Thoracoscopic resection of functional posterior mediastinal paraganglioma: a case report
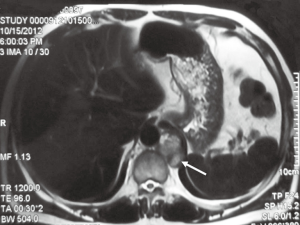
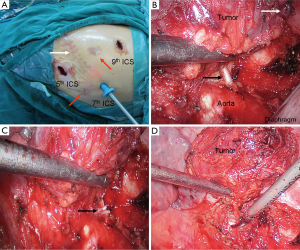
Case presentation (Figure 1)
A 48-year-old man was admitted to our center for a functional posterior mediastinal paraganglioma on the left side of the vertebrae. He suffered from hypertension for nine years with intermittent palpitation and headaches without significant family history. The tumor was found incidentally on abdominal computed tomography (CT) scan two months before admission. He underwent surgical exploration via open thoracotomy in another hospital previously. However, his blood pressure increased to 302/165 mmHg when touching the tumor and the operation was terminated. After previous surgery, plasma test of catecholamines showed that norepinephrine was 839 ng/L (ref range, less than 559 ng/L) and epinephrine was 2,340 ng/L (ref range, less than 122 ng/L). He was diagnosed as functional mediastinal paraganglioma and transmitted to our department later. Chest magnetic resonance imaging (MRI) scan was performed and revealed a 2 cm × 3 cm paravertebral mass centered at T11-T12 without vertebrae destruction (Figure 2). Abdominal contrast CT scan showed no abnormalities of the adrenal glands or the retroperitoneum. The patient was medicated with oral alpha- and beta-blockades, as well as intravenous Ringer’s solution (40 mL/kg/day) for two weeks. His hypertension was stabilized and a complete resection of the tumor was planned, using the thoracoscopic approach.
The patient was placed in the right lateral decubitus position after general anesthesia with double-lumen endotracheal intubation. Both arterial blood pressure and central venous pressure were monitored carefully during the operation. A 1-cm thoracoscopic port was made in the seventh intercostal space (ICS) on the midaxillary line. After thoracoscopic exploration, the other two 2-cm incisions were made in the fifth ICS on the anterior axillary line and in the ninth ICS between the posterior axillary line and the scapular line, respectively (Figure 3A). Pleural adhesiolysis was performed first. A 2 cm × 3 cm mass was found in the left side, adjoining the T11-T12 vertebral body. The patient’s blood pressure varied between 125/75 and 165/95 mmHg when cutting the pleura along the basement of the mass. After ligating the vein of the tumor, his blood pressure decreased to 90/50 mmHg, and intravenous norepinephrine was administered to maintain hemodynamic stability. En bloc resection of the tumor was achieved after transecting the nutrient artery derived from the descending aorta (Figure 3B-D). The tumor was removed using a bag made from a rubber glove.
Immunohistochemistry analysis revealed that chromogranin (CgA), synaptophysin (Syn) and S-100 protein were highly expressed in the tumor. The patient was finally confirmed as functional mediastinal paraganglioma. Intravenous medication of norepinephrine was gradually withdrawn on the operative day. His serum catecholamines recovered to normal level on postoperative day 3. The patient recovered uneventfully and stopped using antihypertensive drugs after surgery. He was discharged home on postoperative day 6, and had neither hypertension nor local recurrence during 18 months follow-up.
Discussion
Paragangliomas refer to a set of tumors arising from the chromaffin cells of the autonomic ganglia. Most of these tumors occur in the adrenal medulla and are commonly known as pheochromocytomas. Extra-adrenal pheochromocytomas account for about 15% of all the pheochromocytomas in adult patients (2), and can be classified as functional or non-functional paragangliomas based on the ability of synthesizing and releasing catecholamines (3). More than 75% of the extra-adrenal functional paragangliomas derive from organ of Zuckerkandl at the bifurcation of the aorta and the para-aortic region in the retroperitoneum (2). Functional mediastinal paragangliomas are rare, and most of them origin in the posterior mediastinum (4). These tumors may cause the same physiologic changes and symptoms as those occur in the adrenal medulla, or sometimes asymptomatic (4-7). The level of plasma free or urinary fractionated metanephrines is helpful in screening patients with functional paragangliomas (8). The possibility of functional paragangliomas can be virtually ruled out in patients with negative plasma free metanephrines. Additionally, 123I- or 131I-metaiodobenzylguanidine (MIBG) scan would provide detailed information on the function and location of these tumors, especially for the extra-adrenal lesions and metastases (9,10).
Preoperative diagnosis of ectopic pheochromocytoma is still more or less a challenge for thoracic surgeons. Some patients may be misdiagnosed as nonfunctional tumors until surgery due to insufficient preoperative assessment (3,6). Delayed diagnosis of these tumors caused unexpected critical hypertension when starting surgical resection of the tumor and severe hypotension or even shock after removing the tumor. This may put the patient in jeopardy. In the present case, functional paraganglioma was also ignored before the first operation in such a middle-aged man with early onset of hypertension combined with a posterior mediastinal neoplasm. The patient presented with incredible high blood pressure during the first operation when touching the tumor. As Sakamaki et al. and our previously reports (4,6), the operation could be safely continued in asymptomatic patients with functional paragangliomas diagnosed during the operation after preparation with antihypertensive drugs as well as sufficient fluid resuscitation. However, symptomatic patients with functional paragangliomas diagnosed during the operation have been rarely reported to be removed successfully with one-stage operation. When concerning the high risk of removing pheochromocytoma without effective preoperative preparation, we believe that it’s a wise choice to terminate the operation for this patient. When the patient was transmitted to our center, we assessed his blood catecholamines and thoracoabdominal imaging scan. The patient was clinically diagnosed as functional posterior mediastinal paraganglioma and no more lesions were identified before surgery. Though MIBG scan can help us in excluding whether there were any other lesions in this patient, we chose routine thoracoabdominal imaging techniques such as CT and MRI to evaluate the most common sites of paragangliomas. These techniques provided us more useful and detailed anatomical information for surgical decision. Postoperative decrease of plasma catecholamines and normalization of blood pressure confirmed that there no other lesions. The operation was then carried out after systemic preparation with drugs and blood volume expansion for two weeks to achieve a stable haemodynamic status.
Surgical resection is the most preferred treatment for patients with paraganglioma (9). For patients with adrenal pheochromocytoma or retroperitoneal paraganglioma, video-assisted endoscope has been increasingly adopted as a feasible and safe approach for operation (11). Intraoperative hemodynamic changes were the same in patients with adrenal pheochromocytoma who underwent video-assisted endoscopic or open operations (12). Thoracoscope has been widely applied in the treatment of thoracic diseases since last two decades, including the mediastinal neurogenic tumors (13). However, only a young girl with concomitant right adrenal pheochromocytoma and functional mediastinal paraganglioma has been reported underwent video-assisted endoscopic resection of the tumor (14). Most of the reported cases with functional mediastinal paraganglioma were removed via posterolateral thoracotomy. Even though the present case has undergone previous thoracotomy, we still planned a thoracoscopic operation for him after a careful evaluation of the chest MRI scan. When performing the operation, we tried our best to avoid squeezing the tumor in order to minimize the fluctuations of the patient’s blood pressure. The tumor was dissected along the basement. Nourishing blood vessels of the tumor were ligated when identified. An obvious decrease of arterial blood pressure was observed after ligating the drainage vein of the tumor. The anesthesiologist then medicated intravenous norepinephrine to maintain the patients’ blood pressure immediately. An experienced anesthesiologist is very important for the safety of such an operation. With effective co-operation with the anesthesiologist, the operation was finished uneventfully. Though thoracoscopic approach was successfully applied in the present case, we believe that thoracotomy should be preferred for tumors with abundant blood supply. After surgery, a regular follow-up is needed for these patients because both pheochromocytoma and functional paraganglioma are potentially malignant tumors.
In conclusion, functional mediastinal paragangliomas are still easily misdiagnosed and this should be taken into account in patients with unknown mediastinal neoplasm, especially those in the posterior mediastinum. Thoracoscopic resection of a functional mediastinal paraganglioma is feasible and safe in selected patients.
Acknowledgements
Disclosure: The authors declare no conflict of interest.
References
- Ma L, Mei J, Liu L. Thoracoscopic resection of functional posterior mediastinal paraganglioma: a case report. Asvide 2014;1:374. Available online: http://www.asvide.com/articles/408
- Whalen RK, Althausen AF, Daniels GH. Extra-adrenal pheochromocytoma. J Urol 1992;147:1-10. [PubMed]
- Soffer D, Scheithauer BW. Paraganglioma. In: Kleihues P, Cavenee WK. eds. Patholopy and Genetics of Tumours of the Nervous System. Lyon, France: IARC Press, 2000:112-4.
- Sakamaki Y, Yasukawa M, Kido T. Pheochromocytoma of the posterior mediastinum undiagnosed until the onset of intraoperative hypertension. Gen Thorac Cardiovasc Surg 2008;56:509-11. [PubMed]
- Suzawa K, Yamamoto H, Ichimura K, et al. Asymptomatic but functional paraganglioma of the posterior mediastinum. Ann Thorac Surg 2014;97:1077-80. [PubMed]
- Liu L, Mei J, Che G. Asymptomatic paraganglioma of the posterior mediastinum misdiagnosed until operation. Thorac Cardiovasc Surg 2010;58:302-4. [PubMed]
- Paul S, Jain SH, Gallegos RP, et al. Functional paraganglioma of the middle mediastinum. Ann Thorac Surg 2007;83:e14-6. [PubMed]
- Lenders JW, Pacak K, Walther MM, et al. Biochemical diagnosis of pheochromocytoma: which test is best? JAMA 2002;287:1427-34. [PubMed]
- Young WF Jr. Paragangliomas: clinical overview. Ann N Y Acad Sci 2006;1073:21-9. [PubMed]
- Spector JA, Willis DN, Ginsburg HB. Paraganglioma (pheochromocytoma) of the posterior mediastinum: a case report and review of the literature. J Pediatr Surg 2003;38:1114-6. [PubMed]
- Walz MK, Alesina PF, Wenger FA, et al. Laparoscopic and retroperitoneoscopic treatment of pheochromocytomas and retroperitoneal paragangliomas: results of 161 tumors in 126 patients. World J Surg 2006;30:899-908. [PubMed]
- Vargas HI, Kavoussi LR, Bartlett DL, et al. Laparoscopic adrenalectomy: a new standard of care. Urology 1997;49:673-8. [PubMed]
- Liu HP, Yim AP, Wan J, et al. Thoracoscopic removal of intrathoracic neurogenic tumors: a combined Chinese experience. Ann Surg 2000;232:187-90. [PubMed]
- Qazi A, Najmaldin A, Powis M. Combined laparoscopic and thoracoscopic excision of pheochromocytoma and functional paraganglioma. J Laparoendosc Adv Surg Tech A 2007;17:704-6. [PubMed]


