
Can parapneumonic effusion be diagnosed only with pleural fluid analysis?
Pleural effusion is a common medical problem caused by local disease in the pleura or underlying lung, systemic conditions, and organ dysfunction (1). The major causes of pleural effusion are congestive heart failure, pneumonia, cancer, and tuberculosis (Tb) (2). Systemic and expeditious evaluation is essential because a delay in diagnosing infectious disease is associated with increased morbidity and mortality (3). Infectious pleural effusion, called parapneumonic effusion, is the most common of exudative effusions (3). Although parapneumonic effusion can resolve with antibiotic treatment alone (uncomplicated parapneumonic effusion), a minority of patients undergo secondary bacterial infection of the pleural effusion leading to complicated parapneumonic effusion (4). Complicated parapneumonic effusions generally do not resolve without effusion drainage (4). Persistent pleural effusion can eventually result in the accumulation of pus in the pleural space (empyema) (4). Prevention of progression to complicated effusion can be aided by thoracentesis, if possible, for prompt diagnosis and treatment in patients at risk for parapneumonic effusion (5).
Light’s criteria has remained the standard method for differentiating exudative effusion via the following findings: a ratio of pleural fluid protein to serum protein greater than 0.5, a ratio of pleural lactate dehydrogenase (LDH) level to serum LDH level greater than 0.6, or a pleural fluid LDH level higher than 200 IU per liter (6).
When pleural infection is suspected, microscopic examinations of Gram stain, culture, and pH should be performed. However, fluid culture is only positive in empyema, with a low reported sensitivity (18–60%) (4,7), and time to incubation was 24 to 72 hours (8). Pleural low pH (<7.2) and low glucose (<40 mg/dL) have been assessed as additional features of complicated parapneumonic effusion; however, the sensitivity of these markers is reported to be below 50% (9). As of now, there are no absolute criteria for the diagnosis of uncomplicated parapneumonic effusion. Table 1 suggest that the biochemical features of pleural fluid could assist the diagnostic process.
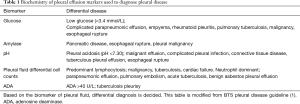
Full table
Ferreiro and colleagues introduced a model for detecting pleural fluid infection using biomarkers in pleural fluids, including C-reactive protein (CRP), leukocyte count, percentage of neutrophils, and IL-6 (10). They evaluated patients having undergone thoracentesis between June 1, 2013, and December 31, 2016 (10). Of the 706 cases, 241 were malignant, 28 were tuberculous, 177 were infectious, 48 were miscellaneous exudative effusion, and 212 were transudative effusion (10). Ferreiro’s group developed a predictive model using logistic regression based on a combination of leukocyte count, neutrophil count, CRP, and IL-6 (10). The area under the curve (AUC) of Model 1 used leukocyte, neutrophil, and CRP values for an AUC of 0.898 (95% CI, 0.866–0.935), and Model 2 added IL-6 to Model 1 for an AUC of 0.909 (95% CI, 0.882–0.937) (10). Elderly patients often do not present with the classic symptoms of cough, fever, sputum, and chest pain; as such, detecting infectious effusion based on pleural fluid analysis is crucial for these patients (3).
The characteristics of pleural fluid are well described in the Ferreiro study (10) and showed that a neutrophil-dominant differential cell count and the inflammatory markers CRP, procalcitonin, and IL-6 were higher in infectious effusion, consistent with previous studies (1,11).
In previous studies, each of the biochemical markers alone has lacked predictive power, with an AUC of 0.75–0.87 for pleural CRP, 0.57–0.59 for pleural procalcitonin, 0.75 for pleural leukocytes, 0.81 for pleural neutrophil count, and 0.54 for pleural lymphocytes (12,13). In infectious effusion, CRP and neutrophil values were significantly higher than for other exudative effusions; San and colleagues proposed a predictive model that uses the multiplied values of neutrophils and CRP (12). This model was reported to have a sensitivity of 64.3%, specificity of 93.4%, and AUC of 0.836 (12). In another study by the same group, a predictive model using IL-6 and pleural neutrophils only had a sensitivity of 25% and specificity of 100% (14). However, the predictive value of these models (12,14) remained lower than Ferreiro’s model (10), potentially because of omitting neutrophil percentages or relying on a crude multiplied value. San’s study population also had a higher percentage of tuberculous effusion (20–21%) than Ferreiro’s (3%), a population defined by high inflammatory markers (12,14).
Against this background, another investigation exploring other biomarkers that could be unique for infectious pleural effusion, such as soluble triggering receptor expressed on myeloid cells (sTREM-1) or lipopolysaccharide binding protein (LBP) showed AUCs of 0.79 (sTREM-1) and 0.80 (LBP) (13). These biomarkers did not, however, show an improved diagnostic value over previous inflammatory markers (13).
In the Ferreiro study (10), mean pH and glucose were within normal limits (WNL) during pleural infection although they included 65 cases of complicated infectious effusion and 38 of empyema in infectious effusion. pH and glucose are usually low in complicated parapneumonic effusion and empyema (4). Thus, infectious condition of Ferreiro study might have been less severe than other study’s populations, because pH and glucose are commonly assessed to detect complicated infectious effusions. Diagnosis of complicated parapneumonic effusion with a cut-off value of pleural pH below 7.2 had a sensitivity of 41% and specificity of 94%; that for glucose below 60 mg/dL had a sensitivity of 39% and specificity of 97%; and that for LDH greater than 1,000 U/L had a sensitivity of 74% and specificity of 83% (9). Porcel and colleagues suggested a model using TNF-α and LDH to improve accuracy that showed a sensitivity of 91% and specificity of 77% (9). TNF-α can also be elevated in tuberculous effusion (10) and thus cannot be used for differentiating between parapneumonic and tuberculous effusion; however, it may be an additional value for diagnosing complicated parapneumonic effusion (9).
In the Ferreiro study (10), although samples were collected continuously between June 1, 2013, and December 31, 2016, the percentage of tuberculous pleural effusion was 3%, which was much less than the 9% reported in Spanish epidemiology and other studies (2,12,14). Moreover, tuberculous pleural effusion also presented with high CRP and IL-6 values (although not neutrophil values) that might easily be misclassified as infectious pleural effusion (10). Since infectious and tuberculous effusions have common inflammatory features, a predictive model would perform poorly in areas with a high incidence of pulmonary Tb, such as the Philippines, India, Africa, and China (15). This predictive model also included IL-6, which is not generally screened for in hospital, rendering the model difficult to generalize to other hospitals.
Adenosine deaminase (ADA) is used to diagnose tuberculous pleurisy (16), with a widely accepted cut-off value in pleural fluid of 40 U/L (16). The sensitivity and specificity of ADA in the diagnosis of pleural Tb were 92% and 90%, respectively (16). However, one-third of parapneumonic effusions and two-thirds of empyemas present with ADA levels that exceed 40 U/L (17).
These data indicate that diagnosis should be based on the fact that parapneumonic effusion presents with predominantly polymorphonuclear leukocytes rather than lymphocytes and inflammatory markers, and suggest that a diagnosis should be made via a logical pathway that includes a high neutrophil count percentage combined AND high CRP AND low ADA, or high neutrophils AND very high CRP AND moderate ADA. This process is well suited to a decision tree model (18).
In a logistic regression model, the biochemical results, such as neutrophil, CRP, and ADA values, should be considered independent variables that render the decision process of the model different from a typical clinician’s diagnostic process. In the decision tree model, the probability of parapneumonic effusion is based on a combination of conditions, including high neutrophil and CRP values and a low ADA. Darooei and colleagues used a decision tree model to discriminate tuberculous from malignant effusion (19). The decision tree model could also be used for multiclass classifications that differentiate among infectious, tuberculous, malignant, and transudative effusion at once. Studies have shown that the random forest (20) and gradient boosting (21) models showed significantly higher discriminating power than logistic regression models and could also be used for multiclass classification. Deep learning is also incorporated into multi-class classification, with favorable accuracy thus far (22). In the future, these new models could significantly improve diagnostic precision and provide a differential probability for each disease.
Acknowledgments
Funding: None.
Footnote
Conflict of Interest: Both authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/jtd.2020.02.02). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work, and are committed to ensuring that questions related to the accuracy or integrity of any part of the work will be appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Maskell N. British Thoracic Society Pleural Disease Guidelines - 2010 update. Thorax 2010;65:667-9. [Crossref] [PubMed]
- Porcel JM, Esquerda A, Vives M, et al. Etiology of pleural effusions: analysis of more than 3,000 consecutive thoracenteses. Arch Bronconeumol 2014;50:161-5. [PubMed]
- Feller-Kopman D, Light R. Pleural Disease. N Engl J Med 2018;378:740-51. [Crossref] [PubMed]
- Chapman SJ, Davies RJ. Recent advances in parapneumonic effusion and empyema. Curr Opin Pulm Med 2004;10:299-304. [Crossref] [PubMed]
- Aboudara M, Maldonado F. Update in the Management of Pleural Effusions. Med Clin North Am 2019;103:475-85. [Crossref] [PubMed]
- Heffner JE, Brown LK, Barbieri CA. Diagnostic value of tests that discriminate between exudative and transudative pleural effusions. Primary Study Investigators. Chest 1997;111:970-80. [Crossref] [PubMed]
- Perez VP, Caierao J, Fischer GB, et al. Pleural effusion with negative culture: a challenge for pneumococcal diagnosis in children. Diagn Microbiol Infect Dis 2016;86:200-4. [Crossref] [PubMed]
- Lamy B. Blood culture time-to-positivity: making use of the hidden information. Clin Microbiol Infect 2019;25:268-71. [Crossref] [PubMed]
- Porcel JM, Vives M, Esquerda A. Tumor necrosis factor-alpha in pleural fluid: a marker of complicated parapneumonic effusions. Chest 2004;125:160-4. [Crossref] [PubMed]
- Ferreiro L, Lado-Baleato Ó, Suárez-Antelo J, et al. Diagnosis of infectious pleural effusion using predictive models based on pleural fluid biomarkers. Ann Thorac Med 2019;14:254-63. [Crossref] [PubMed]
- Tarn AC, Lapworth R. Biochemical analysis of pleural fluid: what should we measure? Ann Clin Biochem 2001;38:311-22. [Crossref] [PubMed]
- San Jose ME, Valdes L, Vizcaino LH, et al. Procalcitonin, C-reactive protein, and cell counts in the diagnosis of parapneumonic pleural effusions. J Investig Med 2010;58:971-6. [Crossref] [PubMed]
- Porcel JM, Vives M, Cao G, et al. Biomarkers of infection for the differential diagnosis of pleural effusions. Eur Respir J 2009;34:1383-9. [Crossref] [PubMed]
- San Jose ME, Valdes L, Gonzalez-Barcala FJ, et al. Diagnostic value of proinflammatory interleukins in parapneumonic effusions. Am J Clin Pathol 2010;133:884-91. [Crossref] [PubMed]
- Organization WH. Global Tuberculosis report 2015. 2015. Available online: http://apps.who.int/iris/bitstream/10665/191102/1/9789241565059_eng.pdf
- Shaw JA, Irusen EM, Diacon AH, et al. Pleural tuberculosis: A concise clinical review. Clin Respir J 2018;12:1779-86. [Crossref] [PubMed]
- Light RW. Update on tuberculous pleural effusion. Respirology 2010;15:451-8. [Crossref] [PubMed]
- Podgorelec V, Kokol P, Stiglic B, et al. Decision trees: an overview and their use in medicine. J Med Syst 2002;26:445-63. [Crossref] [PubMed]
- Darooei R, Sanadgol G, Gh-Nataj A, et al. Discriminating Tuberculous Pleural Effusion from Malignant Pleural Effusion Based on Routine Pleural Fluid Biomarkers, Using Mathematical Methods. Tanaffos 2017;16:157-65. [PubMed]
- Prinzie A, Van den Poel D. Random Forests for multiclass classification: Random MultiNomial Logit. Expert Systems with Applications 2008;34:1721-32. [Crossref]
- Friedman JH. Greedy function approximation: A gradient boosting machine. Ann Statist 2001;29:1189-232. [Crossref]
- Yuan X, Xie L, Abouelenien M. A regularized ensemble framework of deep learning for cancer detection from multi-class, imbalanced training data. Pattern Recognition 2018;77:160-72. [Crossref]


