Video-assisted thoracoscopic surgery right upper posterior segmentectomywith systemic mediastinal lymph node dissection
Introduction
Lobectomy is the established procedure for earlystage non-small cell lung cancer (1). However, anatomic segmentectomy has been an optimized choicefor elderly patients and for patients with a compromised cardiopulmonary function (2). In addition, data in medical Literature have demonstrated an equivalent perioperative morbidity and mortality, as well as long-term outcomes of anatomic segmentectomy in patients with smaller tumors (especially ≤2 cm) compared with standard lobectomy (2). Video-assisted thoracoscopic surgery (VATS) approach to anatomic segmentectomy has become widely accepted, achieving similar oncological outcomes compared with the open techniques (3,4). Experienced hands and rigorous patient selection concerning individualized assessment of each patient and tumor characteristics will aid in benefiting more patients. In this video, we will present our operative techniques of VATS right upper posterior segmentectomy with systemic mediastinal lymph node (LN) dissection for the treatment of a 66-year-old male patient with a 1.6 cm suspicious lung nodule. The histology of the nodule was well differentiated adenocarcinoma, the post operative staging was T1aN0M0.
Operative techniques (Figure 1)
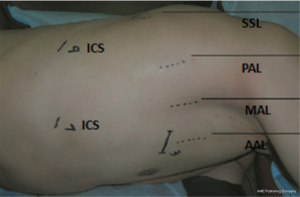
Port strategy (Figure 2)
First thoracoport (1 cm) was placed in the seventh intercostal space (ICS) at the mid-axillary line (MAL). The main utility incision (2.5 cm) was made at the anterior axillary line (AAL) in the third ICS. The assistant incision (1 cm) was placed in the ninth ICS [between the posterior axillary line (PAL) and subscapular line (SSL)].
Anatomic segmentectomy
The approach to thoracoscopic right upper posterior segmentectomy began with opening the oblique fissure. Incomplete oblique fissure could be divided via endoscopic stapler (Covidien Endo GIA stapler, blue staples). Any LNs encountered would be resected to facilitate further dissection of the posterior segmental artery and drainage vein, which would be encircled and transected together (Covidien Endo GIA stapler, white vascular staples). The next step was the dissection of the posterior segmental bronchus. Before closing the bronchus with the stapler, differential ventilation should be performed to confirm the target bronchus, and to define the correct intersegmental parenchymal plane. Then, the posterior segmental bronchus was transected (Covidien Endo GIA stapler, green staples) followed by division of the parenchyma (Covidien Endo GIA stapler, green and blue staples). The specimen would be retrieved in a self-made bag using a surgical glove.
Lymph nodes (LNs) dissection
Hilar LNs dissection and systemic mediastinal LNs dissection were routinely performed for an adequate staging according to the current oncological guidelines.
2R and 4R stations
Using the electrocoagulation hook (ECH), the dissection was initiated by opening the mediastinal pleura along the caudal border of the azygos vein and detaching the LNs block from the arch of azygos vein. Then, the mediastinal pleura was opened by the ECH along the upper border of the azygos vein and along the posterior border of the superior vena cava (SVC) to the caudal border of the innominate artery. With help of the metal endoscopic suction, the block would be hollowed out using the ultrasound scalpel (US) from the interspace surrounded by the arch of azygos, SVC, lower trachea, and ascending aorta. After the lower part of the block was free, it would be flipped over the arch of azygos vein. Next, the block was dissected off the posterior border of the SVC, the lateral border of the ascending aorta and the anterior border of the trachea sequentially from the upper border of the azygos vein to the caudal border of the innominate artery. At last, the block would be dissected longitudinally and anterior to the vagus nerve en bloc.
station
Dissection of the subcarinal LNs block was initiated by opening the mediastinal pleura using the ECH along the posterior border of the right intermediate and main-stem bronchi until approaching the arch of azygos vein. Small bronchial arteries and/or pulmonary branches of the vagus nerve were cut by the US. Then the subcarinal block would be dissected off the right intermediate and main-stem bronchi, pericardium, carina, esophagus, and the left main-stem bronchus.
Comments
In our experience executing VATS segmentectomy there are some tips and pitfalls.
The port strategy is constant with that we used for the single-direction thoracoscopic lobectomy (6) and it will aid the introduction of endoscopic stapler and straight metal endoscopic suction.
To accurately locate the target nodule buried in the parenchyma, we provide two modalities according to different situations: (I) if the chest CT scan shows that the tumor is ≥0.7 cm in diameter and ≤2 cm distant from the visceral pleura, digital palpation will be performed focusing on the target area containing the nodule. After the nodule been palpated, a marking suture is placed in the featureless pulmonary parenchyma on top of the nodule, guided by the surgeon’s finger; (II) preoperative CT-guided location by hook wire will be performed to the nodules ≥2 cm distant from the visceral pleura.
To find the correct artery and vein to posterior segment, opening the borderline between the oblique fissure and the horizontal fissure, and exposing the pulmonary artery is the first step. After dissected the oblique fissure with the endoscopic stapler, the artery to posterior segment will be exposed and the corresponding vein will be found nearby in most instances. Differential ventilation is used to aid confirming the border of the target segment. The target segment of which the bronchus is clamped will keep collapsing. If the tumor does not conform to discrete segmental boundaries, extended segmentectomy might be worth to obtain an adequate margin especially for a patient who has compromised pulmonary function and cannot bear a lobectomy.
The procedure of mediastinal LN dissection showed a non-grasping en bloc mediastinal LN dissection. When dissecting the subcarinal LNs, meticulousness should be retained to avoid injury to the membraneous portion of the right and left main-stem bronchi. Negative intersegmental LNs should be confirmed by frozen-section pathological examination. Otherwise, this approach should be converted to a VATS lobectomy.
Acknowledgements
Disclosure: The authors declare no conflict of interest.
References
- Vansteenkiste J, Crinò L, Dooms C, et al. 2nd ESMO Consensus Conference on Lung Cancer: early-stage non-small-cell lung cancer consensus on diagnosis, treatment and follow-up. Ann Oncol 2014;25:1462-74. [PubMed]
- Schuchert MJ, Abbas G, Pennathur A, et al. Sublobar resection for early-stage lung cancer. Semin Thorac Cardiovasc Surg 2010;22:22-31. [PubMed]
- Swanson SJ. Video-assisted thoracic surgery segmentectomy: the future of surgery for lung cancer? Ann Thorac Surg 2010;89:S2096-7. [PubMed]
- D’Amico TA. Thoracoscopic segmentectomy: technical considerations and outcomes. Ann Thorac Surg 2008;85:S716-8. [PubMed]
- Ma L, Liu C, Liu L. VATS right upper lobe posterior segmentectomy and lymphadenectomy. Asvide 2014;1:362. Available online: http://www.asvide.com/articles/396
- Liu L, Che G, Pu Q, et al. A new concept of endoscopic lung cancer resection: Single-direction thoracoscopic lobectomy. Surg Oncol 2010;19:e71-7. [PubMed]


