
Completion pneumonectomy is safe and effective in select patients with recurrent non-small cell lung cancer
Introduction
Locoregional recurrence following surgical resection for non-small cell lung cancer (NSCLC) varies according to stage, but affects upwards of 30% of patients following curative (R0) surgery (1-5). National Cancer Care Network (NCCN) guidelines (6) advocate surgery for locoregional recurrence in patients without evidence of distant disease, but completion pneumonectomy, specifically for recurrent cancer, is sparingly represented in available literature (7-13). Published studies demonstrate mortality rates up to 36% and substantial morbidity, but often include patients undergoing completion pneumonectomy for benign lesions, primary lung cancer and metastatic disease indications, making extrapolation to the NSCLC population challenging. We sought to evaluate perioperative outcomes and survival among patients who underwent completion pneumonectomy for recurrent NSCLC, with and without preoperative chemotherapy or chemoradiotherapy.
Methods
This study was approved by institutional review board of Brigham and Women’s Hospital (No. 2006P002482). We reviewed records from all patients who underwent completion pneumonectomy for recurrent NSCLC at our institution between 2000–2015. Patient demographics, morbidity and mortality statistics and survival data were extracted from the medical record into a database. Preoperative chemotherapy or chemoradiotherapy data were also collated. Statistical analysis was performed using STATA 14.1 (Stata Statistical Software, College Station, TX: StataCorp LP). Comparative analysis was performed with the Chi-Square test. Survival was calculated using the Kaplan-Meier method and was statistically evaluated by the log-rank test. A P value of less than 0.05 was considered significant.
Results
A total of 31 patients underwent completion pneumonectomy for suspected recurrent NSCLC between 2000 and 2015. On final pathologic review, three patients were believed to have new, unrelated second primary lung cancers and were eliminated from the overall survival analysis, leaving 28 patients for analysis. This included 14 women and 14 men (Table 1). Median time from index surgery was 34 months (range, 5–228 months). Median age at surgery was 64.2 years. There were 11 left-sided and 17 right-sided resections. The most common prior resection was a right upper lobectomy (n=8, 28.6%), followed by left lower lobectomy (n=6, 21.4%). Two patients had undergone prior bilobectomy. Four patients (14.3%) had positive resection margins noted on final path following their index procedure (prior to completion pneumonectomy). One patient had documented N2 disease at the time of initial resection.
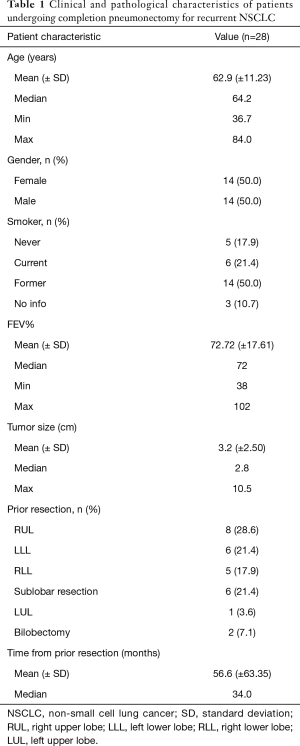
Full table
Patients considered for completion pneumonectomy for this indication undergo a thorough evaluation prior to surgery. All patients had a recent computed tomography (CT) scan prior to surgery. Twenty patients (71.4%) underwent pre-pneumonectomy positron emission tomography (PET) scanning and two underwent pre-pneumonectomy bone scans, as was the standard practice at this institution prior to 2003. All patients underwent preoperative pulmonary function studies. Median percent predicted FEV1 was 72%. Nineteen patients (67.9%) underwent preoperative echocardiogram. All patients examined by echocardiogram had documented normal right and left ventricular function. The lowest documented ejection fraction was 53% (range, 53–72%).
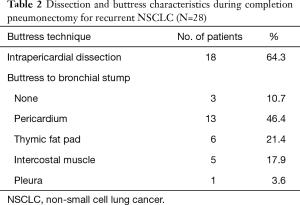
All patients underwent standard posterolateral thoracotomy. Most patients underwent intrapericardial dissection for control of hilar structures during pneumonectomy (n=18, 64.3%). Nearly all mainstem staple lines were reinforced with a soft tissue buttress (n=25, 89.3%), most commonly with pericardium (n=13, 46.4%), followed by thymic fat pad (n=6, 21.4%), and intercostal muscle (n=5, 17.9%) (Table 2). Median length of stay was 8 days. Fourteen patients received chemotherapy, radiotherapy or both prior to pneumonectomy. The majority of patients were N0 following pneumonectomy. Six patients (21.4%) exhibited N1 nodal disease on final pathology, and one patients had N2 disease (3.6%). Two patients (7.1%) had final positive margins after completion pneumonectomy, one at the chest wall margin and one at the bronchial margin.
Full table
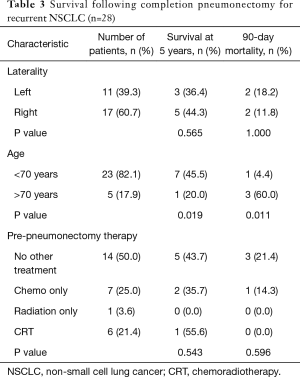
Overall survival at 5 years was 43.1% (Table 3). Mortality at 30 days was 3.6% and at 90 days was 14.3% (n=4) and did not differ according to laterality of resection.
Full table
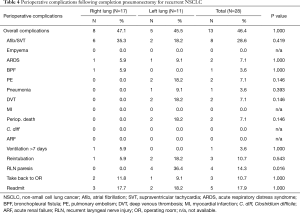
Pre-pneumonectomy chemoradiation was not associated with a difference in survival or morbidity. Postoperative complication rate was 46.4% (Table 4). Patients over 70 years old (n=5) experienced a statistically higher rate of postoperative complications (100.0% vs. 34.8%, P=0.013). Left-sided resections were associated with increased risk of recurrent laryngeal nerve injury (RLN) compared to right-sided resections (36.4% vs. 0%, P=0.016), and those patients with RLN injury were more likely to be reintubated (50.0% vs. 4.2%, P=0.04). Bronchopleural fistula occurred in 1 patient (3.6%).
Full table
Discussion
Survival in patients facing recurrent lung cancer is quite poor, and completion pneumonectomy can be daunting as depicted in the available literature, which describes discouraging morbidity and mortality rates (8-11). Yet with improvements in local and systemic therapies for NSCLC, thoracic surgeons are likely to encounter patients with recurrent NSCLC without overt contraindications to radical re-resection by completion pneumonectomy. Published series report on heterogeneous cohorts of patients, including those who underwent completion pneumonectomy for benign conditions or metastatic disease from other primary sites, making extrapolation of survival data challenging. Patients undergoing primary pneumonectomy for the treatment of NSCLC at this institution over the same time period experienced a 5-year overall survival rate of 38.5%. This study concludes that survival rates comparable to primary pneumonectomy can be achieved when facing recurrent disease and re-operative surgery. Interestingly, 7 patients (25.0%) had undergone more than one prior resection, making the pneumonectomy a third-time re-operative strategy. Nine patients had prior muscle flap or fat pad coverage of the bronchial stump, which did not appear to affect safe dissection of the hilar structures. In one case, the prior muscle flap was removed and replaced onto the bronchial stump after pneumonectomy.
Little is published regarding the impact of preoperative chemoradiotherapy on completion pneumonectomy, regardless of histology or indication. In this study, 50.0% of patients received chemotherapy or chemoradiotherapy prior to completion pneumonectomy. Within the constraints of small sample size, this does not appear to confer a survival advantage. While intuitively, re-operative surgery in the context of chemotherapy and/or radiation could imply a hostile hilar dissection, this does not appear to translate into increased perioperative complications or mortality. However, completion pneumonectomy, as a whole, conferred a 14.3% 90-day perioperative mortality rate, compared to 7.9% for patients who underwent primary pneumonectomy at the same institution over the same time period.
Recurrent laryngeal nerve paralysis occurred in 4 patients (36.4%) who underwent left completion pneumonectomy, which is higher than published studies of primary pneumonectomy (5% at this institution). This was clinically significant in that there were more reintubations among those patients. Adhesions along the arch of the aorta and mediastinum as well as desmoplastic changes relative to tumor and/or treatment affect may affect preservation of the recurrent laryngeal nerve and predispose to paresis. It is important to consider and discuss this with patients prior to radical resection, particularly of left sided tumors.
While age-related trends in survival did not reach statistical significance, all patients over 70 experienced a complication, and mortality in this age group was higher, approaching significance at 60 days (P=0.07), and significant at 90 days (P=0.01). Therefore, age is an important consideration when weighing options for the treatment of locally recurrent lung cancer and may argue for the inclusion of more advanced scoring systems or scales as part of the risk stratification process to aid the identification of patients who will not benefit from completion pneumonectomy.
Limitations of this retrospective review include our inability to capture patients with recurrent disease who were not offered or refused surgery for recurrent disease, which would infer a selection bias. Patients undergoing pneumonectomy in this study were quite fit with high functional status and normal right and left ventricular function. The majority of patients did not have mediastinal nodal disease. Our study would not have captured patients who underwent attempted, but aborted resection, in the setting of node-positive disease, though we expect this represents a rare exception.
Exciting advances in screening, surgical and systemic strategies for NSCLC are changing the landscape of lung cancer and may afford operability to patients previously deemed unresectable. It is feasible that the role of completion pneumonectomy will expand as thoracic surgeons are presented with healthier patients with localized disease, or disease controlled with novel chemo and immunotherapeutic agents. This study demonstrates that completion pneumonectomy, in thoughtfully selected patients, can achieve reasonable survival results. Preoperative evaluation for locoregional nodal disease and metastatic disease should be standard, and considerable attention to functional status and cardiopulmonary reserve is essential. Soft tissue buttress of the bronchial stump is recommended as routine, and intrapericardial dissection is particularly useful to delineate hilar structures in the setting of repeated prior surgery, adhesions and treatment related changes. Careful attention to the recurrent laryngeal nerve, along with expeditious diagnosis and treatment of nerve palsy is crucial in left sided resections.
Acknowledgments
Funding: None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. This study was approved by institutional review board of Brigham and Women’s Hospital (No. 2006P002482).
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Uramoto H, Tanaka F. Recurrence after surgery in patients with NSCLC. Transl Lung Cancer Res 2014;3:242-9. [PubMed]
- Kozu Y, Maniwa T, Takahashi S, et al. Risk factors for both recurrence and survival in patients with pathological stage I non-small-cell lung cancer. Eur J Cardiothorac Surg 2013;44:e53-8. [Crossref] [PubMed]
- Wright G, Manser RL, Byrnes G, et al. Surgery for non-small cell lung cancer: systematic review and meta-analysis of randomised controlled trials. Thorax 2006;61:597-603. [Crossref] [PubMed]
- Deslauriers J, Grégoire J. Surgical therapy of early non-small cell lung cancer. Chest 2000;117:104S-109S. [Crossref] [PubMed]
- Whitson BA, Groth SS, Duval SJ, et al. Surgery for early-stage non-small cell lung cancer: a systematic review of the video-assisted thoracoscopic surgery versus thoracotomy approaches to lobectomy. Ann Thorac Surg 2008;86:2008-16; discussion 2016-8.
- National Comprehensive Cancer Network. Non-Small Cell Lung Cancer (Version 3.2018). Available online: http://www.nccn.org/professionals/physician_gls/pdf/nsclc.pdf. Accessed April 6, 2018.
- Cardillo G, Galetta D, van Schil P, et al. Completion pneumonectomy: a multicentre international study on 165 patients. Eur J Cardiothorac Surg 2012;42:405-9. [Crossref] [PubMed]
- Tabutin M, Couraud S, Guibert B, et al. Completion pneumonectomy in patients with cancer: postoperative survival and mortality factors. J Thorac Oncol 2012;7:1556-62. [Crossref] [PubMed]
- Kasprzyk M, Sławiński G, Musik M, et al. Completion pneumonectomy and chemoradiotherapy as treatment options in local recurrence of non-small-cell lung cancer. Kardiochir Torakochirurgia Pol 2015;12:18-25. [Crossref] [PubMed]
- Puri V, Tran A, Bell JM, et al. Completion pneumonectomy: outcomes for benign and malignant indications. Ann Thorac Surg 2013;95:1885-91. [Crossref] [PubMed]
- Miller DL, Deschamps C, Jenkins GD, et al. Completion pneumonectomy: factors affecting operative mortality and cardiopulmonary morbidity. Ann Thorac Surg 2002.74876-83; discussion 883-4. [Crossref] [PubMed]
- Grégoire J, Deslauriers J, Guojin L, et al. Indications, risks, and results of completion pneumonectomy. J Thorac Cardiovasc Surg 1993;105:918-24. [Crossref] [PubMed]
- Fujimoto T, Zaboura G, Fechner S, et al. Completion pneumonectomy: current indications, complications, and results. J Thorac Cardiovasc Surg 2001;121:484-90. [Crossref] [PubMed]


