresh
frozen plasma was found to be in Congestive heart failure and
developed bilateral pleural effusions.
As patient was in respiratory distress secondary to pleural
effusions, decision was made to place a pigtail catheter in right
pleural space. Patient drained 1200 cc of fluid in first 24 hrs
and showed rapid clinical improvement. Pleural fluid analysis
revealed it to be a transudate and catheter was removed on day 3
with near resolution of the respiratory symptoms.
Case V
47-year old African American male with past medical history of
restrictive cardiomyopathy and hypercalcemia, End stage renal
disease on hemodialysis presented with dyspnea of few hours
duration and was found to have bilateral pleural effusion left
greater than right. Patient was hypotensive at presentation with
increased WBC and fever suggesting presence of severe sepsis.
A pigtail catheter was placed at bedside as soon as a central line
catheter was place, both using ultrasound guidance. Patient
immediately improved symptomatically, and sepsis was treated
as per guidelines (Figure 2A3, B3).
|
|
Discussion
The use of thoracostomy tubes for draining pleural fluid or air is
an important therapeutic measure that ideally provides effective
drainage in a timely manner without complications from the
procedure. Traditional large-bore chest tubes, placed by either
blunt dissection or by trocar assistance, may have significant
morbidity associated with the force required to breech the chest wall and the stiffness of the chest tube itself. At the same
time, CT-guided pigtail replacement requires more expertise
and expenses. Development of a polyurethane pigtail catheter
by Fuhrman et al provided a potentially less traumatic bedside
technique alternative to the traditional methods.
In our experience, the catheters are simple to place in
critically ill patients. We found that pigtail catheters were very
effective in draining serous and chylous effusions. Further, they
were successful in draining blood or air, and empyema.
In contrast to our study, Fuhrman et al. (4) reported that 4 out
of 12 patients required further drainage procedures after initial
pigtail catheter placement. But none of our patient required any
further procedure for drainage.
In all our cases, though the rapidity of radiographic and
clinical improvement after pig tail insertion is very reassuring,
another important variable that needs to be considered is the
amount of time saved in doing a procedure at bedside under the
guidance of bedside ultrasound by the internist as opposed to
requesting a consult from a different service and coordinating
between two different specialties. The utility of a percutaneous
pigtail pleural drainage in various different settings as mentioned
in our clinical settings needs to be studied on a large scale and
adapted to a wider practice if reproducible.
Comparison of small-caliber chest tubes and standard chest
tubes in adult has shown that smaller tubes are more likely
to malfunction, and unlike conventional chest tubes, pigtail
catheters are easily compressed. But on the same time rate of
major complications including hemothorax, pneumothorax,
and liver perforation, was very low. There are some reported
minor complications including dislodgment, kinking, and
disconnection. But the rate of these complications was very low
and none of these complications were reported in our cases. |
|
Conclusion
Percutaneous pigtail catheters are useful in the drainage of
pleural air and fluids including serous, chylous and empyemic
collections. The pigtail catheters can be placed successful at
bedside by the pulmonologist under ultrasound guidance with
minimal complications and marked clinical improvement.
|
|
References
Cite this article as: Aziz F, Penupolu S, Flores D. Efficacy of percutaneous
pigtail catheters for thoracostomy at bedside. J Thorac Dis 2012;4(3):292-
295. doi: 10.3978/j.issn.2072-1439.2011.12.01
|