Diagnostic ability of the Timed Up & Go test for balance impairment prediction in chronic obstructive pulmonary disease
Introduction
Falling is a common problem in elderly people including in subjects with chronic obstructive pulmonary disease (COPD) (1). Previous studies showed the incidence of falling in COPD patients varies from 25.0–31.7% (2,3). Hakamy et al. also showed that the incidence of falling in patients with COPD was significant higher than non-COPD subjects (44.9 per 1,000 person-years vs. 24.1 per 1,000 person-years) (4). The greater fall risk in COPD patients needs more consideration of modifiable factors. Besides negative effects on mortality and morbidity, falls are linked to poorer overall functional status and quality of life (5). Therefore, reducing the fall risk is very important and assessment of balance impairment in elderly especially in COPD should be addressed (6). Balance impairment should be evaluated in older adults including COPD as a screen for identifying individuals who may benefit from a multifactorial fall risk assessment. Although a balance impairment assessment is now recommended by the guidelines for pulmonary rehabilitation program, specific tests have yet to be suggested (7). A number of tests have been developed to quantitatively measure balance in the elderly population (8). The Timed Up and Go (TUG) test is recommended as a routine screening test for balance impairment and falls in older adults (9). Some studies indicated that the TUG could be used for predicting history of falling and exercise capacity in COPD (10-13). For example, Reynaud et al. (13) and Al Haddad et al. (11) suggest that a cut-off 11 and 12 seconds could predict fall in patients with COPD, respectively. However, there are few data regarding the cut-off point of the TUG test that could predict balance impairment in COPD patients. Therefore, the aim of this study was to examine the diagnostic ability of the TUG test for identifying balance impairment in COPD.
Methods
Study procedures
This cross-sectional study was conducted at a single visit in COPD patient at Maharaj Nakorn Chiang Mai Hospital, Chiang Mai, Thailand from November 2015 to October 2017. Balance tests were measured using the Berg Balance Scale (BBS) and the TUG test. A BBS score of ≤45 indicated balance impairment in this study (14). The demographic and clinical data including age, sex, body mass index (BMI), co-morbidity, lung function, severity of COPD, history of a fall in the previous year using the Elderly Falls Screening Test (EFST) (15), and history of acute exacerbation of COPD (AECOPD) were collected. In addition to the standard assessments at our COPD clinic, the St. George’s Respiratory Questionnaire (SGRQ) (16), the Thai version of COPD assessment test (CAT) (17), the modified Medical Research Council (mMRC) dyspnea scale (18), and six-minute walk test (6-MWT) (19) were utilized. Testing was also performed for visual deficits by using the Snellen chart (20) and detection of anxiety or depression using the Thai version of Hospital Anxiety and Depression Scale (HADS) (21). All tests including the BBS, the TUG test, and the single test of 6-MWT were performed by the same well trained physical therapist. The study was approved by the Research Ethics Committee [Institutional Review Board (IRB) approval number: MED-2558-03253, date of approval: 12 October 2015 and filed under Clinical Trials Registry (study ID: TCTR20151015001, date of approval: 15 October 2015). Before enrollment, written informed consent was obtained from all subjects. We used the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) guidelines for reporting this cross-sectional study (22).
Study population
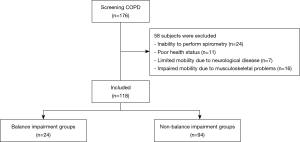
One hundred seventy-six COPD patients were screened for eligibility criteria from both clinical and medical record. The inclusion criteria were COPD patients, age ≥60 years, with no history of acute exacerbation for at least three months prior to enrollment. Diagnosis of COPD was based on smoking history of more than ten pack-years and post-bronchodilator (BD) ratio of forced expiratory volume in first second (FEV1)/forced vital capacity (FVC) of <0.7 (23). The exclusion criteria were subjects with neurological and musculoskeletal diseases that might affect the balance test were excluded. The subjects who have recently participated in exercise training program prior to study were also excluded.
Spirometry
All subjects were evaluated for lung function using a spirometer (Spiro Master PC, Chest M.I., Inc., Japan). Spirometry was performed according to the standards of American Thoracic Society (ATS)/European Respiratory Society (ERS) (24). Spirometric parameters were collected including FVC, FEV1, and ratio of FEV1/FVC. The predicted values were calculated using the Knudson’s reference equations (25). However, a correction factor of 0.94 was applied to the FVC and FEV1 predicted for Thai population (26).
Berg Balance Scale (BBS)
The balance test was measured by a physical therapist using the BBS in all subjects. This test was performed after the patients completed all questionnaires and spirometry. The BBS has more evidence for its psychometric properties than tests such as the Mini- Balance Evaluation Systems Test (BESTest) (7), and that the BBS has been more frequently used in the literature and clinical practice. Therefore, the BBS was selected for using in this study. The BBS includes 14 items for assessment of activities of daily living (ADL) tasks and is considered as the gold standard for testing static and dynamic balance abilities (27). In each task, the scores are classified from 0 (unable) to 4 (independent). The maximum score of 14-task items is 56, the lower score indicates a larger risk of falling and balance impairment. Previous finding suggested a cut-off score ≤45 as the risk of falling in community-dwelling adults (14). Therefore, a cut-off score of BBS ≤45 was defined as balance impairment in our study.
TUG test
The TUG test is a simple and widely used test of balance general mobility (28). The subjects were instructed to sit on an armchair of standard height before standing-up, walk three meters, turn around, walk back to the chair, and sit down on the chair again. The timing of the TUG started when the participant’s back lifted off the back of the chair and stopped when their buttocks retouched the seat of the chair. All subjects were instructed to perform the TUG test at their normal regular speed and gait aids were permitted when appropriate. For COPD patients treated with long-term oxygen therapy (LTOT), the test was performed without oxygen flow prescribed for walking. The TUG test was performed three times with a pause between repetitions with the shortest time selected.
Sample size calculation
The sample size of the study was calculated based on the data from the pilot study using the easy ROC: a web-tool for ROC curve analysis Version 1.3.1 (29) which consisted of 25 COPD subjects (twenty non-impaired balance and five impaired balance, ratio of sample size was four). The expected area under receiver operating characteristic curve (AUROC) of TUG test to indicate those who had impaired balance was 0.70. Therefore, at least 75 subjects (60 non-impaired balance and 15 impaired balance) were included in the study (power =0.8 with statistically significant <0.05).
Statistical analysis
Results for numerical data were expressed as mean ± standard deviation (SD) or median, interquartile range (IQR). Results with proportion were expressed as frequencies and percentages. Independent sample t-tests and Mann-Whitney U Test were used to compare differences between the groups for parametric and non-parametric data, respectively. Fisher’s exact test was used to compare the categorical data. To determine the diagnostic ability of TUG for assessing balance impairment, receiver operating characteristic (ROC) curves were constructed by plotting the true positive rate (sensitivity) against the false positive rate (1-specificity) for each scale level of the predictor variables for two dichotomous outcomes (balance impairment and non-balance impairment). The TUG was evaluated using sensitivity, specificity, positive likelihood ratio (LR+), negative likelihood ratio (LR−), Youden’s index, and AUROC from various points of TUG to identify the optimum cut-off point. Multivariable logistic regressions were performed to identify the TUG ≥12 seconds as a predictor for balance impairment in COPD when adjusted for other possible confounding factors including age, sex, cardiovascular co-morbidity, history of falling in the previous year, BMI, marital status, impaired visualization, and six-minute walk distance (6-MWD). Results were displayed as adjusted risk ratio (RR) together with a 95% confidence interval (CI) for RR. Statistical significance was accepted at the P value <0.05. All statistical analyses were performed using STATA version 15 (StataCorp., College Station, TX, USA).
Results
One hundred and eighteen COPD subjects were included after excluded 58 subjects due to various reasons including unacceptable spirometry, poor health status, and limited mobility due to neurological disease or musculoskeletal problems that defined by leading to early retirement from work, reduced accumulated wealth and reduced ability to participate in social roles. More details are shown in Figure 1. Eighty-six (72.9%) cases were males with a mean age of 73.5±8.1 years. Twenty-four (20.3%) cases were classified with balance impairment defined by the cut-off score of BBS ≤45 and 6 (5.1%) cases had history of falling in the previous year. The baseline characteristics of the balance impairment and non-balance impairment groups are shown in Table 1. There was no significant difference between the ratio of FEV1/FVC, percentage of predicted FEV1, GOLD classification, visual deficit, inhaled medications, cardiovascular comorbidity, anxiety and depression of subjects in the balance impairment and non-balance impairment groups. However, age, SGRQ score, CAT score, mMRC score, and TUG time in the balance impairment group were significantly higher than non-balance impairment groups. The balance impairment group had a significantly higher frequency of females. Furthermore, the balance impairment group had significantly lower percentage of predicted FVC, BBS score, and six-minute walk distance (6-MWD) compared to the non-balance impairment group.

Full table
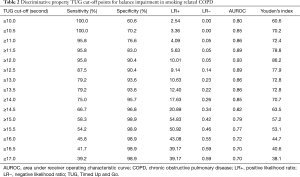
The sensitivity, specificity, LR+, LR−, and AUROC for each cut-off time of TUG are presented in Table 2. The cut-off TUG times of ≥12 seconds represented the highest AUROC (0.93), with sensitivity of 95.8% and specificity of 90.4%, the Youden’s index of 86.2 for detection of balance impairment in COPD.
Full table
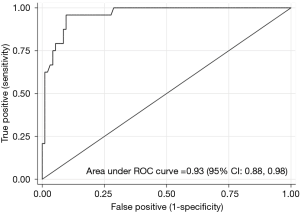
The TUG test demonstrated excellent overall accuracy relative to the balance impairment inpatients with COPD with an AUROC of 0.93 (95% CI: 0.88, 0.98) (Figure 2).
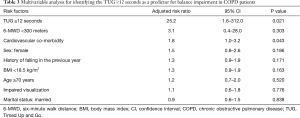
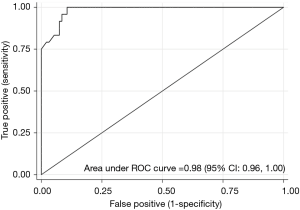
After adjustment for the possible confounding factors including age, sex, cardiovascular co-morbidity, history of falling in the previous year, BMI, impaired visualization, and exercise performance. Multivariable analysis showed that the TUG test time ≥12 seconds was the best predictor of balance impairment in COPD patients with adjusted RR of 25.2 (95% CI: 1.6, 312.0, P=0.021) (Table 3) and the AUROC was 0.98 (95% CI: 0.96, 1.00) (Figure 3).
Full table
Discussion
Falling and balance impairment in COPD are concerning issues. The previous studies showed a high proportion of falling in COPD patient (46%) (13,30) which were higher than our study (5.1%). The lower rate of falling of COPD patients in our study may be due to there were more family members’ supports and assist their daily activities than those in western countries as a large family type is common in Thai society. Therefore, the elderly persons have their relatives helping them on various activity daily living e.g.; housework, gardening, and shopping. Therefore, when the physical activity in COPD patients was reduced, the chance of falls is also reduced.
A balance assessment such as the TUG test is an integrated assessment of physical function, which consists of balance and gait speed (28). Our study demonstrated that the TUG test showed a high sensitivity, specificity, and AUROC for correct detection of balance impairment in COPD. Our study also showed that the TUG time was 6.6 seconds longer in COPD patients with balance impairment than non-balance impairment. This finding was higher when compared to the data from previous studies (range from 1.4–4.3 seconds) which might be explained by the higher age of subjects in our cohort (10,30,31).
To the best of our knowledge, this is the first study that shows the ability of TUG to identify COPD subjects with balance impairment. A previous study suggested that the BBS test is valid, reliable, and valuable in identifying the fall status in COPD patients (32). Moreover, the gap of knowledge was highlighted in a recent systematic review on the simple balance test such as TUG test in COPD (7). Thus, we explored the role of TUG for detection of balance impairment in this specific population. Our result indicates that the TUG test demonstrated excellent overall accuracy in prediction of balance impairment with high AUROC of 0.93 (95% CI: 0.88, 0.98). Moreover, multivariable analysis showed that the TUG ≥12 seconds was the best predictor of balance impairment in COPD patients with adjusted RR of 25.2 (95% CI: 1.6, 312.0, P=0.021) and the AUROC of TUG test time ≥12 seconds to indicate those who had impaired balance was 0.98 (95% CI: 0.96, 1.00). Therefore, we suggested a cut-off value of TUG ≥12 seconds as an indicator of balance impairment in this population. This threshold showed discriminative ability to identify subjects with balance impairment with high sensitivity (95.8%), specificity (90.4%), and AUROC (0.93). These results were similar to the previous findings (11-13). However, these studies used different outcomes including history of falling and exercise capacity. Previous studies published by Al Haddad et al. (11) and Reynaud et al. (13) suggested that the TUG test was found to predict falling with TUG of ≥12 seconds (sensitivity, specificity, and AUROC =74%, 74%, and 0.77, respectively) and ≥11 seconds (sensitivity and specificity =93% and 74%, respectively). Another studies indicated that the TUG could be used for a measure of physical performance (10,12). They showed that the TUG could be used as an excellent diagnostic ability to predict the exercise capacity (10,12). Cut-off values of TUG ≥11.2 seconds (AUROC =0.86) and ≥8.42 seconds (AUROC =0.826) corresponded to 350 and 360 meters of 6-MWDs, respectively (10,12). Applicably, in clinical practice, COPD patients whose TUG time was ≥12 seconds should receive any early interventions to prevent subsequent complications related to balance impairment or falling.
Strength and limitation of this study
This study has strengths that should be considered. To the best of our knowledge, this is the first study that identifies the TUG as a predictor for BBS-diagnosed balance impairment in COPD. However, this study has some limitations. Firstly, a healthy control group was not included in this study. Therefore, age-, sex-matched controls should be included to determine whether the TUG time differs in comparison with healthy elderly. Secondly, some baseline characteristics including age, sex, QOL, dyspnea score, exercise capacity, and cardiovascular comorbidity between balance impairment and non-balance impairment were different. Thus, the results of this study should be interpreted with caution. Thirdly, this is single-center study. The cut-off time of TUG for detecting balance impairment in COPD may be different in other clinical practices. Further research is needed to confirm these results. Fourthly, we used only the BBS for detecting balance impairment in COPD since the literature is rather clear on this subject on the fact that a multifactorial analysis e.g.; Performance-Oriented Mobility Assessment, the 30-Second Chair Stand test, the Mini-Balance Evaluation Systems Test (BESTest) and the 4-Stage Balance test must be cooperated with the BBS test (7,33,34).
Conclusions
Our study indicates the TUG test time ≥12 seconds has a high diagnostic ability for balance impairment prediction in COPD. The result supports a potential role for this simple test to be incorporated into routine COPD assessment to stratify patients’ balance.
Acknowledgments
The authors thank COPD patients who kindly participate in this study. The authors acknowledge the nurse and physical therapist staff members of the Division of Pulmonary, Critical Care and Allergy, Department of Internal Medicine, Faculty of Medicine, Chiang Mai University for their contribution to this trial.
Funding: None.
Footnote
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/jtd.2020.03.47). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was approved by the Research Ethics Committee [Institutional Review Board (IRB) approval number: MED-2558-03253, date of approval: 12 October 2015 and filed under Clinical Trials Registry (study ID: TCTR20151015001, date of approval: 15 October 2015). Before enrollment, written informed consent was obtained from all subjects.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Smith MD, Chang AT, Seale HE, et al. Balance is impaired in people with chronic obstructive pulmonary disease. Gait Posture 2010;31:456-60. [Crossref] [PubMed]
- Hellström K, Vahlberg B, Urell C, et al. Fear of falling, fall-related self-efficacy, anxiety and depression in individuals with chronic obstructive pulmonary disease. Clin Rehabil 2009;23:1136-44. [Crossref] [PubMed]
- Roig M, Eng JJ, MacIntyre DL, et al. Falls in people with chronic obstructive pulmonary disease: an observational cohort study. Respir Med 2011;105:461-9. [Crossref] [PubMed]
- Hakamy A, Bolton CE, Gibson JE, et al. Risk of fall in patients with COPD. Thorax 2018;73:1079-80. [Crossref] [PubMed]
- Cutson TM. Falls in the elderly. Am Fam Physician 1994;49:149-56. [PubMed]
- Crişan AF, Oancea C, Timar B, et al. Balance impairment in patients with COPD. PLoS One 2015;10:e0120573. [Crossref] [PubMed]
- Beauchamp MK. Balance assessment in people with COPD: An evidence-based guide. Chron Respir Dis 2019;16:1479973118820311. [Crossref] [PubMed]
- Mancini M, Horak FB. The relevance of clinical balance assessment tools to differentiate balance deficits. Eur J Phys Rehabil Med 2010;46:239-48. [PubMed]
- Beauchet O, Fantino B, Allali G, et al. Timed Up and Go test and risk of falls in older adults: a systematic review. J Nutr Health Aging 2011;15:933-8. [Crossref] [PubMed]
- Mesquita R, Wilke S, Smid DE, et al. Measurement properties of the Timed Up & Go test in patients with COPD. Chron Respir Dis 2016;13:344-52. [Crossref] [PubMed]
- Al Haddad MA, John M, Hussain S, et al. Role of the Timed Up and Go Test in Patients with Chronic Obstructive Pulmonary Disease. J Cardiopulm Rehabil Prev 2016;36:49-55. [Crossref] [PubMed]
- Albarrati AM, Gale NS, Enright S, et al. A simple and rapid test of physical performance inchronic obstructive pulmonary disease. Int J Chron Obstruct Pulmon Dis 2016;11:1785-91. [Crossref] [PubMed]
- Reynaud V, Muti D, Pereira B, et al. A TUG Value Longer Than 11 s Predicts Fall Risk at 6-Month in Individuals with COPD. J Clin Med 2019. [Crossref] [PubMed]
- Hawk C, Hyland JK, Rupert R, et al. Assessment of balance and risk for falls in sample of community-dwelling adults aged 65 and older. Chiropr Osteopat 2006;14:3. [Crossref] [PubMed]
- Cwikel JG, Fried AV, Biderman A, et al. Validation of a Fall-Risk Screening Test, the Elderly Fall Screening Test (EFST), for Community Dwelling Elderly. Disabil Rehabil 1998;20:161-7. [Crossref] [PubMed]
- Jones PW, Quirk FH, Baveystock CM, et al. A self-complete measure of health status for chronic airflow limitation. The St. George's Respiratory Questionnaire. Am Rev Respir Dis 1992;145:1321-7. [Crossref] [PubMed]
- Pothirat C, Chaiwong W, Phetsuk N, et al. Dialectal influence on chronic pulmonary disease assessment test: the reliability and validity study. Int J Chron Obstruct Pulmon Dis 2015;10:541-8. [Crossref] [PubMed]
- Bestall JC, Paul EA, Garrod R, et al. Usefulness of the Medical Research Council (MRC) dyspnoea scale as a measure of disability in patients with chronic obstructive pulmonary disease. Thorax 1999;54:581-6. [Crossref] [PubMed]
- ATS Committee on Proficiency Standards for Clinical Pulmonary Function Laboratories. ATS Statement: guidelines for the six-minute walk test. Am J Respir Crit Care Med 2002;166:111-7. [Crossref] [PubMed]
- Ricci F, Cedrone C, Cerulli L. Standardized measurement of visual acuity. Ophthalmic Epidemiol 1998;5:41-53. [Crossref] [PubMed]
- Zigmond AS, Snaith RP. The hospital anxiety and depression scale. Acta Psychiatr Scand 1983;67:361-70. [Crossref] [PubMed]
- von Elm E, Altman DG, Egger M, et al. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) Statement: guidelines for reporting observational studies. Int J Surg 2014;12:1495-9. [Crossref] [PubMed]
- Rabe KF, Hurd S, Anzueto A, et al. Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease. Am J Respir Crit Care Med 2007;176:532-55. [Crossref] [PubMed]
- Miller MR, Hankinson J, Brusasco V, et al. Standardisation of spirometry. Eur Respir J 2005;26:319-38. [Crossref] [PubMed]
- Knudson RJ, Lebowitz MD, Holberg CJ, et al. Changes in the normal maximal expiratory flow-volume curve with growth and aging. Am Rev Respir Dis 1983;127:725-34. [PubMed]
- American Thoracic Society. Lung function testing: selection of reference values and interpretative strategies. Am Rev Respir Dis 1991;144:1202-18. [Crossref] [PubMed]
- Bogle Thorbahn LD, Newton RA. Use of the Berg Balance Test to predict falls in elderly persons. Phys Ther. 1996;76:576-83. [Crossref] [PubMed]
- Podsiadlo D, Richardson S. The timed "Up & Go": a test of basic functional mobility for frail elderly persons. J Am Geriatr Soc 1991;39:142-8. [Crossref] [PubMed]
- Lopez-Raton M, Rodriguez-Alvarez MX, Suarez CC, et al. Optimal Cut points: An R Package for Selecting Optimal Cutpoints in Diagnostic Tests. J Stat Softw 2014;61:1-36. [Crossref]
- Beauchamp MK, Hill K, Goldstein RS, et al. Impairments in balance discriminate fallers from non-fallers in COPD. Respir Med 2009;103:1885-91. [Crossref] [PubMed]
- Porto EF, Pradella CO, Rocco CM, et al. Comparative Postural Control in COPD Patients and Healthy Individuals During Dynamic and Static Activities. J Cardiopulm Rehabil Prev 2017;37:139-45. [Crossref] [PubMed]
- Jácome C, Cruz J, Oliveira A, et al. Validity, Reliability, and Ability to Identify Fall Status of the Berg Balance Scale, BESTest, Mini-BESTest, and Brief-BESTest in Patients With COPD. Phys Ther 2016;96:1807-15. [Crossref] [PubMed]
- Panel on Prevention of Falls in Older Persons, American Geriatrics Society and British Geriatrics Society. Summary of the Updated American Geriatrics Society/British Geriatrics Society clinical practice guideline for prevention of falls in older persons. J Am Geriatr Soc 2011;59:148-57. [Crossref] [PubMed]
- Phelan EA, Mahoney JE, Voit JC, et al. Assessment and management of fall risk in primary care settings. Med Clin North Am 2015;99:281-93. [Crossref] [PubMed]