Standardizing education in interventional pulmonology in the midst of technological change
Introduction
Interventional pulmonology (IP) is a maturing subspecialty of pulmonary medicine with a focus on management of complex thoracic disorders with minimally invasive technology. IP encompasses the diagnostic and therapeutic approach of a variety of complex and challenging airway, lung and pleural disorders impacting patient outcomes and quality of life (1,2). The robust growth and innovation in technology with the emergence of new procedures including cryobiopsy, bronchoscopic lung volume reduction and robotic bronchoscopy have increased the diversity of interventional procedures offered. This has resulted in certification and formal training in IP throughout the globe. The United States (US), Australia, and some European nations have developed various forms of certification and formal training. China has recently developed national IP certification and designated accredited IP training centers. However, even with the recent adoption of formal IP fellowship training, the reality is that procedural training during fellowship only, will not last an entire career without learning new procedures and abandoning others learned during fellowship. The emphasis in modern fellowship training should incorporate methods to learn beyond fellowship training by collaborating with industry and global medical societies. Procedural training must evolve with technology.
Pulmonary medicine fellowship programs in the US and Canada typically do not provide the required number of interventional pulmonary procedures, with only about 30% of programs meeting the requirement (3,4). This creates an educational gap without defined standardized training and assessment of competency in performance of advanced airway and pleural procedures outside an IP fellowship. As a community of educators we are tasked to create a future best practice to fill this gap as discussed throughout this article. This is also true for pulmonary fellowship programs in Italy resulting in recognition of a 1-year fellowship in IP (5). Most US and Canadian IP fellowship programs provide a significantly higher number of basic and advanced interventional procedures than required by the American College of Chest Physicians (ACCP) and American Thoracic Society (ATS)/European Respiratory Society (ERS) guidelines (6). IP fellowship training in fact complements pulmonary medicine fellowship training and takes it to the next level.
Lahey Clinic (now Lahey Hospital & Medical Center, Burlington, MA, USA) was the first program to start a dedicated IP fellowship in the US in 1996, followed by an exponential growth in IP fellowship training programs over the last decade (7). There are existing opportunities to integrate training of specific procedures including advanced bronchoscopy in centers that have a pulmonary and critical care fellowship and IP fellowship programs. Currently 39 IP fellowship training programs in US and Canada participate in National Resident Matching Program (NRMP). The multi-societal accreditation of these programs as well as IP board certification, assures improved standardization in curriculum and procedural training. However, as newer technologies evolve, it becomes increasingly challenging to ensure competency beyond the scope of fellowship training.
Simulation based training
Simulation is an effective educational tool that facilitates repetitive training to improve psychomotor skills and assessment of decision making in a zero-risk environment. Simulation is being increasingly used in almost every industry with an ongoing growth and innovation in technology. Simulation and demonstration-based teaching has been found to be more effective than the classic didactics and lectures (8-10). Current evidence strongly suggests utilizing simulation in procedural training across all specialties (11). The American Board of Internal Medicine (ABIM) recommends simulation-based training as part of procedural training (12). The ATS and ACCP have strongly advocated including simulation in procedural training in pulmonary and critical care medicine (13). Patient-based procedural training (apprenticeship training model) alone may increase the risk of procedure-related complications and morbidity and brings up various ethical and liability issues. One study demonstrated that =trainee participation in procedures can increase the procedure time and required dose of sedative medications with the resultant increase in risk of complications (14).
Simulation is an essential part of training in medicine and specifically the procedure-based specialty of IP (15). Simulation can be of various types including low- and high-fidelity simulation, complex task trainers, computer virtual reality, augmented reality (AR) models and real time simulated scenarios (16). Debriefing and immediate feedback have been shown to improve skills and performance (17). Studies have shown that simulation-based bronchoscopy and endobronchial ultrasound (EBUS) training is associated with improvement in skills and time management as compared to typical apprenticeship training model alone (18-25). Simulation based training has shown promising results in various procedural training specialties including thoracic surgery, congenital heart surgery, endoscopic surgery, colorectal surgery, neurosurgery, extracorporeal membrane oxygenation (ECMO), vitreoretinal surgery, cataract surgery and interventional radiology (26-34). Numerous studies have proven that trainee performance in achieving basic competency in airway management, tube thoracotomy, thoracentesis, central venous catheter (CVC) placement and diagnostic radiology improved after incorporating simulation-based curriculum (35-47). Simulation can span low fidelity to high fidelity virtual reality and augmented reality platforms for single learner to multi-team learning across multiple disciplines. These can be focused as procedure-specific, disease-specific with realistic patient driven scenarios. AR platforms are underutilized and can create a cost effective and global classroom with interactivity that brings a shared classroom real-time with a limitless number of learners to provide procedure-based learning with faculty mentorship.
Simulation-based boot camp training is being increasingly utilized in various subspecialties with a significant improvement in trainee knowledge, skills and confidence (48). The American Association of Bronchology and Interventional Pulmonology (AABIP) has successfully arranged simulation-based boot camps at the beginning of each academic year for IP fellows in a flipped classroom model with the goal to improve education and training, as well as offer integrated online educational materials and IP specific symposia. A study showed that general pulmonologists and pulmonary fellows are less proficient in performing appropriate mediastinal staging using EBUS (49). To work towards a more standardized process and bridge this training gap, AABIP, ACCP and ATS host hands-on simulation procedure based training for pulmonary critical care fellows and general pulmonologists.
Although simulation-based training is important and should be part of the training curriculum, patient-based procedural training as an apprenticeship training model coupled with procedure volume are also necessary to establish competency that translates to successful independent clinical practice. Procedure volume has been shown to improve skill acquisition and proficiency in thoracic surgery as well as other procedure-based specialties (50). Simulation training is not meant to replace apprenticeship training but it should rather complement it.
Simulation training is a valuable option but there can be various barriers to its successful implementation including duty hour restrictions, scheduling problems and ongoing cost associated with buying and maintaining simulation equipment, a need for structured curriculum with objectives and having a simulation center facility and personnel. Simulation often lags behind as new procedures are developed. We need to collaborate with industry to establish models of training and create validated assessment tools for new technology.
Competency and mastery learning
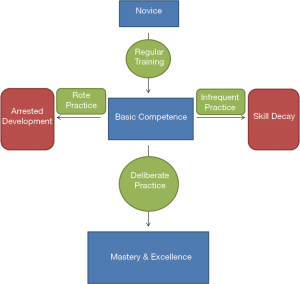
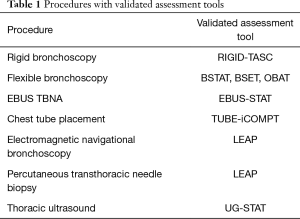
A deliberate practice model with rehearsal and editing of specific tasks under supervision and constructive feedback has been shown to achieve mastery learning (51-53). Basic competence skills and expertise can be achieved after a routine training period but they plateau if deliberate practice model is not adopted (51-53). Most experts in various professions including sports and music reach mastery level by using deliberate practice over years. Deliberate practice of at least 10,000 hours over 10–15 years has been consistently shown to achieve mastery level performance (Figure 1) (54-56). Simulation may be very helpful in achieving mastery learning by utilizing a deliberate practice model. Spaced practice or distributed practice refers to spacing out training sessions over time rather than practicing in one long session (massed practice). Massed practice training sessions are long and intense as compared to spaced or distributed practice. For example scheduling two rigid bronchoscopy training sessions in subsequent days or weeks (spaced practice) as compared to both on the same day (massed practice). Spaced practice has been recognized as a more efficient learning model for trainees with better skill acquisition and long term skill retention as compared to massed practice (57). Spaced practice reduces mental fatigue, demands increased trainee effort to attain proficiency level at practice sessions and leads to better memory consolidation, with the subsequent efficient learning. Simulation and spaced practice have been shown to improve acquisition of skills with a decrease in surgical adverse events in laparoscopic surgery training (57-60). Continued learning with the goal to improve procedure skills beyond a year of IP fellowship training can be challenging. Simulation, video recording and distance learning may be helpful. It is also important to assess for skill maintenance and improvement on a regular basis after achieving initial procedural competency as acquired skills can be lost if a particular procedure is not performed, a phenomenon often referred to as skill decay (61,62). Procedure volume is important but does not ensure procedural competency, due to variable learning curves for different trainees (63). Procedural competency should be assessed using a standardized knowledge and skills assessment system rather than procedural volume alone (64,65). The concept of competency and mastery training in medical procedures mandate validated assessment tools to assess knowledge and technical skills of the learner at various points during training due to variable learning curve (66). Basic competency skills can be assessed using well validated competency assessment tools (Table 1). A newer validated procedure assessment tool is available to measure basic competency in electromagnetic navigational bronchoscopy and percutaneous transthoracic needle biopsy (67). Studies have shown a significant variation in endobronchial ultrasound guided transbronchial needle aspiration (EBUS TBNA) learning curve among IP fellows even after performing 200 procedures (63,68). RIGID-TASC (Rigid Bronchoscopy Tool for Assessment of Skills and Competence) is a validated tool to assess basic competency in performing rigid bronchoscopy (69). EBUS-STAT (Endobronchial Ultrasound Skills and Task Assessment Tool) is another reliable tool to evaluate knowledge and skills in EBUS-TBNA procedure (70-72). Various assessment tools have been developed to assess competency in flexible bronchoscopy including BSTAT (Bronchoscopy Skills and Task Assessment Tool), BSET (Bronchoscopy Step-by-Step Evaluation Tool) and OBAT (Ontario Bronchoscopy Assessment Tool) (73,74). Chest tube placement proficiency can be assessed using TUBE-iCOMPT (Chest Tube Insertion Competency Test) (75).
Full table
IP fellowship training
IP has experienced an exponential growth over the last decade with a significant increase in the number of IP fellowship programs, fellowship-trained IP physicians and IP positions across various academic and non-academic institutions. IP training has become more standardized across the board due to a multi-societal accreditation process. The Association for Interventional Pulmonary Program Directors (AIPPD) and the AABIP have been instrumental in partnership with ACCP and ATS in promoting IP education and training through the formal accreditation process of IP fellowship programs, the IP board certification process as well as providing ongoing numerous opportunities in collaboration with industry for IP fellows through disease-specific and training-specific symposia.
An IP fellowship training curriculum should include (76-81);
- Structured formal didactics;
- Hands-on simulation-based training;
- Satisfactory procedure volume under faculty supervision and real time feedback;
- Quarterly review in a 360-degree fashion;
- Standardized curriculum.
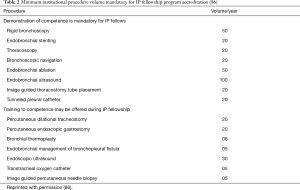
A similar training model has been used in robotic surgery, cardiothoracic surgery and vascular surgery with improved procedural proficiency of the trainees (82-84). A proficiency-based progression training model using simulation training has been shown to improve skills and proficiency (85). The multisociety interventional pulmonology fellowship accreditation committee has published guidelines regarding IP fellowship accreditation standards to standardize IP training across various IP training programs (86). Table 2 lists the minimum institutional procedure volume required per year for accreditation of an IP fellowship program (86).
Full table
AABIP has conducted annual IP board certification examinations since 2013. Completion of a dedicated year of IP fellowship training at an accredited IP fellowship program has been a requirement for taking the AABIP board certification exam since 2017 (87,88). The IP in-service examination is a reliable tool to assess trainee knowledge and provide feedback to fellowship program directors regarding their training curriculum (89). In-service examination performance has been shown to strongly correlate with the performance on a subspecialty certification examination, irrespective of various other factors related to the fellow and fellowship program (90).
Research and academic productivity
The importance of academic productivity and research cannot be overemphasized in any specialty. This is especially true for IP given the robust growth in technology and minimally invasive procedures. The academic productivity of IP training programs has been comparable to other procedural specialties (91). Scholarly activity including multi-center research will have a great impact on further growth and recognition of IP. Allocation of specific research time throughout fellowship training with well-defined research goals and expectations can help improve academic productivity of IP fellowship programs (92,93). Dedicated research time for IP faculty is equally important and expert mentorship of young fellows and faculty can help in successful academic career development (94). We suggest additional scholarship in education, i.e., formal training in education, publications and research in cognitive load, decision making, curriculum development and mixed methods research.
Ongoing education and training after fellowship
Mastery in procedure skills is a dynamic ongoing process beyond a dedicated year of IP fellowship training. Excellence at performing a complex task e.g., playing violin requires an average of 10,000 hours of deliberate practice (95). Faculty mentoring extending beyond a year of IP fellowship training coupled with additional procedure specific training can be very helpful in professional development (76). The ongoing evolution and innovation in technology and research requires IP physicians to maintain and update their procedural skills on a regular basis far beyond fellowship training. Practicing IP physicians need to be competent and up-to-date in new technology and procedural interventions. Didactic teaching and hands-on training sessions including simulation workshops offered at professional society meetings (AABIP, Chest and ATS), short 1–2-day training courses and mini-fellowships extending beyond the extent of introductory courses may be helpful in achieving the goal of procedural proficiency in the era of technologic change and maintain high standard of practice.
Recommendations
We need to work closely with the industry for early development of training models and formal training of new technology, using simulation and training courses. Encouraging distance learning with video recording assessment and feedback as seen in Europe and China can be an additional helpful option in achieving procedural proficiency.
Conclusions
The education and training in IP must be as innovative as the growing technology pushing this field forward. The use of augmented reality for global real time team based learning with video assessment/feedback, and simulators can allow IP practitioners to keep pace with technological changes. This will require the adoption of educators familiar with modern pedagogical practices and training. Program standardization and accreditation with both standard and flexible curricula, simulation-based training, continuous measures and ongoing assessment of competency skills will ensure progress toward sustained expertise and mastery.
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editors (Fabien Maldonado and Robert Lentz) for the series “Novel Diagnostic Techniques for Lung Cancer” published in Journal of Thoracic Disease. The article was sent for external peer review organized by the Guest Editors and the editorial office.
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/jtd.2020.03.104). The series “Novel Diagnostic Techniques for Lung Cancer” was commissioned by the editorial office without any funding or sponsorship. HJL is an educational consultant for Veran Medical, Veracyte and Intuitive. CRL is an educational and product development consultant for Boston Scientific and Veracyte. WA has no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Pastis NJ, Silvestri GA, Shepherd RW. Quality-of-life improvement and cost-effectiveness of interventional pulmonary procedures. Clin Chest Med 2013;34:593-603. [Crossref] [PubMed]
- Mondoni M, Radovanovic D, Sotgiu G, et al. Interventional pulmonology techniques in elderly patients with comorbidities. Eur J Intern Med 2019;59:14-20. [Crossref] [PubMed]
- Pastis NJ, Nietert PJ, Silvestri GA. Variation in training for interventional pulmonary procedures among US pulmonary/critical care fellowships: a survey of fellowship directors. Chest 2005;127:1614-21. [Crossref] [PubMed]
- Stather DR, Jarand J, Silvestri GA, et al. An evaluation of procedural training in Canadian respirology fellowship programs: program directors' and fellows' perspectives. Can Respir J 2009;16:55-9. [Crossref] [PubMed]
- Corbetta L, Patelli M. Executive Summary of Training and Competence Standards for the Interventional Pulmonology Master Program in Italy. J Bronchology Interv Pulmonol 2018;25:6-8. [Crossref] [PubMed]
- Yarmus L, Feller-Kopman D, Imad M, et al. Procedural volume and structure of interventional pulmonary fellowships: a survey of fellows and fellowship program directors. Chest 2013;144:935-9. [Crossref] [PubMed]
- Arias S, Lee HJ. The future of interventional pulmonology. Semin Respir Crit Care Med 2014;35:763-8. [Crossref] [PubMed]
- Semler MW, Keriwala RD, Clune JK, et al. A randomized trial comparing didactics, demonstration, and simulation for teaching teamwork to medical residents. Ann Am Thorac Soc 2015;12:512-9. [Crossref] [PubMed]
- Lee Chang A, Dym AA, Venegas-Borsellino C, et al. Comparison between Simulation-based Training and Lecture-based Education in Teaching Situation Awareness. A Randomized Controlled Study. Ann Am Thorac Soc 2017;14:529-35. [Crossref] [PubMed]
- Ramar K, De Moraes AG, Selim B, et al. Effectiveness of hands-on tutoring and guided self-directed learning versus self-directed learning alone to educate critical care fellows on mechanical ventilation - a pilot project. Med Educ Online 2016;21:32727. [Crossref] [PubMed]
- Huang GC, McSparron JI, Balk EM, et al. Procedural instruction in invasive bedside procedures: a systematic review and meta-analysis of effective teaching approaches. BMJ Qual Saf 2016;25:281-94. [Crossref] [PubMed]
- American Board of Internal Medicine. Policies and Procedures for Certification. Philadelphia, PA: ABIM, 2006.
- McSparron JI, Michaud GC, Gordan PL, et al. Simulation for Skills-based Education in Pulmonary and Critical Care Medicine. Ann Am Thorac Soc 2015;12:579-86. [Crossref] [PubMed]
- Stather DR, MacEachern P, Chee A, et al. Trainee impact on procedural complications: an analysis of 967 consecutive flexible bronchoscopy procedures in an interventional pulmonology practice. Respiration 2013;85:422-8. [Crossref] [PubMed]
- Nayahangan LJ, Clementsen PF, Paltved C, et al. Identifying Technical Procedures in Pulmonary Medicine That Should Be Integrated in a Simulation-Based Curriculum: A National General Needs Assessment. Respiration 2016;91:517-22. [Crossref] [PubMed]
- Kurup V, Matei V, Ray J. Role of in-situ simulation for training in healthcare: opportunities and challenges. Curr Opin Anaesthesiol 2017;30:755-60. [Crossref] [PubMed]
- Dine CJ, Gersh RE, Leary M, et al. Improving cardiopulmonary resuscitation quality and resuscitation training by combining audiovisual feedback and debriefing. Crit Care Med 2008;36:2817-22. [Crossref] [PubMed]
- Kennedy CC, Maldonado F, Cook DA. Simulation-based bronchoscopy training: systematic review and meta-analysis. Chest 2013;144:183-92. [Crossref] [PubMed]
- Pastis NJ, Vanderbilt AA, Tanner NT, et al. Construct validity of the Simbionix bronch mentor simulator for essential bronchoscopic skills. J Bronchology Interv Pulmonol 2014;21:314-21. [Crossref] [PubMed]
- Colt HG, Crawford SW, Galbraith O 3rd. Virtual reality bronchoscopy simulation: a revolution in procedural training. Chest 2001;120:1333-9. [Crossref] [PubMed]
- Crawford SW, Colt HG. Virtual reality and written assessments are of potential value to determine knowledge and skill in flexible bronchoscopy. Respiration 2004;71:269-75. [Crossref] [PubMed]
- Sehgal IS, Dhooria S, Aggarwal AN, et al. Training and proficiency in endobronchial ultrasound-guided transbronchial needle aspiration: A systematic review. Respirology 2017;22:1547-57. [Crossref] [PubMed]
- Stather DR, MacEachern P, Chee A, et al. Evaluation of clinical endobronchial ultrasound skills following clinical versus simulation training. Respirology 2012;17:291-9. [Crossref] [PubMed]
- Stather DR, Maceachern P, Rimmer K, et al. Assessment and learning curve evaluation of endobronchial ultrasound skills following simulation and clinical training. Respirology 2011;16:698-704. [Crossref] [PubMed]
- Unroe MA, Shofer SL, Wahidi MM. Training for endobronchial ultrasound: methods for proper training in new bronchoscopic techniques. Curr Opin Pulm Med 2010;16:295-300. [Crossref] [PubMed]
- Iwasaki A, Moriyama S, Shirakusa T. New trainer for video-assisted thoracic surgery lobectomy. Thorac Cardiovasc Surg 2008;56:32-6. [Crossref] [PubMed]
- Mavroudis CD, Mavroudis C, Jacobs JP, et al. Simulation and Deliberate Practice in a Porcine Model for Congenital Heart Surgery Training. Ann Thorac Surg 2018;105:637-43. [Crossref] [PubMed]
- Ritter EM, Taylor ZA, Wolf KR, et al. Simulation-based mastery learning for endoscopy using the endoscopy training system: a strategy to improve endoscopic skills and prepare for the fundamentals of endoscopic surgery (FES) manual skills exam. Surg Endosc 2018;32:413-20. [Crossref] [PubMed]
- Beyer-Berjot L, Pucher P, Patel V, et al. Colorectal surgery and enhanced recovery: Impact of a simulation-based care pathway training curriculum. J Visc Surg 2017;154:313-20. [Crossref] [PubMed]
- Clarke DB, Kureshi N, Hong M, et al. Simulation-based training for burr hole surgery instrument recognition. BMC Med Educ 2016;16:153. [Crossref] [PubMed]
- Zakhary BM, Kam LM, Kaufman BS, et al. The Utility of High-Fidelity Simulation for Training Critical Care Fellows in the Management of Extracorporeal Membrane Oxygenation Emergencies: A Randomized Controlled Trial. Crit Care Med 2017;45:1367-73. [Crossref] [PubMed]
- Vergmann AS, Vestergaard AH, Grauslund J. Virtual vitreoretinal surgery: validation of a training programme. Acta Ophthalmol 2017;95:60-5. [Crossref] [PubMed]
- Staropoli PC, Gregori NZ, Junk AK, et al. Surgical Simulation Training Reduces Intraoperative Cataract Surgery Complications Among Residents. Simul Healthc 2018;13:11-5. [PubMed]
- Patel R, Dennick R. Simulation based teaching in interventional radiology training: is it effective? Clin Radiol 2017;72:266.e7-e14. [Crossref] [PubMed]
- Mosier JM, Malo J, Sakles JC, et al. The impact of a comprehensive airway management training program for pulmonary and critical care medicine fellows. A three-year experience. Ann Am Thorac Soc 2015;12:539-48. [Crossref] [PubMed]
- Gause CD, Hsiung G, Schwab B, et al. Advances in Pediatric Surgical Education: A Critical Appraisal of Two Consecutive Minimally Invasive Pediatric Surgery Training Courses. J Laparoendosc Adv Surg Tech A 2016;26:663-70. [Crossref] [PubMed]
- Agarwal A, Marks N, Wessel V, et al. Improving knowledge, technical skills, and confidence among pediatric health care providers in the management of chronic tracheostomy using a simulation model. Pediatr Pulmonol 2016;51:696-704. [Crossref] [PubMed]
- Kennedy CC, Cannon EK, Warner DO, et al. Advanced airway management simulation training in medical education: a systematic review and meta-analysis. Crit Care Med 2014;42:169-78. [Crossref] [PubMed]
- Kory PD, Eisen LA, Adachi M, et al. Initial airway management skills of senior residents: simulation training compared with traditional training. Chest 2007;132:1927-31. [Crossref] [PubMed]
- Rosenthal ME, Adachi M, Ribaudo V, et al. Achieving housestaff competence in emergency airway management using scenario based simulation training: comparison of attending vs housestaff trainers. Chest 2006;129:1453-8. [Crossref] [PubMed]
- Bohnen JD, Demetri L, Fuentes E, et al. High-Fidelity Emergency Department Thoracotomy Simulator With Beating-Heart Technology and OSATS Tool Improves Trainee Confidence and Distinguishes Level of Skill. J Surg Educ 2018;75:1357-66. [Crossref] [PubMed]
- Barsuk JH, Cohen ER, Williams MV, et al. Simulation-Based Mastery Learning for Thoracentesis Skills Improves Patient Outcomes: A Randomized Trial. Acad Med 2018;93:729-35. [Crossref] [PubMed]
- Alsaad AA, Bhide VY, Moss JL Jr, et al. Central Line Proficiency Test Outcomes after Simulation Training versus Traditional Training to Competence. Ann Am Thorac Soc 2017;14:550-4. [Crossref] [PubMed]
- Peltan ID, Shiga T, Gordon JA, et al. Simulation Improves Procedural Protocol Adherence During Central Venous Catheter Placement: A Randomized Controlled Trial. Simul Healthc 2015;10:270-6. [Crossref] [PubMed]
- Hoskote SS, Khouli H, Lanoix R, et al. Simulation-based training for emergency medicine residents in sterile technique during central venous catheterization: impact on performance, policy, and outcomes. Acad Emerg Med 2015;22:81-7. [Crossref] [PubMed]
- Laack TA, Dong Y, Goyal DG, et al. Short-term and long-term impact of the central line workshop on resident clinical performance during simulated central line placement. Simul Healthc 2014;9:228-33. [Crossref] [PubMed]
- Auffermann WF, Henry TS, Little BP, et al. Simulation for Teaching and Assessment of Nodule Perception on Chest Radiography in Nonradiology Health Care Trainees. J Am Coll Radiol 2015;12:1215-22. [Crossref] [PubMed]
- Yeh DH, Fung K, Malekzadeh S. Boot Camps: Preparing for Residency. Otolaryngol Clin North Am 2017;50:1003-13. [Crossref] [PubMed]
- Miller RJ, Mudambi L, Vial MR, et al. Evaluation of Appropriate Mediastinal Staging among Endobronchial Ultrasound Bronchoscopists. Ann Am Thorac Soc 2017;14:1162-8. [PubMed]
- Sihoe ADL, Gonzalez-Rivas D, Yang TY, et al. High-volume intensive training course: a new paradigm for video-assisted thoracoscopic surgery education. Interact Cardiovasc Thorac Surg 2018;27:365-71. [Crossref] [PubMed]
- Rowse PG, Dearani JA. Deliberate Practice and the Emerging Roles of Simulation in Thoracic Surgery. Thorac Surg Clin 2019;29:303-9. [Crossref] [PubMed]
- Wang JM, Zorek JA. Deliberate Practice as a Theoretical Framework for Interprofessional Experiential Education. Front Pharmacol 2016;7:188. [Crossref] [PubMed]
- Hastings RH, Rickard TC. Deliberate practice for achieving and maintaining expertise in anesthesiology. Anesth Analg 2015;120:449-59. [Crossref] [PubMed]
- Helsen WF, Hodges NJ, Van Winckel J, et al. The roles of talent, physical precocity and practice in the development of soccer expertise. J Sports Sci 2000;18:727-36. [Crossref] [PubMed]
- Ericsson KA, Harwell KW. Deliberate Practice and Proposed Limits on the Effects of Practice on the Acquisition of Expert Performance: Why the Original Definition Matters and Recommendations for Future Research. Front Psychol 2019;10:2396. [Crossref] [PubMed]
- Ericsson KA. Deliberate practice and acquisition of expert performance: a general overview. Acad Emerg Med 2008;15:988-94. [Crossref] [PubMed]
- Spruit EN, Band GP, Hamming JF. Increasing efficiency of surgical training: effects of spacing practice on skill acquisition and retention in laparoscopy training. Surg Endosc 2015;29:2235-43. [Crossref] [PubMed]
- Achurra P, Lagos A, Avila R, et al. Allowing New Opportunities in Advanced Laparoscopy Training Using a Full High-Definition Training Box. Surg Innov 2017;24:66-71. [Crossref] [PubMed]
- Van Cleynenbreugel BSEP, Gözen AS, Tokas T. The value of simulation-based training in the path to laparoscopic urological proficiency. Curr Opin Urol 2017;27:337-41. [Crossref] [PubMed]
- Boza C, León F, Buckel E, et al. Simulation-trained junior residents perform better than general surgeons on advanced laparoscopic cases. Surg Endosc 2017;31:135-41. [Crossref] [PubMed]
- Jones GF, Forsyth K, Jenewein CG, et al. Research Residents' perceptions of skill decay: Effects of repeated skills assessments and scenario difficulty. Am J Surg 2017;213:631-6. [Crossref] [PubMed]
- Perez RS, Skinner A, Weyhrauch P, et al. Prevention of surgical skill decay. Mil Med 2013;178:76-86. [Crossref] [PubMed]
- Stather DR, Chee A, MacEachern P, et al. Endobronchial ultrasound learning curve in interventional pulmonary fellows. Respirology 2015;20:333-9. [Crossref] [PubMed]
- Ernst A, Wahidi MM, Read CA, et al. Adult Bronchoscopy Training: Current State and Suggestions for the Future: CHEST Expert Panel Report. Chest 2015;148:321-32. [Crossref] [PubMed]
- Bellinger CR, Chatterjee AB, Adair N, et al. Training in and experience with endobronchial ultrasound. Respiration 2014;88:478-83. [Crossref] [PubMed]
- Medford AR. Learning Curve for EBUS-TBNA: Longer than We May Think. Respiration 2015;90:173. [Crossref] [PubMed]
- Lee HJ, Lerner AD, Coleman B, et al. Learning Electromagnetic Navigational Bronchoscopy and Percutaneous Transthoracic Needle Biopsy (LEAP): A Pilot Study. J Bronchology Interv Pulmonol 2019;26:55-61. [Crossref] [PubMed]
- Wahidi MM, Hulett C, Pastis N, et al. Learning experience of linear endobronchial ultrasound among pulmonary trainees. Chest 2014;145:574-8. [Crossref] [PubMed]
- Mahmood K, Wahidi MM, Osann KE, et al. Development of a Tool to Assess Basic Competency in the Performance of Rigid Bronchoscopy. Ann Am Thorac Soc 2016;13:502-11. [PubMed]
- Davoudi M, Colt HG, Osann KE, et al. Endobronchial ultrasound skills and tasks assessment tool: assessing the validity evidence for a test of endobronchial ultrasound-guided transbronchial needle aspiration operator skill. Am J Respir Crit Care Med 2012;186:773-9. [Crossref] [PubMed]
- Scarlata S, Palermo P, Candoli P, et al. EBUS-STAT Subscore Analysis to Predict the Efficacy and Assess the Validity of Virtual Reality Simulation for EBUS-TBNA Training Among Experienced Bronchoscopists. J Bronchology Interv Pulmonol 2017;24:110-6. [Crossref] [PubMed]
- Konge L, Clementsen PF, Ringsted C, et al. Simulator training for endobronchial ultrasound: a randomised controlled trial. Eur Respir J 2015;46:1140-9. [Crossref] [PubMed]
- Davoudi M, Osann K, Colt HG. Validation of two instruments to assess technical bronchoscopic skill using virtual reality simulation. Respiration 2008;76:92-101. [Crossref] [PubMed]
- Voduc N, Dudek N, Parker CM, et al. Development and Validation of a Bronchoscopy Competence Assessment Tool in a Clinical Setting. Ann Am Thorac Soc 2016;13:495-501. [PubMed]
- Salamonsen MR, Bashirzadeh F, Ritchie AJ, et al. A new instrument to assess physician skill at chest tube insertion: the TUBE-iCOMPT. Thorax 2015;70:186-8. [Crossref] [PubMed]
- Lamb CR, Feller-Kopman D, Ernst A, et al. An approach to interventional pulmonary fellowship training. Chest 2010;137:195-9. [Crossref] [PubMed]
- Fielding D, Phillips M, Robinson P, et al. Advanced interventional pulmonology procedures: training guidelines from the Thoracic Society of Australia and New Zealand. Respirology 2012;17:1176-89. [Crossref] [PubMed]
- Corbetta L, Arru LB, Mereu C, et al. Competence and training in interventional pulmonology. Panminerva Med 2019;61:203-31. [PubMed]
- Corbetta L. Training to competence in interventional pulmonology. Panminerva Med 2019;61:201-2. [PubMed]
- Feller-Kopman D, Yarmus L. Training in interventional pulmonology. Semin Respir Crit Care Med 2014;35:631-5. [Crossref] [PubMed]
- Courtright KR, Weinberger SE, Wagner J. Meeting the milestones. Strategies for including high-value care education in pulmonary and critical care fellowship training. Ann Am Thorac Soc 2015;12:574-8. [Crossref] [PubMed]
- Winder JS, Juza RM, Sasaki J, et al. Implementing a robotics curriculum at an academic general surgery training program: our initial experience. J Robot Surg 2016;10:209-13. [Crossref] [PubMed]
- Chan PG, Schaheen LW, Chan EG, et al. Technology-Enhanced Simulation Improves Trainee Readiness Transitioning to Cardiothoracic Training. J Surg Educ 2018;75:1395-402. [Crossref] [PubMed]
- Maertens H, Aggarwal R, Desender L, et al. Development of a PROficiency-Based StePwise Endovascular Curricular Training (PROSPECT) Program. J Surg Educ 2016;73:51-60. [Crossref] [PubMed]
- Angelo RL, Ryu RK, Pedowitz RA, et al. A Proficiency-Based Progression Training Curriculum Coupled With a Model Simulator Results in the Acquisition of a Superior Arthroscopic Bankart Skill Set. Arthroscopy 2015;31:1854-71. [Crossref] [PubMed]
- Mullon JJ, Burkart KM, Silvestri G, et al. Interventional Pulmonology Fellowship Accreditation Standards: Executive Summary of the Multisociety Interventional Pulmonology Fellowship Accreditation Committee. Chest 2017;151:1114-21. [Crossref] [PubMed]
- Wahidi MM. Interventional Pulmonology: Marching Forward Together. J Bronchology Interv Pulmonol 2016;23:87-8. [Crossref] [PubMed]
- Lee HJ, Mullon JJ. Accredited Interventional Pulmonary Fellowships: The Time is Here. J Bronchology Interv Pulmonol 2015;22:189-90. [Crossref] [PubMed]
- Lee HJ, Feller-Kopman D, Shepherd RW, et al. Validation of an interventional pulmonary examination. Chest 2013;143:1667-70. [Crossref] [PubMed]
- Kempainen RR, Hess BJ, Addrizzo-Harris DJ, et al. Pulmonary and Critical Care In-Service Training Examination Score as a Predictor of Board Certification Examination Performance. Ann Am Thorac Soc 2016;13:481-8. [PubMed]
- Semaan RW, Hazbon MP, Arias SA, et al. Academic Productivity of Interventional Pulmonology Training Programs. Ann Am Thorac Soc 2016;13:536-9. [PubMed]
- Ramar K, Vassallo R, Nelson DR, et al. Innovative intervention to improve fellows' research training. Med Educ 2015;49:1159. [Crossref] [PubMed]
- Mireles-Cabodevila E, Stoller JK. Research during fellowship: ten commandments. Chest. 2009;135:1395-9. [Crossref] [PubMed]
- Weinert CR, Billings J, Ryan R, et al. Academic and career development of pulmonary and critical care physician-scientists. Am J Respir Crit Care Med 2006;173:23-31. [Crossref] [PubMed]
- Ericsson KA. Training history, deliberate practice and elite sports performance: an analysis in response to Tucker and Collins review--what makes champions? Br J Sports Med 2013;47:533-5. [Crossref] [PubMed]