
Combined non-invasive scan and biomarkers to identify independent risk factors in patients with mild coronary stenosis
Introduction
Cardiovascular diseases (CVDs) are leading causes of death and disability all over the world in which the coronary heart disease (CHD) induces one-third of all deaths in the population older than 35 years in western countries (1-3). In China, the mortality rate caused by CHD was around 106 per 100,000 according to the China Health and Family Planning Commission’s Statistical Yearbook-2015 (4). Clinical examination of patients with coronary heart disease still mainly focuses on morphological characteristics, e.g., luminal stenosis, currently. In general, mild coronary stenosis is often reckoned with a slight risk without the consideration of intervention, but studies have shown that even in patients without coronary stenosis, 25% of whom will develop the acute coronary syndrome. Previous angiographic studies demonstrated that the majority of myocardial infarctions occur due to the occlusion of arteries that previously did not present angiographically significant (>50%) stenosis. This indicates that the isolated morphological assessment of the degree of the coronary stenosis is unable to accurately predict the occurrence of MACE events. Especially for mild coronary stenosis, the precise evaluation of risk factors for MACE events could help physicians to devise a more patient-suitable revascularization strategy and aid in the prediction of future ischemic events.
Detailed recognition of coronary plaque components has been investigated intensively in recent years, which is more promising in the prediction of MACE events (5-7). Coronary computed tomographic angiography (CCTA) has been extended to the identification of morphology and properties of plaques indicating the stability. Moreover, the unfavorable characteristics of plaques detected by CCTA were capable of predicting the occurrence of acute coronary syndromes (ACS), independently of age and gender, etc. (8-10). However, related trials revealed that the uncertainty on management decisions for patients with significant CVDs after CTA examination because the positive predictive value of CTA for significant CVDs remains moderate (11), indicating that anatomic characteristics of plaques provided by CCTA alone may not be reliable. In addition, the hemodynamic environment of impaired arteries plays a vital role in the disease progression and management reportedly and thus computational dynamic simulations were extensively employed to investigate the stability of coronary plaques (12,13). It is worth to note that the fractional flow reserve (FFR) was proposed to quantify the functional performance of stenosed coronary arteries, and it has been accepted its effectiveness and importance in guiding treatment strategies (14). Unfortunately, due to its invasive feature and high-technique requirement, also with the consideration of high cost from the patients perspective, it has not been widely used in clinical practice (15).
Besides, previous studies have shown that blood biomarkers such as high-sensitivity C-reactive protein (hs-CRP), matrix metallopeptidase 9 (MMP-9) and myeloperoxidase (MPO) are also related to plaque stability and risk of cardiovascular disease (16,17), which indicated the potential ability of these three biomarkers in the prediction of MACEs. For instance, a great number of studies have demonstrated that hs-CRP helped predict cardiovascular outcomes and it could be a useful marker for predicting coronary angiographic severity progression with acute coronary syndromes. Thus, a better understanding of anatomic characteristics and functional properties (blood biomarkers) of coronary atherosclerotic plaque can help to evaluate risk factors and further forecast MACE events in patients with mild coronary stenosis.
In this study, varies risk levels of plaques were identified by CCTA images and the levels of hs-CRP, MMP-9 and MPO were measured simultaneously for patients who have mild coronary stenosis with chest pain. Thus, this study created a diversified pool mixed with plaques characteristics assessed through angiography images and the above-mentioned blood biomarkers, aiming to investigate independent risk factors associated with MACEs.
Methods
This protocol has been approved by the Tianjin Chest Hospital Ethics Committee. Before undergoing any study-related procedures, all patients agreeing to participate in the trial must sign a written informed consent.
Study population
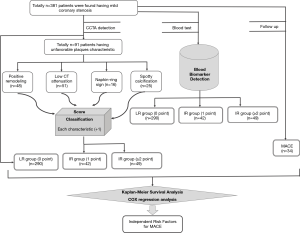
Totally 381 patients were detected having mild coronary stenosis after the CCTA examination, who went to our hospital due to chest pain from January 2015 to December 2016 (Figure 1). All these patients agreed to donate a blood sample for research purposes and signed the written informed consent forms.
Inclusion criteria: (I) patients with chest pain; (II) no obvious abnormalities in electrocardiogram (ECG) and treadmill exercise test; (III) no increase in myocardial enzymes-creatine kinase, creatine kinase-MB and trinitrotoluene; (IV) belong to a high-risk group for CHD: having two or more coronary heart disease risk factors. Exclusion criteria: patients with coronary stenosis of a luminal narrowing ≥50%, acute myocardial infarction, pulmonary embolism, aortic dissection, severe arrhythmia, cardiac insufficiency, NYHA Class III/IV, renal insufficiency and hyperthyroidism, or patients have allergic reactions to the contrast medium.
CCTA examinations
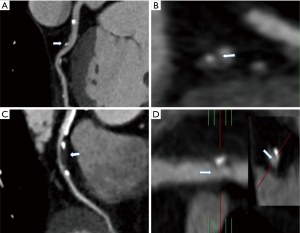
Dual-source CT (DSCT) scanner (SOMATOM DEFINITION CT, Siemens Healthcare, Forchheim, Germany) consists two sets of data acquisition systems which equipped with two X-ray tubes and corresponding detectors, with which we could obtain 64 overlapped slices with a thickness of 0.6 mm. The significant advantage of this DSCT scan for CHD detection is the highly improved temporal resolution. During the examination, contrast agent Uvita (370 mgI/100 mL, Bayer HealthCare Co., Ltd. Guangzhou Branch) or iohexol (350 mgI/100 mL, General Electric Pharmaceuticals) was injected through elbow veins using the double barrel syringes with a high pressure, at a flow rate of 3.5–4.5 mLs according to the patient's weight. Scanning for coronary artery calcification was performed firstly and the scan range was set from the plane of 10–15 mm below the tracheal branch to the heart diaphragmatic surface, with a tube voltage of 120 kV, a tube current of 100 mA, and the scan time was 6–10 s. Then, the coronary enhancement scan was performed and the images were processed with multi-layer reconstruction, surface reconstruction, maximum density projection, volume rendering procedures and cardiovascular optimization analysis software, selecting the optimal CT images to perform the assessment the coronary vascular plaque. Mild, moderate and severe stenosis induced by plaques in coronary arteries is defined as the luminal narrowing in the rage of <50%, 50–69%, ≥70%, respectively. Unfavorable plaque is defined as having at least one CT performance among the following items (18) shown in Figure 2:
- Positive remodeling: remodeling index (RI) equals the cross-sectional area of the largest stenosis divided by the average cross-sectional area of the proximal and distal reference segments. These two segments refer to the largest cross-sectional area from the stenosis site to proximal and distal direction with a maximum distance of 10mm in the same artery with no major branches, respectively. According to this RI value, the patients were divided into positive remodeling (RI ≥1.1), negative remodeling (RI <0.95) and no remodeling (RI =0.95–1.10).
- Low CT attenuation: in the non-calcified plaque lesions, select three regions of interest randomly (0.5–1.0 mm2) for CT value measurement. The resulting average CT value of less than 30 Hounsfield units is regarded as low CT attenuation.
- Napkin-ring sign (NRS): a central low-CT attenuated lesion that is connected to the lumen, surrounded by slightly high-attenuated plaque tissue.
- Spotty calcification: a piece of small calcified substance with a diameter less than 3 mm under the CCTA view, the length and the width do not exceed 1.5 times and 2/3 of the lumen diameter, respectively.
According to the scoring role, one unfavorable plaque characteristic was recorded for 1 point, the patients could be divided into low-risk group (no unfavorable plaque characteristic, 0 points, LR), intermediate-risk group (one unfavorable plaque characteristic, 1 point, IR), high-risk group (two or more unfavorable plaque characteristics, ≥2 points, HR).
Blood biomarker detection
Five milliliters of the venous blood sample was collected from each patient. Allow the sample to stand at room temperature and centrifuge at 3,000 rpm for 10 minutes, after which the isolated serum was stored in a centrifuge tube at −80 °C immediately for testing. Then left the thawed specimen at room temperature (18–25 °C) for at least 30 minutes and gradually configured the reagents for use according to the instructions. The hs-CRP and MMP-9 kits were purchased from Wuhan Huamei Bioengineering Co., Ltd., and the MPO kit was purchased from Tianjin Kanger Biotechnology Co., Ltd.
Follow-up
Follow-up was based on outpatient clinic visits at 1, 3, 6, 12, 18, and 24 months including telephone interviews. MACE events were recorded including cardiac death, nonfatal myocardial infarction and unstable angina requiring rehospitalization or revascularization.
Statistical methods
Statistical Package for Social Science (SPSS, v20.0) was employed for all statistical analyses and the measurement data were expressed as mean ± standard deviation. The t-test was used to investigate between-group differences while the count data were analyzed by χ2 test. The event-free survival rates of patients were compared through the Kaplan-Meier survival curve. The way to evaluate the predictive ability of medical scanning and biomarkers for adverse events in patients is COX regression method. Calculate the odds ratio (OR) and 95% CI. A P value of <0.05 was deemed to indicate significance.
Results
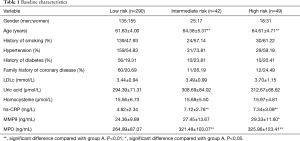
Baseline data comparison
The results of coronary enhancement scan and component analysis of plaques showed that 91 patients were diagnosed having unfavorable plaque characteristics: positive remodeling, n=48; low CT attenuation plaque, n=51; spotty calcium n=16; and NRS, n=25 (Figure 1). Consequently, the number of patients allocated in the LR group, IR group and HR group were 290, 42 and 49 respectively. All the variables presented in Table 1 were considered for both the univariate and stepwise analyses.
Full table
Follow-up results
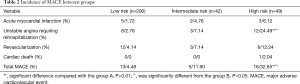
There were 178 males and 203 females aged between 35 to 88 years old with an average age of 62.32±4.42 years. In the end, 34 out of 381 patients occurred MACE (follow-up rate: 91%). One patient had cardiac death, and the acute myocardial infarction occurred in 10 cases, unstable angina occurred in 25 cases, and 21 patients underwent coronary revascularization. The incidence rates of unstable angina hospitalization and overall MACEs was much higher in the HR group than that in the LR group and the IR group. There were no significant differences in acute myocardial infarction, revascularization, and cardiac death between groups, as shown in Table 2.
Full table
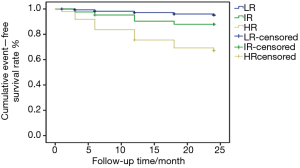
Kaplan-Meier survival analysis
Kaplan-Meier survival curves showed that the event-free survival rates of LR, IR and HR were 95.5%, 88.1%, and 67.3%, respectively. LR group was significantly higher than high-risk group (P<0.01), while IR group was higher than HR group (P<0.05), and it is no statistical difference (P>0.05) between LR and IR group, as shown in Figure 3.
COX regression analysis
Factors related to MACE events includes gender, age, smoking, hypertension, diabetes, family history, low-density lipoprotein cholesterol (LDLc), uric acid, homocysteine, hs-CRP, MMP-9, MPO, positive remodeling, low-CT attenuation, spotty calcification, napkin-ring sign and unfavorable plaque score ≥2 points were included for univariate analysis. Results suggest that age, hs-CRP, MMP-9, MPO, positive remodeling, low-CT attenuation, spotty calcification, NRS and unfavorable plaque score ≥2 points all have an effect on MACE events (P<0.05). On the contrary, gender, smoking, hypertension, diabetes, family history, LDLc, uric acid and homocysteine have no impact on MACE events (P>0.05), as shown in Table 3.
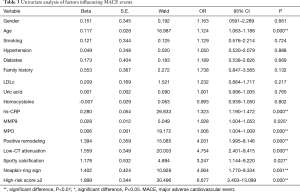
Full table
Multivariate COX regression analysis of above factors associated to the MACE events revealed that the age (OR =1.071, P=0.038), hs-CRP (OR =1.155, P=0.047), MPO (OR =1.005, P=0.006) and unfavorable plaque score ≥2 points (OR =9.533, P=0.045) are the significant factors to induce the occurrence of MACE events. However, MMP-9, positive remodeling, low-CT attenuation, spotty calcification and NRS have no obvious impact on clinical outcomes, as shown in Table 4.
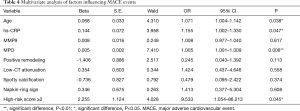
Full table
Discussion
The unfavorable plaques detected by CCTA have specific features: positive remodeling, low-CT attenuation, spotty calcification or NRS. The lesions with positive remodeling have a larger volume with more areas of necrotic centers; lipid-rich plaques present low-CT attenuation characteristic; the spotty calcification is a high-density small calcification material surrounded by non-calcified plaque tissue; the NRS shows a central low-CT attenuation lesion connected to the cavity, with a slightly high attenuation around the ring. These are comparative analyses between the large necrotic center (low attenuation in the center) and the fibrous plaque tissue (slightly higher attenuation in the ring). A plaque with these characteristics is extremely unstable and prone to result in plaque rupture. The formation of unfavorable plaques is accompanied by a series of inflammatory factors. Kohei et al. detected one patient has a thin fiber cap with vulnerable plaque characteristics by optical coherence tomography (OCT) and found that there was a remarkable increase of hs-CRP in the circulating blood (19). Silvello et al. found that expression level of MMP-9 increased significantly in patients with thinner fibrous caps or the acute intraplaque hemorrhage (IPH) occurred recently, suggesting that MMP-9 is associated with the formation of vulnerable plaques (20). MPO can enhance the instability of atherosclerotic plaque and even lead to plaque rupture. Fong et al. showed that hs-CRP, MPO and the soluble ligand CD40 were higher in patients with ACS compared with stable angina (21).
Levels of hs-CRP and MPO of patients in the IR group and the HR group were significantly higher than that in the LR group. Patients at high risk have higher MMP-9 level than those patients in the low-risk group, which revealed that the formation of unfavorable plaque is related to the biomarkers hs-CRP, MMP-9 and MPO.
It has been proved that plaques with unfavorable characteristics can predict a high risk of cardiovascular events independent of the stenosis degree (22,23). And low-CT attenuated plaques and their volume are important predictors of coronary events (24). Moreover, intravascular ultrasound studies found that heavily calcified plaques are clinically inactive, while spotty calcification has a tendency to worsen the stable angina condition (25). Otsuka et al. carried out a prospective study of 895 patients and they found that the NRS was an independent predictor of ACS. Blood biomarkers are also associated with cardiovascular disease risk (26). CRP can serve as a predictor of cardiovascular adverse events in both healthy population and patients with stable angina or acute coronary syndromes. Therefore, the American Heart Association (AHA) and the Centers for Disease Control and Prevention (CDC) recommend physicians to test the CRP level routinely to predict risk events of atherosclerosis (26). In another prospective study (27), ACS patients with elevated MPO level (>350 g/L) had a typically higher risk of myocardial infarction or death within 72 hours, 30 days, and 6 months. Furthermore, the MPO level was independent of troponin, CRP, and soluble CD ligand, suggesting that MPO level can provide different prognostic information compared to other biomarkers.
This study enrolled patients for a 24-month follow-up and major adverse cardiac events were recorded. Four specific features of unfavorable plaques involved in the Univariate COX analysis found that positive remodeling, low-CT attenuation, spotty calcification, and NRS have a significant difference to the occurrence of MACE events but not shown in the multivariate COX analysis. However, the unfavorable plaque score ≥2 points, hs-CRP and MPO levels were independent predictors for MACE events.
In addition, this study also found that the mean age of patients in the IR group and HR group was significantly higher than LR group, indicating that the volume and quantity of unfavorable coronary atherosclerotic plaques increased with age. In the multivariate COX analysis, age was correlated with prognosis, which was an independent risk factor for MACE events in patients who have mild coronary artery stenosis with chest pain.
Patients with unfavorable plaque characteristics of mild coronary stenosis are prone to serious cardiac adverse events if they were not treated in a timely and regular manner (28), which indicated that well-timed and effective individualized treatment was necessary to further reduce the occurrence rate of adverse cardiovascular events.
The limitation of this study is that the relationship between individual unfavorable plaque characteristic and prognosis has not been clearly clarified, which may be related to the co-existence of these unfavorable plaque features in majority cases. Recruiting a larger scale of the dataset, in order to find more subjects with a single characteristic of unfavorable plaque, would contribute to the analysis of the results.
Conclusions
At present, unfavorable plaques are primarily limited to the morphological investigation, and there is no data analysis combined this with the functional analysis. In recent years, coronary artery models, reconstructed through CT imaging data analyzed with computed fluid dynamics, have been simulated to obtain non-invasive FFR distribution. Hence, combining plaque morphology and the functional analysis can help to further identify unfavorable plaques more accurately using non-invasive methods for the early diagnosis of potentially acute clinical cardiovascular events (29). This study investigated a better characterization of plaques using both non-invasive imaging and biomarkers to identify patients at risk, suggesting that age, hs-CRP and MPO levels, and unfavorable plaque scores ≥2 were independent risk factors for MACEs, especially MPO level. This is a promising method to provide a more comprehensive evaluation and prediction tool in clinical practice. In the future, we will focus on the research relating to the combination of plaque morphological and functional study in more detail.
Acknowledgments
To all involved in the trial, the sponsor, the clinical teams in the participating sites, the manufacturer, the investigators, and particularly the patients.
Funding: This paper was supported by Tianjin Health and Family Planning Commission under the grants 14KG126 and 2015KY35 ‘Predictive value of high-risk plaques and biomarkers for cardiac events in patients with chest pain’. The funding body had no role in the design of the study beyond organizing peer review as part of the process of obtaining funding. The manuscript was fully written by the authors who expressed their views, without any considerations from the funding institution.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. This protocol has been approved by TianJin Chest Hospital Ethics Committee. All patients provided their consent for the publication of this study.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Roger VL. Epidemiology of myocardial infarction. Med Clin N Am 2007;91:537-52. [Crossref] [PubMed]
- Mozaffarian D, Benjamin EJ, Go AS, et al. Executive summary: heart disease and stroke statistics—2016 update: a report from the American Heart Association. Circulation 2016;133:447-54. [Crossref] [PubMed]
- Nichols M, Townsend N, Scarborough P, et al. Cardiovascular disease in Europe 2014: epidemiological update. Eur Heart J 2014;35:2950-9. [Crossref] [PubMed]
- Chen WW, Gao RL, Liu LS, et al. China cardiovascular diseases report 2015: a summary. J Geriatr Cardiol 2017;14:1. [PubMed]
- Maurovich-Horvat P, Ferencik M, Voros S, et al. Comprehensive plaque assessment by coronary CT angiography. Nat Rev Cardiol 2014;11:390. [Crossref] [PubMed]
- Tomizawa N, Yamamoto K, Inoh S, et al. High-risk Plaque and Calcification Detected by Coronary CT Angiography to Predict Future Cardiovascular Events After Percutaneous Coronary Intervention. Acad Radiol 2018;25:486-93. [Crossref] [PubMed]
- Lee JM, Choi G, Koo B-K, et al. Identification of high-risk plaques destined to cause acute coronary syndrome using coronary computed tomographic angiography and computational fluid dynamics. JACC Cardiovasc Imaging 2019;12:1032-43. [Crossref] [PubMed]
- Nabel EG. Braunwald EJNEJoM. A tale of coronary artery disease and myocardial infarction. New Engl J Med 2012;366:54-63. [Crossref] [PubMed]
- Dey D, Gaur S, Ovrehus KA, et al. Integrated prediction of lesion-specific ischaemia from quantitative coronary CT angiography using machine learning: a multicentre study. Eur Radiol 2018;28:2655-64. [Crossref] [PubMed]
- Liu T, Maurovich-Horvat P, Mayrhofer T, et al. Quantitative coronary plaque analysis predicts high-risk plaque morphology on coronary computed tomography angiography: results from the ROMICAT II trial. Int J Cardiovasc Imaging 2018;34:311-9. [Crossref] [PubMed]
- Puchner SB, Liu T, Mayrhofer T, et al. High-risk plaque detected on coronary CT angiography predicts acute coronary syndromes independent of significant stenosis in acute chest pain: results from the ROMICAT-II trial. J Am Coll Cardiol 2014;64:684-92. [Crossref] [PubMed]
- Matsuo Y, Higashioka D, Ino Y, et al. Association of Hemodynamic Severity With Plaque Vulnerability and Complexity of Coronary Artery Stenosis: A Combined Optical Coherence Tomography and Fractional Flow Reserve Study. JACC Cardiovasc Imaging 2019;12:1103-5. [Crossref] [PubMed]
- Liu X, Peng C, Xia Y, et al. Hemodynamics analysis of the serial stenotic coronary arteries. Biomed Eng Online 2017;16:127. [Crossref] [PubMed]
- Pijls NH, Sels JW. Functional measurement of coronary stenosis. J Am Coll Cardiol 2012;59:1045-57. [Crossref] [PubMed]
- Tesche C, De Cecco CN, Albrecht MH, et al. Coronary CT angiography–derived fractional flow reserve. Radiology 2017;285:17-33. [Crossref] [PubMed]
- Symons R, Choi Y, Cork TE, et al. Optimized energy of spectral coronary CT angiography for coronary plaque detection and quantification. J Cardiovasc Comput Tomogr 2018;12:108-14. [Crossref] [PubMed]
- Zakynthinos E, Pappa N. Inflammatory biomarkers in coronary artery disease. J Cardiol 2009;53:317-33. [Crossref] [PubMed]
- Dwivedi A, Al'Aref SJ, Lin FY, et al. Evaluation of atherosclerotic plaque in non-invasive coronary imaging. Korean Circ J 2018;48:124-33. [Crossref] [PubMed]
- Koyama K, Yoneyama K, Mitarai T, et al. Association between inflammatory biomarkers and thin-cap fibroatheroma detected by optical coherence tomography in patients with coronary heart disease. Arch Med Sci 2015;11:505. [Crossref] [PubMed]
- Silvello D, Narvaes LB, Albuquerque LC, et al. Serum levels and polymorphisms of matrix metalloproteinases (MMPs) in carotid artery atherosclerosis: higher MMP-9 levels are associated with plaque vulnerability. Biomarkers 2014;19:49-55. [Crossref] [PubMed]
- Fong SW, Few LL, Too WCS, et al. Systemic and coronary levels of CRP, MPO, sCD40L and PlGF in patients with coronary artery disease. BMC Res Notes 2015;8:679. [Crossref] [PubMed]
- Nadjiri J, Hausleiter J, Jähnichen C, et al. Incremental prognostic value of quantitative plaque assessment in coronary CT angiography during 5 years of follow up. J Cardiovasc Comput Tomogr 2016;10:97-104. [Crossref] [PubMed]
- Motoyama S, Ito H, Sarai M, et al. Plaque characterization by coronary computed tomography angiography and the likelihood of acute coronary events in mid-term follow-up. J Am Coll Cardiol 2015;66:337-46. [Crossref] [PubMed]
- Ozaki Y, Okumura M, Ismail TF, et al. Coronary CT angiographic characteristics of culprit lesions in acute coronary syndromes not related to plaque rupture as defined by optical coherence tomography and angioscopy. Eur Heart J 2011;32:2814-23. [Crossref] [PubMed]
- Otsuka K, Fukuda S, Tanaka A, et al. Napkin-ring sign on coronary CT angiography for the prediction of acute coronary syndrome. JACC Cardiovasc Imaging 2013;6:448-57. [Crossref] [PubMed]
- Pearson TA, Mensah GA, Alexander RW, et al. Markers of inflammation and cardiovascular disease: application to clinical and public health practice: a statement for healthcare professionals from the Centers for Disease Control and Prevention and the American Heart Association. Circulation 2003;107:499-511. [Crossref] [PubMed]
- Baldus S, Heeschen C, Meinertz T, et al. Myeloperoxidase serum levels predict risk in patients with acute coronary syndromes. Circulation 2003;108:1440-5. [Crossref] [PubMed]
- Takata K, Imaizumi S, Zhang B, et al. Stabilization of high-risk plaques. Cardiovasc Diagn Ther 2016;6:304. [Crossref] [PubMed]
- Min JK, Leipsic J, Pencina MJ, et al. Diagnostic accuracy of fractional flow reserve from anatomic CT angiography. JAMA 2012;308:1237-45. [Crossref] [PubMed]


