
Autoimmune disorders and paraneoplastic syndromes in thymoma
Introduction
The current 4th edition of the WHO Classification of tumours of the thymus from 2015 distinguishes thymomas, thymic carcinoma, and thymic neuroendocrine tumours as essential thymic epithelial tumours (TET) originating within this mediastinal organ that is of particular relevance for the development of human adaptive immune response (1). Although these three TETs represent rare tumour entities, empirical clinical knowledge has long-since prompted a causal link between thymoma and autoimmune disorders (AIDs) as well as paraneoplastic syndromes (PNS), likewise, but to a lesser extent in the other two thymic tumour entities. First autoimmune and paraneoplastic phenomena were already described in cancer by Auche in 1890 (2) as well as specifically related to a thymic tumour by Weigert in 1901 (3) which were succeeded by a growing body of case reports and case series depicting a whole spectrum of AID and PNS including their clinical impact in thymic neoplasia. Yet, it took more than a century before the recently published analysis of the world’s largest database of the International Thymic Malignancy Interest Group (ITMIG) could substantiate their frequencies on a more reliable evidence basis (4). In parallel, basic research has increasingly revealed underlying pathophysiological mechanisms over the last decades, namely due to more sophisticated moleculargenetic techniques, leading to a much clearer, though still incomplete understanding of the complex nature of AID and PNS in TETs (5).
This invited review article as part of the special issue on ‘Thymoma’ provides a thorough overview on the variety of AID and PNS in thymomas considering common features as well as portraying their distinct pathophysiological, clinical, therapeutic, and prognostic aspects.
General pathogenesis of AID and PNS in thymic tumours
There are no generally consented definitions of AID and PNS. The British Society for Immunology referred to AID as ‘Autoimmunity involves a misdirection of the body’s immune system against its own tissues, causing a large number of diseases. Some affect only one tissue or organ, while others are systemic’ (6). In their book on PNS, Darnell and Posner labelled them as ‘disorders caused by cancer, but not by a direct result of cancer invasion of the affected tissue or organ’ (7). As Girard pointed out in his editorial on the retrospective analysis of the large ITMIG dataset, the practical distinction between AID and PNS in thymic malignancies is still challenging, nonetheless, due to substantial differences in their clinical effects, courses and outcomes, a clearer separation of both should be sought prospectively (8).
Physiologically, thymopoiesis, the maturation and differentiation from bone marrow-derived haematopoietic precursor cells to T cells, forms a complex process with the thymus as an essential place of maturation. In the thymic cortex, a so-called positive selection limits the survival of the immigrated immature precursors (thymocytes) to only those with a functioning T cell receptor. Hereafter, a negative selection in the thymic medulla, triggered by medullary thymic epithelial cells, leads to the elimination of those T cells which have developed specific receptors primed against tissue-specific self-antigens. The latter step is critical in the genuine prevention of autoimmunity. The success of this maturation sequence is considerably depending on two factors, first the expression of specific genes [i.e., autoimmune regulator (AIRE) gene, major histocompatibility (MHC) class II] and the presence of certain transcription factors (i.e., forebrain-expressed zinc finger 2) as well as second on an intact architecture of the internal thymic structure. In addition, AIRE is involved in the normal composition of regulatory T cells which bear an immunosuppressive function attenuating potential autoimmune reactions (9).
As reviewed more in-depth elsewhere, the understanding of the pathophysiology in thymoma leading to AID has well-advanced over the last decades. Contributing factors to the emergence of autoimmunity in thymoma patients include deprived or even lacking expression levels of AIRE and MHC class II, and as a consequence diminished immune tolerance as well as a reduced number of regulatory T cells. Equally, evidence underlines that the disorder of the thymic architecture through the formation and expansion of thymoma cell clones results in the promotion of AID for which separate mechanisms have been postulated. Owing to the perturbance of the normal thymic microenvironment, immature autoreactive T cells may bypass thymic medulla elimination and slip through into systemic circulation, similarly, uncontrolled accelerated proliferation of autoreactive thymoma clones may outreach the originary limiting positive selection in the thymic cortex, both of which have been termed as escape and genetic hypotheses, respectively. The occurrence of neo-antigens in the form of muscle, parathyroid or other adjacent components as well as cytokines and interferons elicited by disrupted thymic structures have been shown to implicate autoreactive T cell behaviour as well. Noteworthy, the release of dysfunctional T cells from the thymus may in addition go along with immune-incompetence prone to provoke serious infections as well as the genesis of secondary malignancies (5,9,10). Finally, recent scientific advances aim to generate genetic profiles of thymomas and other thymic epithelial tumours, not only to set the basis for more precise future classification systems of thymic tumours exceeding current histopathologically driven groupings, but also to deepen the knowledge of autoimmunity mechanisms in thymic tumours (11,12).
While the prerequisites for AID in thymoma originate centrally in the thymus mainly through the alteration of normal naïve T cells towards systemically effective autoreactive behaviour, the underlying elicitors for PNS in thymoma are triggered by the thymoma cells themselves. It is evident that thymoma can release endocrine or paracrine messengers, be it peptides, cytokines, or hormones, all of them capable to induce a variety of clinically relevant systemic effects. At the same time, the presence of thymoma cells or specific constituent elements of them inhere an antigenic potential that can constantly drive the creation of autoantibodies as signs of cross-reactions with equivalent antigenic organ or tissue structures remotely from the tumour (13).
General epidemiological and clinical aspects of AID and PNS in thymic tumours
Reported frequencies of AID and PNS in thymoma vary in the literature. The retrospective exploration of the by far largest ITMIG database by Padda et al. encompassed 6,670 patients diagnosed between 1951 and 2012 with thymomas, thymic carcinoma and neuroendocrine thymic tumours in 86%, 12% and 2%, respectively. Type AB and B2 thymomas were the most prominent histological subtypes in the thymoma cohort. AID and PNS were declared by the 56 contributing institutions in 38.8% of the thymoma patients, while significantly less common in both thymic carcinomas and neuroendocrine thymic tumours with respective 5.8% and 3.6%. In the entire cohort, myasthenia gravis was the most prominent AID/PNS with 34.0%. Pure red cell aplasia, hypogammaglobulinemia as well as a mixture of other AID/PNS accounted for less than 1% each of all cases (4).
The retrospective thymic database of the European Society of Thoracic Surgeons (ESTS) collecting data from 2,030 eligible patients in 35 institutions during 1999–2010 proved similar proportions of thymic cancers (9%) and neuroendocrine thymic tumours (2%) as well as of myasthenia gravis in all patients (35%) (14). A separate analysis of this ESTS database exclusively in the 215 thymic carcinoma patients depicted a myasthenia gravis rate of 14% (15).
A retrospective observational study in six Italian centres collated 797 thymoma-only cases with a consecutively higher rate of myasthenia gravis occurrence of 47% (16).
In contrast, three large Asian studies built upon retrospective databases, one by the Japanese Association for Research on the Thymus (JART) on thymic tumours (2,638 patients; 32 institutions; 1991–2010; thymic carcinomas in 12%) and another two on thymoma only [(I) Chinese Alliance for Research in Thymomas (ChART) registry; 1,850 patients; 18 centres; 1992–2012; (II) Japan; 1,089 patients; 115 centres; 1990–1994], depicted substantially lower myasthenia gravis rates of 23%, 22.7% and 24.8%, respectively (17-19). Yet, the worldwide ITMIG database could verify these differences of myasthenia gravis proportions across continents in a respective subgroup analysis (Europe: 49%, Asia: 26%, North America: 27%) prompting distinct genetic backgrounds as a causative factor for these findings (4).
Bernard et al. published a smaller case series of 85 thymoma patients treated in 3 French centres between 2005 and 2011 out of whom 47 (55%) had one or more AID or PNS. AID/PNS diagnoses were preceding, concomitant to or succeeding the thymoma diagnosis in 68%, 19% and 15%, respectively. Generally, AID/PND were documented more frequently than in the ITMIG cohort with myasthenia gravis in 39% and a higher number of different manifestations (n=14) constituting 1–5% each within the entire cohort (20).
In their review, Marx et al. provided frequencies of an extensive list of proven or presumed AID and PNS in thymoma, obviously based on published case reports and case series. Comparably, they quantified the co-incidence of thymoma and myasthenia gravis with 30–44%. While the proportions in the majority of the other named AID/PNS again ranged between less than 1% up to 5%, higher rates were reported for hypogammaglobulinemia and alopecia areata in 5–20% and 0.5–17%, respectively (21).
Regarding clinical features, Padda et al. could demonstrate in their large ITMIG patient population statistically significant associations of AID/PNS presence with younger median age, female gender, B2 thymoma (mostly due to the predominance of myasthenia gravis in this subtype) and more favourable stages. These findings are in concordance with the other above mentioned larger retrospective databases from Europe and Asia (14,16-19).
Remarkably, the more recent and prospective thymic database of the European Society of Thoracic Surgeons which enrolled 1,122 patients from 75 ESTS institutions showed higher proportions of thymic carcinoma (28%) and neuroendocrine thymic tumours (7%) at the expense of a lower thymoma rate (65%) contrasting distributions in the named retrospective databases. Albeit this seems mostly due to advanced classification systems and thereby more accurate histological grouping of thymic tumours over time (1), one should keep in mind that such a significant shift needs to be accounted for when comparing historical and future data of this kind (22).
General Management of thymoma as well as related AID and PNS
During the clinical work-up of newly diagnosed thymoma patients as well as during the entire course of their disease, full attention should be paid to symptoms and signs of AID or PNS ensuring thorough history and complete clinical examination. Relapse of thymoma and/or AID/PNS as well as occurrence of new AID/PNS may emerge any time throughout the entire disease continuum. Thymoma patients should be informed accordingly by their treating physicians. Likewise, thymic tumour disease should always be taken into consideration if potential AID or PNS are suspected without so far recognizable or a history of former malignancies. Guidelines regarding screening for tumours in paraneoplastic syndromes as well as diagnostic and therapeutical guidance for neurological PNS were published by the European Federation of Neurological Societies (EFNS), the Paraneoplastic Neurological Syndrome Euronetwork and the Myasthenia Gravis Foundation of America. Amongst other topics, immunological diagnostics including AID/PNS-related autoantibody-profiles have been addressed comprehensively (23-26). The management of thymoma and thymic carcinoma is covered in the guideline issued by the European Society for Medical Oncology from 2015 (27) and more recently in the statement by the Italian collaborative group for ThYmic MalignanciEs (TYME) (28) as well as the guideline of the National Comprehensive Cancer Network (29). Specific recommendations on the management of AID and PNS are missing in all 3 worthwhile documents. However, all 3 recommend, based on a multidisciplinary decision finding, upfront thymectomy in resectable thymomas (Masaoka stage I–III, TNM stage I–IIIA) as well as to consider a multimodal approach with neoadjuvant chemotherapy followed by surgery and radiotherapy in locally advanced, unresectable thymomas (Masaoka stage III–IVA, TNM stage IIIA–IVA). This is in line with the three pillars of the general treatment strategy to tackle AID and PNS in which the first pillar aims on effective tumour-specific treatment targeted against the primary tumour and potential metastases of the causative malignancy. The second and third pillar consist of immunosuppressive and/or immunomodulating therapies as well as treatment measures to antagonize potentially hazardous signs or symptoms of AID/PNS.
Specific manifestations of AID and PNS in thymoma, related findings, diagnostic and therapeutic aspects
AID and PNS in thymoma have been described in numerous organs and tissues within the human body. Since thymoma are counted among the orphan diseases and their specific AID/PNS manifestations mostly occur rarely, the underlying treasure of empirical knowledge has been mainly built upon epoch-spanning publications of case reports and smaller case series as well as by implication limited translational research options.
Recently, Zhao et al. performed a systematic review of case reports and case series on PNS with thymoma-association. They detected 507 initially operated patients with 123 different PNS. Myasthenia gravis was present in 302 of all reported patients (63%). The next most common PNS among all collated cases were pure red cell aplasia (39 patients; 7.7%), lichen planus (32 patients; 6.3%), Good syndrome and limbic encephalitis (both: 30 patients; 5.9%). 49% of all thymoma cases featured 2 or more PNS. The detection of PNS succeeded surgical resection in 20% of cases (30).
On the contrary, larger multicentric databases which were commonly retrospective in nature provided frequently solely general information on thymic tumours. As a result, the overall quality of the evidence is for the most part low.
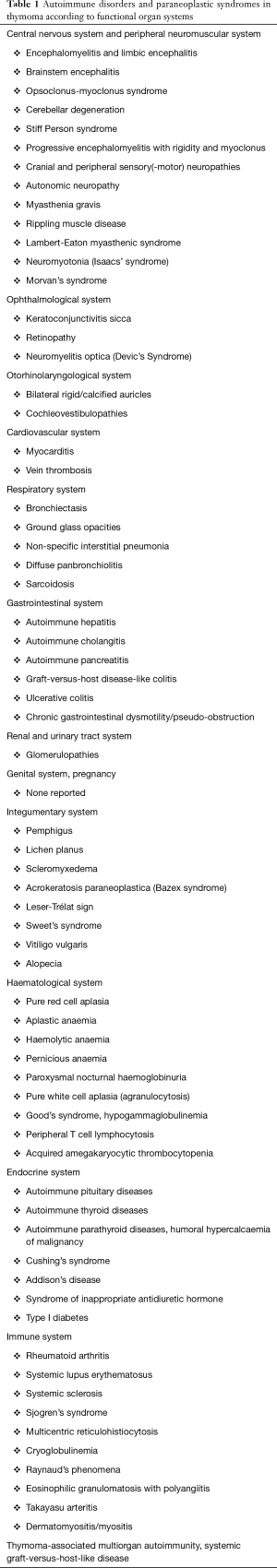
In the subsequent subsections, this review article offers a broad overview on the specific AID/PNS manifestations in thymoma and highlights related findings as well as relevant diagnostic and therapeutic aspects. It would be far beyond the scope of this work to reference pieces of evidence to their full extent for all AID and PNS, instead focussed reviews of good quality are referred to whenever available for the various manifestations, otherwise exemplary case reports are cited. Table 1 summarizes the AID/PNS in thymoma according to functional organ systems.
Full table
Central nervous system and peripheral neuromuscular system
Most segments alongside the entire neural axis from the cerebral cortex to the neuromuscular junctions may be affected by AID and PNS as thoroughly reviewed by Lancaster (31). Already in 2004, the Paraneoplastic Neurological Syndrome Euronetwork formulated sophisticated diagnostic criteria for paraneoplastic neurological syndromes. Their diagnostic decision-algorithm discriminates between (I) classical/non-classical syndromes, (II) tumour presence/absence, and (III) presence/absence of onconeural antibodies resulting in a definite or a possible diagnosis. The authors named as classical neurological syndromes encephalomyelitis, limbic encephalitis, subacute cerebellar degeneration, opsoclonus-myoclonus, subacute sensory neuronopathy, Lambert-Eaton myasthenic syndrome (LEMS), chronic gastro-intestinal pseudo-obstruction, and dermatomyositis (in this present review, the latter two are covered in the respective subsections for the gastrointestinal and immune system) (24). In 2010, the Paraneoplastic Neurological Syndrome Euronetwork published their findings derived from a pan-European multi-centric (n=20), prospective data collection on paraneoplastic neurological syndromes during 2000–2008. In total, 979 patients were enrolled. Cerebellar degeneration and sensory neuronopathy were the two syndromes most detected and representing 24.3% each of all patients, followed by limbic encephalitis with 10%. Thymoma ranked 7th with 2.7% of cases within the entire cohort, nominally led by far by small cell lung cancer as most frequent underlying tumour type with 38.2%. Yet, beside the different general incidence rates of both tumours, it is worth noting that myasthenia gravis was excluded in this data collection. Death was recorded in 403 patients (41%) which was due to progressive tumour and the paraneoplastic syndrome in 37% and 27%, respectively (36% other/unknown causes of death). Notably, dysautonomia signalled a very poor prognosis as 32 of the 51 included patients died (63%) (32).
Encephalomyelitis and limbic encephalitis
Encephalomyelitis in thymoma is triggered by anti-Hu (ANNA-1)- and anti-Ma2-antibodies in most cases, both directed against neuronal antigens. Signs and symptoms vary according to the cerebral structures affected with commonly subacute onsets. In addition, involvement of peripheral nerves or the myenteric plexus can be another clinical feature of encephalomyelitis.
The involvement of the limbic system in limbic encephalitis may provoke cognitive as well as neuro-psychiatric impairments. Immunosuppressive agents are therapy of first choice, yet refractory or residual courses are common in which plasmapheresis or intravenous immunoglobulins may be used. The same therapeutic approaches apply to brainstem encephalitis, opsoclonus-myoclonus syndrome and cerebellar degeneration which are covered subsequently (33).
Brainstem encephalitis
Anti-Ri (ANNA-2)- and anti-Ma2-antibodies are most prevalent in brainstem encephalitis. Findings could be life-threatening when respiratory or other regulatory vital centres in the brainstem are affected (34).
Opsoclonus-myoclonus syndrome
Opsoclonus-myoclonus syndrome is characterized by a combination of high-frequent eye oscillations, involuntary movements of limb and/or trunk muscles and ataxia, but patients may also present with ancillary behavioural and cognitive disturbances, vertigo and sleep disorders. Paraneoplastic opsoclonus-myoclonus syndrome has been linked with a variety of onconeural antibodies such as anti-Ri (ANNA-2), anti-Hu (ANNA-1, anti-Yo (PCA-1), anti-Ma1 and anti-Ma2 (35).
Cerebellar degeneration
Cerebellar degeneration shows often an anti-Yo (PCA-1)- or anti-Hu (ANNA-1)-antibody-profile going along with progressing cerebellar signs (i.e., nystagmus, diplopia, vertigo, dysarthria, ataxia) (36).
Stiff person syndrome
Stiff person syndrome is associated with several autoimmune diseases (type 1 diabetes, chronic atrophic gastritis, autoimmune thyroiditis) as well as tumours such as thymomas.
Anti-glutaminic acid decarboxylase (GAD) antibodies are most commonly detected, to a lesser extent anti-glycin receptor-, anti-amphiphysin- or anti-DPPX-antibodies. All of these target inhibitory central nervous synapses which could well explain the symptom load including symmetric muscular immobility accentuated in trunk and pelvis regions as well as shooting pain attacks causing sudden falls. Therapeutic measures include benzodiazepines or baclofen as antispasmodics, further immunosuppression/-modulation via prednisolone, intravenous immunoglobulins and plasmapheresis (37).
Progressive encephalomyelitis with rigidity and myoclonus
Progressive encephalomyelitis with rigidity and myoclonus (PERM) resembles stiff person syndrome with the addition of augmented startle responses (38).
Cranial and peripheral sensory(-motor) neuropathies
In thymoma, paraneoplastic sensory or sensory-motor neuropathies in cranial and peripheral nerves are often related to anti-CRMP-5- or anti-Hu (ANNA-1)-antibodies, yet, also seronegative cases are frequently encountered (39,40).
In their case series, Xu et al. refer to 7 patients with paraneoplastic optic neuropathy of whom 1 patient had type B thymoma. Clinical findings and courses varied among patients. Mean time from diagnosis of tumour to first symptoms of optic neuropathy was 18.5 months (range, 1–36 months). Despite immunosuppressive treatment, outcomes were mostly unfavourable with persisting significant impairment in 69% of all affected eyes (41).
Paraneoplastic cochleovestibulopathies present with sudden to subacute bilateral sensorineural hearing loss which may be accompanied by vertigo as symptom of vestibular dysfunction (42). A retrospective observational study in a patient cohort with bilateral hearing loss from Central Illinois, USA revealed paraneoplastic origin in 3 out of 57 cases in the time period 2007–2017 (43).
In peripheral neuropathies, neuropathic side-effects under systemic chemotherapies affecting peripheral nerves should be considered as a differential diagnosis, correspondingly rare brain or skull metastasis in optic neuropathies or cochleovestibulopathies. Again, specific treatment options aim at immunosuppression as well as immunomodulation, unfortunately, in many instances with only limited or no benefit. Nonetheless, findings in paraneoplastic sensory/sensory-motor neuropathies may be alleviated with thymoma-directed therapies as well (39-42).
Autonomic neuropathy
Anti-acetylcholine receptor (AChR)- and anti-Contactin Response Mediator Protein 5 (CRMP-5)-antibodies binding in autonomic ganglia may affect the autonomic nervous system resulting in downstream vegetative signs and symptoms, both sympathetic and/or parasympathetic. In their case series of 7 patients, Vernino et al. reported the detection of specific neuronal AChR-antibodies in the 3 thymoma patients as well as symptom relief following acetylcholinesterase inhibitor medication (44).
Myasthenia gravis
According to the recent review by Marx et al., up to 40% of thymoma patients develop thymoma-associated myasthenia gravis (TAMG), while in all myasthenia gravis cases, thymoma frequencies account for 10–20%. Other thymic conditions such as thymic follicular hyperplasia or thymic atrophy are related to early-onset myasthenia gravis (EOMG) and late-onset myasthenia gravis (LOMG) contributing to 30% and 40% in all myasthenia gravis patients, respectively. While anti-AChR-antibodies are most prevalent in thymoma-associated as well as non-thymomatous myasthenia gravis, in rare instances anti-MuSK-, anti-LRP4-, anti-Agrin-antibodies and still seronegative findings have become evident in thymic myasthenia gravis. In thymomas, myasthenia gravis is most frequent in type B2 thymoma followed by B1- and B3-subtypes (45). Lately in this journal, Xi et al. provided a decent genetic analysis based upon the Cancer Genome Atlas dataset which could discriminate the two groups of TAMG and non-TAMG through six upregulated genes related to autoreactive T cells and in addition in 4 soluble cytokines (46).
Weakness in different muscle groups with the typical wax and wane pattern in correlation with exercise and rest is specific in myasthenia gravis patients. Muscle groups most affected are extraocular muscles (ptosis, double vision), bulbar muscles (impaired chewing, swallowing and speaking), facial and respiratory muscles (breathlessness up to ventilatory insufficiency). Therapeutic approaches beside thymectomy rest on acetylcholinesterase inhibitors, immunosuppressants (prednisolone, rituximab), plasmapheresis, and intravenous immunoglobulins (47).
Rippling muscle disease
Forms of rippling muscle disease contain an autosomal-dominant inherited variant with caveolin-3 mutations as well as acquired ones amongst others relating to thymomas and/or myasthenia gravis. The latter two are often accompanied by neuronal anti-AChR-antibodies. Clinically, patients present with rolling or wave-like muscle movements as well as stiffness.
Immunosuppressive as well as plasmapheresis are potential treatment options (48).
Lambert-Eaton myasthenic syndrome
Autoantibodies against P/Q-type voltage-gated calcium channels (VGCC) are predominantly found in LEMS which lead to a presynaptic disorder of the neuromuscular transmission due to their directly damaging impact and at the same time help to distinguish LEMS from myasthenia gravis. Related findings include the triad of proximal muscle weakness, autonomic dysfunctions and attenuated tendon reflexes, in addition coprostasis. Commonly, LEMS precedes the detection of thymoma or other related malignancies. 3,4 diaminopyridine phosphate, both in mono therapy or in combination with physostigmine may serve as symptomatic treatment (49).
Neuromyotonia (Isaacs’ syndrome)
Isaacs’ syndrome is based on a dysfunction of peripheral nerve voltage-gated potassium channels (VGKC). Unlike the primary genetic variant, in thymoma, secondary acquired forms take place for some of which VGKC-antibodies have been described. Fasciculations up to cramps, stiffness or consecutive hypertrophy of muscle are seen in patients. Therapeutic options include phenytoin and carbamazepine as sodium channel blockers as well as other anticonvulsants, but may warrant also plasmapheresis in refractory cases (50).
Morvan’s syndrome
Classical Morvan’s syndrome is composed of the combination of neuromyotonia/myokymia as well as the autonomic findings hyperhidrosis, insomnia, and encephalopathy. Anti-VGKC-antibodies, in particular anti-CASPR2 antibodies are thought to be causative for the manifold manifestations. Beside immunosuppressives, symptomatic agents are given to ameliorate autonomic symptoms as outlined in a case report by Vale et al. (51).
Ophthalmological system
Keratoconjunctivitis sicca
Keratoconjunctivitis sicca is scarcely addressed in three case reports in which immunosuppressives (corticosteroids, cyclosporine) were topically administered. No potentially causal antibodies were reported. However, cutaneous lichen planus was co-existing in all three thymoma cases as a synchronous AID/PNS manifestation which may have therefore been the potential trigger of keratoconjunctivitis in all of them (52-54).
Retinopathy
Diagnostic criteria for autoimmune retinopathy including paraneoplastic forms were proposed by Sobrin based on the consensus paper for non-paraneoplastic retinopathy from 2016 by specialists of the American Uveitis Society. The diagnosis is based on 5 essential criteria, 4 related to opthalmological exams and 1 to the presence of antiretinal antibodies. Treatment recommendations suggested the use of steroids and/or immunosuppressives as first- or second-line as well as biologics and intravenous immunoglobulins in refractory cases (55,56).
In their case series, Makiyama et al. described the courses of 8 patients with paraneoplastic retinopathies. The single thymoma patient in this series complained of a rapid decrease of visual acuity and contraction of vision field. Serologic testing prompted the presence of anti-photoreceptor antibodies. The treatment included systemic corticosteroid as well as plasmapheresis and intravenous immunoglobulins (57).
Neuromyelitis optica (Devic’s syndrome)
Neuromyelitis optica, also known as Devic’s syndrome, refers to the coincidental inflammation/demyelination of the optic nerve and the spinal cord. The combination Anti-aquaporin-4 (AQP4)- as well as anti-Hu (ANNA-1)-antibodies were detected in thymoma patients who were diagnosed with neuromyelitis optica and were symptomatic with imminent vision loss. Immunosuppressive treatment is favoured (58,59).
Otorhinolaryngological system
Bilateral rigid/calcified auricles
Although a rare finding, rigid bilateral auricles in clinical palpation, with signs of bilateral ossification of the auricles in imaging may be paraneoplastic in nature and serve as a warning sign for causative secondary adrenal insufficiency as depicted in the case presented by Koning et al. (60).
Cochleovestibulopathies
Cochleovestibulopathies are covered under cranial and peripheral sensory(-motor) neuropathies above.
Cardiovascular system
Myocarditis
Myocarditis is a rare paraneoplastic syndrome in thymoma patients, however most often with life-threatening complications due to acute heart failure and/or malignant cardiac arrhythmias (i.e., ventricular tachycardia, sick sinus syndrome, atrioventricular block). Co-incident myositis and myasthenia gravis as well as the occurrence of severe acute heart failure in the short-term perioperative phase after thymectomy were reported. Giant cell myocarditis is the histopathological correlate (61-66).
Suzuki et al. pointed out the predictive value of anti-Kv1.4-antibodies relating to autoimmune myocarditis. In their cohort, 70 out of 650 patients had positive anti-Kv1.4-antibodies, 60% of them showed abnormal ECG findings. Myocarditis was present in 8 of these patients, whereas no myocarditis at all was seen in anti-Kv1.4-negative patients (67).
In their review on giant cell myocarditis, Xu et al. suggested immunosuppressive ciclosporine-based combinations as preferred medical therapies since improved, transplant-free 5-year survival rates up to 72% were shown hereunder compared to death or need for heart transplantation within 3 months without adequate immunosuppression (68).
Vein thrombosis
Ball et al. published a thymoma patient case with development of a deep arm vein thrombosis (69).
Respiratory system
Literature on potential respiratory system manifestations of AID/PNS is almost not existing. Ferré et al. described co-existing lung diseases (ground glass opacities, bronchiectasis) in 13 out of 62 thymoma patients who were also symptomatic with chronic cough or dyspnea. Six out of these 13 patients revealed autoantibodies against the lung-specific bactericidal/permeability-increasing fold-containing B1 (BPIFB1) and/or the potassium channel regulator KCNRG (70). Maiolo et al. depicted a thymoma case with a nonspecific interstitial pneumonia (NSIP)-pattern (71). The presence of diffuse panbronchiolitis was associated to thymoma in two Japanese case reports (72,73). Sarcoidosis is seldom reported in thymoma patients (74,75).
Gastrointestinal system
Evidence indicates also rare AID/PND affections of the gastrointestinal system in thymoma patients, namely autoimmune hepatitis and different forms of colitis. Secondary infectious enteritis due to immune incompetence is dealt with in the subsection on Good syndrome/hypogammaglobulinemia below.
Autoimmune hepatitis
The already mentioned French study by Bernard et al. detected 1 patient with autoimmune hepatitis and reported on another 9 patients in the literature. Patients had in the majority synchronous diagnoses of autoimmune hepatitis and thymoma, interestingly, in 1 patient the onset of autoimmune hepatitis was not before 4 years after thymoma detection. Concomitant AID/PNS were common. Response to immunosuppressive medication (corticosteroids, azathioprine) was favourable (20). Most recently, Stilwell et al. presented a patient with autoimmune hepatitis preceding the diagnosis of a thymoma whose initially raised transaminases became normal after thymectomy as well as adjuvant chemotherapy including dexamethasone but increased again after its completion (76).
Autoimmune cholangitis
According to literature, cholangitis was associated as an autoimmune feature in thymoma. Antibody-profiles revealed positive antinuclear antibodies, but no antimitochondrial antibodies in one patient (73,77).
Autoimmune pancreatitis
Colaut et al. characterized a patient with thymoma who developed clinical signs of pancreatitis. Autoantibodies against pancreatic insulin were detected. Findings resolved after thymectomy (78).
Graft-versus-host disease-like colitis
Several authors published case reports on graft-versus-host disease-like colitis in which persistent diarrhoea required immunosuppressive regimes (79-82).
Ulcerative colitis
In 1967, Kirk et al. reported on a patient with thymoma, hypogammaglobulinemia and ulcerative colitis in whom diarrhoea improved after thymoma-resection (83). In 2001, Okubo et al. described a similar scenario of a patient with thymoma and co-existing ulcerative colitis. Equally, gastrointestinal symptoms dissolved completely after thymectomy (84).
Chronic gastrointestinal dysmotility/pseudo-obstruction
Gastrointestinal dysmotility or even pseudo-obstruction in thymoma both outreach to the gastric, intestinal as well as colonic sections of the gastrointestinal tract. Autoantibody-patterns include VGKC as well as neuronal AChR as targets. Prokinetic agents (i.e., pyridostigmine) and immunosuppressive therapies (corticosteroids, intravenous immunoglobulins) were utilized (85-89).
Renal and urinary tract system
Glomerulopathies
Both, non-proliferative and proliferative glomerulopathies were associated with systemic autoimmune features in thymomas, namely minimal change disease, membranous nephropathy and focal segmental glomerulosclerosis as well as membranoproliferative glomerulonephritis and crescentic glomerulonephritis (rapidly progressive glomerulonephritis) as outlined in a former review by Bacchetta et al. (90) and in recent case reports (91-95). Pronounced in the non-proliferative glomerulopathies, nephrotic syndrome is frequently encountered as complication which itself bears the risk of secondary thrombosis or infections due to renal protein loss. Responses to immunosuppressive agents in combination with thymoma-specific treatments were described as quite favourable (90-95). The underlying pathophysiologies are still inadequately understood but seem to involve different mechanisms of AID as well as PNS eliciting the distinct glomerulopathy variants (96). Independently, the evidently higher prevalence of glomerulopathies in various malignancies compared to the general population should warrant clinicians to check for thymomas and other cancer types at the time of diagnosis as well as during the course of glomerulopathies (97). In their review, de Oliveira Filgueira et al. added tubulopathies as well as extrarenal disorders affecting the tubules to the list of paraneoplastic renal syndromes. These are addressed in the endocrinological subsection of our review (98).
Genital system
As far as we know, beside a vulvovaginal lichen planus manifestation (99), no AID/PNS manifestations primarily originating in female or male genital organs relating to thymoma have been reported in the literature. Interestingly, Hechtman et al. did not detect any unfolding of AID or PNS in two pregnant thymoma patients (100).
Integumentary system
In their publication from 1987 on 172 thymoma patients, Gibson et al. found a mixture of cutaneous disorders in 19 thymoma patients including pemphigus, lichen planus, dermatomyositis and lupus-like skin lesions (the latter two disorders are covered in the immune system subsection). In addition, the case series addressed also cutaneous fungal infections owing to impaired immune system (101). In the latter context, Beck et al. reported on a fatal thymoma case following a chronic cutaneous herpes simplex infection as a consequence of hypogammaglobulinemia (102).
Thymoma-associated multiorgan autoimmunity (TAMA) which causes also regularly dermatological involvements is thematized in the immune system subsection as well (103).
Pemphigus
Pemphigus denotes a group of potentially fatal bullous disorders in which acantholysis induces intraepithelial blister formation, either in skin or mucosa, through circulating autoantibodies which target intercellular adhesion molecules. In paraneoplastic pemphigus, envoplakin and periplakin, but also desmoglein 1 and 3 have been described as autoantigens, the latter two also in the variants pemphigus vulgaris and foliaceus (104,105). Various immunosuppressives (corticosteroids, azathioprine, mycophenolate mofetil, ciclosporine, rituximab, cyclophosphamide) as well as plasmapheresis and intravenous immunoglobulins have been applied in paraneoplastic pemphigus, yet, 1-year survival rate has been stated low with 49% (106). Serious and burdensome involvement of mucosa by pemphigus was reported in thymoma patients, also patterns resembling pemphigus vulgaris or foliaceus (107,108).
Lichen planus
Lichen planus is rarely associated with thymomas. Beside cutaneous lichen planus (= papules, plaques with typical white lines), oral lichen planus (= affects oral cavity, like cutaneous form) and lichen planus planopilaris (= perifollicular erythema, follicular hyperkeratosis and persisting hair loss) were previously reported, in addition evolvement of cicatrizing conjunctivitis. Autoreactive T cells are the potential trigger in thymoma patients provoking epithelial cell apoptosis. Immunosuppressive medication (oral/topical corticosteroids, topical tacrolimus, retinoids) and intravenous immunoglobulins were applied. The benefit of thymectomy was considered as divergent (109-112).
Other cutaneous manifestations
Scleromyxedema (113), acrokeratosis paraneoplastica (Bazex syndrome) (114), Leser-Trélat sign (= rapid onset of seborrheic keratoses) (115), Sweet’s syndrome (= acute febrile neutrophilic dermatosis with painful plaques) (116), vitiligo vulgaris (117) and alopecia (118) were reported sporadically in thymic tumours.
Haematological system
Haematological AID and PNS in thymoma affect red and white blood cells as well as platelets. Pathophysiology has been well-described in pure red cell aplasia in which T cell-mediated autoreactive processes are considered as main underlying mechanisms leading to reduction of bone marrow erythropoiesis, however, autoantibodies may play a causative role as well. Disorders of other haematological cell lines seem to share analogous triggers but have been less well explored (119).
Pure red cell aplasia
Acquired pure red cell aplasia is one of the more common AID in thymomas. Moriyama et al. shared their monocentric experiences of 8 thymoma patients with pure red cell aplasia. Diagnoses of pure red cell aplasia were succeeding thymoma resection in all but one patient with a median of 56 months (range, 1–101 months). Ciclosporine treatment resulted in good response, but remarkably all patients developed complicative pneumonia, lethal in 4 patients (120). Balasubramanian et al. reviewed recently the management of pure red cell aplasia and quoted the overall response rate of first line ciclosporine with 76% (121).
Other forms of anaemia
Aplastic anaemia (122), haemolytic anaemia (123) and pernicious anaemia (124) represent other anaemia variants in thymoma which were reported in the literature. Gendron et al. provided comprehensive observational data from the French Reference Centre of aplastic anaemia on 9 own and 26 literature-based patients (125).
Paroxysmal nocturnal haemoglobinuria
Palmieri et al. reported on the occurrence of paroxysmal nocturnal haemoglobinuria in a thymoma patient seven years after thymectomy. Causatively, they were able to attribute the reduction of circulating erythroid and myeloid progenitors to altered CD8+ T cells in this patient (126).
Pure white cell aplasia (agranulocytosis)
Pure white cell aplasia constitutes the equivalent to pure red cell aplasia with agranulocytosis due to suppressed granulopoiesis. Consecutively, immunosuppression with severe infections may occur (127-129).
Good syndrome, hypogammaglobulinemia
Good syndrome relates to thymoma in combination with hypogammaglobulinemia because of reduced or missing B cells, reduced T cells and an inverted CD4+/CD8+ T cell ratio which results in secondary immune incompetence (130).
Peripheral T cell lymphocytosis
Peripheral T cell lymphocytosis may indicate more aggressive behaviour in thymoma. Thymectomy and/or systemic chemotherapy as well as radiation therapy positively influence lymphocytosis (131).
Acquired amegakaryocytic thrombocytopenia
Acquired amegakaryocytic thrombocytopenia is rare and occurs sometimes in combination with pure red cell aplasia (132,133). Simkins et al. reported on a patient who developed aplastic anaemia under acquired amegakaryocytic thrombocytopenia and was successfully treated with allogenic stem cell transplantation (134).
Endocrine system
Different endocrine glands encompassing distinct parts of the corresponding hormone axes can be involved in thymoma-related AID/PNS. Therapies are built on immunosuppression and hormonal treatments according to the underlying endocrine disorder.
Autoimmune pituitary diseases
Autoimmune pituitary disease in thymoma can result in combined deficiencies of thyroid-stimulating hormone, growth hormone, prolactin, and adrenocorticotropic hormone (ACTH). Anti-PIT-1 antibodies and PIT-1-reactive cytotoxic T cells seem to be crucial in the pathogenesis. Isolated ACTH paucity has also been reported (135).
Autoimmune thyroid diseases
Kubiszewska et al. provided data on 343 consecutive myasthenia gravis patients of whom 92 patients were also diagnosed with autoimmune thyroid disease. Hashimoto’s thyroiditis, Grave’s disease and antithyroid antibodies only were detected in 9%, 4% and 13%, respectively (136).
Autoimmune parathyroid diseases, humoral hypercalcaemia of malignancy
Hypoparathyroidism (137) and hyperparathyroidism (138) as well as parathyroid hyperplasia (139) have been described in thymoma patients. Besides, parathyroid hormone related protein (PTHrP)-mediated humoral hypercalcemia in malignancy needs to be considered as well, life-threatening conditions may arise (140).
Other endocrine disorders
Cushing’s syndrome (141), Addison’s disease (142), syndrome of inappropriate antidiuretic hormone (143), and type I diabetes (144) have been also associated with thymoma.
Immune system
Thymomas may initiate or at least interact with and augment several immunological diseases. Moreover, thymomas bear the potential to cause systemic AID/PNS affecting multiple sites themselves.
Rheumatological disorders
Thymoma has been connected with several rheumatological disorders: rheumatoid arthritis (145), cutaneous and systemic lupus erythematosus (146), systemic sclerosis (147), Sjogren’s syndrome (148), multicentric reticulohistiocytosis (149), cryoglobulinemia (150), Raynaud’s phenomena (151), eosinophilic granulomatosis with polyangiitis (152), Takayasu arteritis (153) as well as dermatomyositis/myositis (154-156). Most recently, Noël et al. described 14 thymoma patients with co-existing systemic lupus erythematosus. Pleural or pericardial effusions as well as joint- and skin-manifestations occurred in more than 50% of these patients. Treatment consisted mostly of prednisone and hydroxychloroquine (157).
Thymoma-associated multiorgan autoimmunity
Wadhera et al. coined thymoma-associated multiorgan autoimmunity (TAMA) to label a systemic graft-versus-host-like disease in thymoma. TAMA affects thyroid, gastrointestinal tract, liver and skin (103). This T cell mediated disorder is histopathologically akin to a graft-versus-host disease pattern (158). Literature provides some rather complex case reports (159-161).
Co-incidental, but pathogenetic separate AID/PNS which do not share equal graft-versus-host-like disease mechanisms should be differentiated from this systemic disorder in thymomas. Bernard et al. demonstrated that 7% of their thymoma-cohort revealed at least 2 AID/PNS (20), Gong et al. brought up a thymoma case with 7 different AID/PNS manifestations (162).
Course and Prognosis of AID and PNS
In the large ITMIG cohort, Padda et al. demonstrated that presence of AID/PNS in all thymic tumours correlated with a significantly lower cumulative incidence of recurrence compared to AID/PNS absence (10-year: 17.3% vs. 21.2%; 20-year: 27.2% vs. 28.1%; 30-year: 29.5% vs. 39.4%; P=0.0003). Overall survival was significantly better in the cohort of AID/PNS-positive thymic tumours (median OS 21.6 vs. 17.0 years; HR 0.63, 95% CI: 0.54–0.74; P<0.0001). However, in multivariate analysis AID/PNS did not prove as an independent factor relating to recurrence-free survival and overall survival. Independent predictive factors were instead older age, thymic carcinoma and NETT histology, advanced stage III-IVB, chemotherapy applied within a curative setting and R2-status (4).
Filosso et al. described in their Italian thymoma cohort for patients with myasthenia gravis and those without 5- and 10-year survival rates of 93.6% vs. 84.9% and 77.2% vs. 70.9% (univariate analysis: HR 0.74, 95% CI: 0.54–1.01; P=0.058; multivariate analysis: adjusted HR 0.99, 95% CI: 0.71–1.38; P=0.956). Five- and 10-year cumulative incidence of recurrence were calculated in the myasthenia against the non-myasthenia group with 10.7% vs. 11.1% and 14.7% vs. 15.7% (P=0.827) (16).
Wang et al. revealed in their Chinese ChART-cohort for all thymic tumour patients with myasthenia gravis both a significantly lower tumour recurrence rate and a better 5-/10-year overall survival compared to those without myasthenia gravis (5-year: 93% vs. 88%; 10-year: 83% vs. 81%; P=0.034). Yet, myasthenia gravis was no independent predictive factor in the multivariate analysis (in contrast to WHO classification, Masaoka stage and resectability) (18).
The retrospective analysis of the JART database by Nakajima et al. showed comparable 5- and 10-year overall survival and recurrence-free rates in myasthenic and non-myasthenic thymoma patients (19).
In their appraisal of the ESTS database, Ruffini et al. identified age, histology, Masaoka stage and R status as independent parameters in multivariate analysis, but again not myasthenia gravis (14).
Although solely based on case reports and case series, the systematic review by Zhao et al. provided some detailed insights into AID/PNS thymoma patient characteristics. Out of the 547 patients from all assessed publications, 507 patients (93%) received initial thymoma resection either as mono therapy (59%) or in a multimodal concept (34%). The remaining patients without surgical resection (7%) were excluded from further analysis. In the 407 patients with presence of PNS at the time of surgical thymoma resection, PNS findings reportedly regressed in 308 patients (76%) and subsequently flared up again as recurrence or new PNS in 100 of these patients (21%) (within a time range from 1 month to 19 years after surgery). In contrast, 72 patients (18%) were characterized with persisting PNS out of whom 29 (40%) developed additional PNS. The 5-, 10-, 15- and 20-year overall survival rates of 395 PNS patients with available follow-up data were calculated with 78%, 66%, 59%, and 35%, respectively. Total resolution of PNS was the only independent predictor of favourable overall survival in multivariate analysis. Reported AID/PNS treatment modalities in the 507 operated patients were composed of immunosuppressives (corticosteroids 30%, azathioprine 5%, ciclosporine 2%), immunomodulation (plasmapheresis 8%, intravenous immunoglobulins 7%), anti-cholinergics (19%), transfusion (2%) and others (27%) (30).
Thymectomy is the mainstay of care in resectable thymomas. Its beneficial impact on the course of AID and PNS in thymoma patients has been assumed quite a while, but this is only moderately backed by literature. The only randomized-controlled trial on thymectomy in myasthenia gravis by Wolfe et al. demonstrated better outcomes in the surgical arm, yet enrolled only non-thymomatous patients (163). In their recent review, Comacchio et al. listed 30 case series which depicted results of minimally invasive VATS or robotic thymectomy including patients with thymoma and myasthenia gravis (publication years: 2000–2017; number of total patients per series: 14–134). While the reported 5-year overall survival rates were 97–100%, the myasthenia remission rates were varying widely across studies (complete remission: 28.5–70%, improvement 73–100%) (164). Likewise, other reviews distilled the positive prognostic impact of thymectomy in patients with myasthenia gravis (165-170) and also in non-myasthenic AID/PNS (20,171) based on uncontrolled case series as supporting evidence. Conclusively, extended thymectomy seems to play a crucial role in the improvement and control of AID/PNS in thymoma. Beside the complete resection of the thymus, removal of adjacent extracapsular cervical and mediastinal fat tissues is essential as well since ectopic thymic tissues are prone to cause AID/PNS relapse (169,172,173). Perioperative complication rates in thymectomy have been significantly reduced in the past, particularly through identification of risk factors for acute myasthenic crisis (174) and accounting for them in modern anaesthesiology (175). Bernard et al. pointed towards sustained complex defects in T cell clones after thymic maturation as well as systemic deployment of autoreactive T cells before thymectomy as further triggers of AID/PNS relapse in completely resected thymoma patients (20).
Systemic therapies are acknowledged as an important backbone in treatment of advanced and relapsing thymomas in current guidelines and by that may also positively affect AID and PNS (27-29). Berghmans et al. systematically reviewed their oncological effectiveness demonstrating response rates over 50% for platinum-based regimens (176). Prompted by commonly high-expression of PD-L1 as exemplarily shown by Rouquette et al. in Type B3 thymomas (177), immunotherapies with checkpoint-inhibitors are currently under investigation in thymomas. The efficacy and tolerability of the 2 PD-L1 antibodies pembrolizumab and avelumab were subject in 2 phase-2-trials in relapsed thymomas. While response rates were very favourable with approximately 28%, a substantial proportion of patients developed serious adverse events including myocarditis, hepatitis, polymyositis and myasthenia gravis (178,179). Other case reports on other life-threatening events due to immunotherapy in thymomas have been published recently. Whether these events were due to direct PD-L1 inhibitor side effects or the aggravation of underlying AID/PNS has not been clarified up to now, nevertheless, recommendation for the usage of checkpoint inhibitors in relapsed thymoma cannot be given yet under these circumstances. Further evidence in larger cohorts as well as identification of mechanisms and risk factors for adverse events under checkpoint inhibitor therapies in thymoma patients are needed first (180,181).
Conclusions and outlook
In summary, AID/PNS are common and multifaceted in the orphan disease of thymoma, the underlying pathophysiology in thymoma and distant organs affected by AID/PNS is complex and still not fully understood. Based on evidence deriving mostly from case reports and thereby the risk of publication bias, AID and PNS seem to vary widely in terms of acuteness and magnitude of morbidities as well as mortality, both depending on individual patient factors, the kind of AID/PNS as well as oncological characteristics and residual status of the thymoma. Thymoma patients are at risk of suffering and dying from (I) oncologically uncontrolled thymoma, (II) serious conditions in associated AIP/PNS, (III) diverse mechanisms of impaired immunocompetence in thymoma and AID/PNS resulting in infections or secondary malignancies, and (IV) therapy-related complications, respectively (5,9,10,20). Currently, the role of immunotherapy with checkpoint-inhibitors in systemic thymoma therapy is under controversial debate due to the discrepancy of promising efficacy, but obviously much higher risk of life-threatening adverse events compared to their application in other malignancies. Consequently, clinicians and thymoma patients should be aware of AID and PNS in order to enable earlier diagnosis and treatment preventing more harmful courses. Finally, joint international initiatives towards multicentric, prospective data registries linked to translational research initiatives are key to provide better evidence in the future and by that to clarify the remaining myths of AID and PNS more than a century after their first descriptions.
Acknowledgments
Funding: This work was supported by an unrestricted grant from Stiftung Oskar Helene Heim, Berlin, Germany.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editors (Dragana Jovanovic and Semra Bilaceroglu) for the series “Thymoma” published in Journal of Thoracic Disease. The article was sent for external peer review organized by the Guest Editors and the editorial office.
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at: http://dx.doi.org/10.21037/jtd-2019-thym-10). The series “Thymoma” was commissioned by the editorial office without any funding or sponsorship. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Marx A, Chan JK, Coindre JM, et al. The 2015 World Health Organization Classification of Tumors of the Thymus: Continuity and Changes. J Thorac Oncol 2015;10:1383-95. [Crossref] [PubMed]
- Auche M. Des nevrites peripheriques chez les cancereux. Rev Med 1890;10:785-807.
- Weigert C. Pathologisch-anatomischer Beitrag zur Erb’schen Krankheit (Myasthenia gravis). Neurol Zentralbl 1901;20:597-601.
- Padda SK, Yao X, Antonicelli A, et al. Paraneoplastic Syndromes and Thymic Malignancies: An Examination of the International Thymic Malignancy Interest Group Retrospective Database. J Thorac Oncol 2018;13:436-46. [Crossref] [PubMed]
- Rajan A, Zhao C. Deciphering the biology of thymic epithelial tumors. Mediastinum 2019;3:36. [Crossref] [PubMed]
- British Society for Immunology. Autoimmunity. London, 2016. [Available online: https://www.immunology.org/sites/default/files/autoimmunity-briefing.pdf, last accessed: 01.02.2020].
- Darnell RB, Posner JB. Definitions, classifications, history, epidemiology, and importance. Paraneoplastic Syndromes. Oxford: Oxford University Press, 2011:3-28.
- Girard N. Thymic Tumors: Revisiting Autoimmunity to Give a Chance to Immunotherapy. J Thorac Oncol 2018;13:295-7. [Crossref] [PubMed]
- Cheng M, Anderson MS. Thymic tolerance as a key brake on autoimmunity. Nat Immunol 2018;19:659-64. [Crossref] [PubMed]
- Lippner EA, Lewis DB, Robinson WH, et al. Paraneoplastic and Therapy-Related Immune Complications in Thymic Malignancies. Curr Treat Options Oncol 2019;20:62. [Crossref] [PubMed]
- Radovich M, Pickering CR, Felau I, et al. The Integrated Genomic Landscape of Thymic Epithelial Tumors. Cancer Cell 2018;33:244-258.e10. [Crossref] [PubMed]
- Yu L, Ke J, Du X, et al. Genetic characterization of thymoma. Sci Rep 2019;9:2369. [Crossref] [PubMed]
- Henry K. Paraneoplastic syndromes: Definitions, classification, pathophysiology and principles of treatment. Semin Diagn Pathol 2019;36:204-10. [Crossref] [PubMed]
- Ruffini E, Detterbeck F, Van Raemdonck D, et al. Tumours of the thymus: a cohort study of prognostic factors from the European Society of Thoracic Surgeons database. Eur J Cardiothorac Surg 2014;46:361-8. [Crossref] [PubMed]
- Ruffini E, Detterbeck F, Van Raemdonck D, et al. Thymic carcinoma: a cohort study of patients from the European society of thoracic surgeons database. J Thorac Oncol 2014;9:541-8. [Crossref] [PubMed]
- Filosso PL, Evangelista A, Ruffini E, et al. Does myasthenia gravis influence overall survival and cumulative incidence of recurrence in thymoma patients? A Retrospective clinicopathological multicentre analysis on 797 patients. Lung Cancer 2015;88:338-43. [Crossref] [PubMed]
- Kondo K, Monden Y. Thymoma and myasthenia gravis: a clinical study of 1,089 patients from Japan. Ann Thorac Surg 2005;79:219-24. [Crossref] [PubMed]
- Wang F, Pang L, Fu J, et al. Postoperative survival for patients with thymoma complicating myasthenia gravis-preliminary retrospective results of the ChART database. J Thorac Dis 2016;8:711-7. [Crossref] [PubMed]
- Nakajima J, Okumura M, Yano M, et al. Myasthenia gravis with thymic epithelial tumour: a retrospective analysis of a Japanese database. Eur J Cardiothorac Surg 2016;49:1510-5. [Crossref] [PubMed]
- Bernard C, Frih H, Pasquet F, et al. Thymoma associated with autoimmune diseases: 85 cases and literature review. Autoimmun Rev 2016;15:82-92. [Crossref] [PubMed]
- Marx A, Willcox N, Leite MI, et al. Thymoma and paraneoplastic myasthenia gravis. Autoimmunity 2010;43:413-27. [Crossref] [PubMed]
- Ruffini E, Guerrera F, Brunelli A, et al. Report from the European Society of Thoracic Surgeons prospective thymic database 2017: a powerful resource for a collaborative global effort to manage thymic tumours. Eur J Cardiothorac Surg 2019;55:601-9. [Crossref] [PubMed]
- Vedeler CA, Antoine JC, Giometto B, et al. Paraneoplastic neurological syndromes. In: Gilhus NE, Barnes MP, Brainin M. editors. European Handbook of Neurological Management: Volume 1, 2nd Edition. New Jersey: Blackwell Publishing Ltd., 2011:447-57.
- Graus F, Delattre JY, Antoine JC, et al. Recommended diagnostic criteria for paraneoplastic neurological syndromes. J Neurol Neurosurg Psychiatry 2004;75:1135-40. [Crossref] [PubMed]
- Vedeler CA, Antoine JC, Giometto B, et al. Management of paraneoplastic neurological syndromes: report of an EFNS Task Force. Eur J Neurol 2006;13:682-90. [Crossref] [PubMed]
- Sanders DB, Wolfe GI, Benatar M, et al. International consensus guidance for management of myasthenia gravis: Executive summary. Neurology 2016;87:419-25. [Crossref] [PubMed]
- Girard N, Ruffini E, Marx A, et al. Thymic epithelial tumours: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann Oncol 2015;26 Suppl 5:v40-55. [Crossref] [PubMed]
- Imbimbo M, Ottaviano M, Vitali M, et al. Best practices for the management of thymic epithelial tumors: A position paper by the Italian collaborative group for ThYmic MalignanciEs (TYME). Cancer Treat Rev 2018;71:76-87. [Crossref] [PubMed]
- National Comprehensive Cancer Network (NCCN). NCCN Clinical Practice Guideline in Oncology (NCCN Guidelines). Thymoma and Thymic Carcinomas. Version 2020.1 2019. [Available online: https://www.nccn.org/professionals/physician_gls/default.aspx#site, last accessed: 10.02.2020].
- Zhao J, Bhatnagar V, Ding L, et al. A systematic review of paraneoplastic syndromes associated with thymoma: Treatment modalities, recurrence, and outcomes in resected cases. J Thorac Cardiovasc Surg 2020;160:306-14.e14. [Crossref] [PubMed]
- Lancaster E. Paraneoplastic disorders. Continuum (Minneap Minn) 2015;21:452-75. [Crossref] [PubMed]
- Giometto B, Grisold W, Vitaliani R, et al. Paraneoplastic neurologic syndrome in the PNS Euronetwork database: a European study from 20 centers. Arch Neurol 2010;67:330-5. [Crossref] [PubMed]
- Grativvol RS, Cavalcante WCP, Castro LHM, et al. Updates in the Diagnosis and Treatment of Paraneoplastic Neurologic Syndromes. Curr Oncol Rep 2018;20:92. [Crossref] [PubMed]
- Jubelt B, Mihai C, Li TM, et al. Rhombencephalitis / brainstem encephalitis. Curr Neurol Neurosci Rep 2011;11:543-52. [Crossref] [PubMed]
- Oh SY, Kim JS, Dieterich M. Update on opsoclonus-myoclonus syndrome in adults. J Neurol 2019;266:1541-8. [Crossref] [PubMed]
- Mitoma H, Manto M, Hampe CS. Immune-mediated Cerebellar Ataxias: Practical Guidelines and Therapeutic Challenges. Curr Neuropharmacol 2019;17:33-58. [Crossref] [PubMed]
- El-Abassi R, Soliman MY, Villemarette-Pittman N, et al. SPS: Understanding the complexity. J Neurol Sci 2019;404:137-49. [Crossref] [PubMed]
- Morise S, Nakamura M, Morita JI, et al. Thymoma-associated Progressive Encephalomyelitis with Rigidity and Myoclonus (PERM) with Myasthenia Gravis. Intern Med 2017;56:1733-7. [Crossref] [PubMed]
- Antoine JC, Camdessanche JP. Paraneoplastic neuropathies. Curr Opin Neurol 2017;30:513-20. [Crossref] [PubMed]
- Kumar K, Ahmed R, Bajantri B, et al. Tumors Presenting as Multiple Cranial Nerve Palsies. Case Rep Neurol 2017;9:54-61. [Crossref] [PubMed]
- Xu Q, Du W, Zhou H, et al. Distinct clinical characteristics of paraneoplastic optic neuropathy. Br J Ophthalmol 2019;103:797-801. [Crossref] [PubMed]
- Greene JJ, Keefe MW, Harris JP, et al. Paraneoplastic syndrome: a masquerade of autoimmune inner ear disease. Otol Neurotol 2015;36:e3-10. [Crossref] [PubMed]
- Kattah JC. Clinical Characteristics and Etiology of Bilateral Vestibular Loss in a Cohort from Central Illinois. Front Neurol 2018;9:46. [Crossref] [PubMed]
- Vernino S, Cheshire WP, Lennon VA. Myasthenia gravis with autoimmune autonomic neuropathy. Auton Neurosci 2001;88:187-92. [Crossref] [PubMed]
- Marx A, Ströbel P, Weis CA. The pathology of the thymus in myasthenia gravis. Mediastinum 2018;2:66. [Crossref]
- Xi J, Wang L, Yan C, et al. The Cancer Genome Atlas dataset-based analysis of aberrantly expressed genes by GeneAnalytics in thymoma associated myasthenia gravis: focusing on T cells. J Thorac Dis 2019;11:2315-23. [Crossref] [PubMed]
- Souto EB, Lima B, Campos JR, et al. Myasthenia gravis: State of the art and new therapeutic strategies. J Neuroimmunol 2019;337:577080. [Crossref] [PubMed]
- Bettini M, Gonorazky H, Chaves M, et al. Immune-mediated rippling muscle disease and myasthenia gravis. J Neuroimmunol 2016;299:59-61. [Crossref] [PubMed]
- Verschuuren J, Strijbos E, Vincent A. Neuromuscular junction disorders. Handb Clin Neurol 2016;133:447-66. [Crossref] [PubMed]
- Rana SS, Ramanathan RS, Small G, et al. Paraneoplastic Isaacs' syndrome: a case series and review of the literature. J Clin Neuromuscul Dis 2012;13:228-33. [Crossref] [PubMed]
- Vale TC, Pedroso JL, Dutra LA, et al. Morvan syndrome as a paraneoplastic disorder of thymoma with anti-CASPR2 antibodies. Lancet 2017;389:1367-8. [Crossref] [PubMed]
- Hon C, Chui WH, Cheng LC, et al. Thymoma associated with keratoconjunctivitis, lichen planus, hypogammaglobinemia, and absent circulating B cells. J Clin Oncol 2006;24:2960-1. [Crossref] [PubMed]
- Feinsilber D, Mears KA, Pettiford BL. Polyparaneoplastic Manifestations of Malignant Thymoma: A Unique Case of Myasthenia, Autoimmune Hepatitis, Pure Red Cell Aplasia, and Keratoconjunctivitis Sicca. Cureus 2017;9:e1374. [Crossref] [PubMed]
- Hahn JM, Meisler DM, Lowder CY, et al. Cicatrizing conjunctivitis associated with paraneoplastic lichen planus. Am J Ophthalmol 2000;129:98-9. [Crossref] [PubMed]
- Sobrin L. Progress Toward Precisely Diagnosing Autoimmune Retinopathy. Am J Ophthalmol 2018;188:xiv-xv. [Crossref] [PubMed]
- Fox AR, Gordon LK, Heckenlively JR, et al. Consensus on the Diagnosis and Management of Nonparaneoplastic Autoimmune Retinopathy Using a Modified Delphi Approach. Am J Ophthalmol 2016;168:183-90. [Crossref] [PubMed]
- Makiyama Y, Kikuchi T, Otani A, et al. Clinical and immunological characterization of paraneoplastic retinopathy. Invest Ophthalmol Vis Sci 2013;54:5424-31. [Crossref] [PubMed]
- Yang HK, Woo SJ, Park WY, et al. Paraneoplastic neuromyelitis optica associated with ANNA-1 antibodies in invasive thymoma. BMC Ophthalmol 2014;14:106. [Crossref] [PubMed]
- Beauchemin P, Iorio R, Traboulsee AL, et al. Paraneoplastic Neuromyelitis Optica Spectrum Disorder: A single center cohort description with two cases of histological validation. Mult Scler Relat Disord 2018;20:37-42. [Crossref] [PubMed]
- Koning MV, Struijs A. Adrenal insufficiency presenting as bilateral rigid auricles: a case report. J Med Case Rep 2014;8:302. [Crossref] [PubMed]
- Karippacheril JG, Shetty R, Sagar SC, et al. Myocarditis after thymoma resection, with left ventricular hypokinesia mimicking acute coronary syndrome. J Anesth 2013;27:805-6. [Crossref] [PubMed]
- Kon T, Mori F, Tanji K, et al. Giant cell polymyositis and myocarditis associated with myasthenia gravis and thymoma. Neuropathology 2013;33:281-7. [Crossref] [PubMed]
- Koul D, Kanwar M, Jefic D, et al. Fulminant giant cell myocarditis and cardiogenic shock: an unusual presentation of malignant thymoma. Cardiol Res Pract 2010;2010:185896. [Crossref] [PubMed]
- Gidron A, Quadrini M, Dimov N, et al. Malignant thymoma associated with fatal myocarditis and polymyositis in a 32-year-old woman with a history of hairy cell leukemia. Am J Clin Oncol 2006;29:213-4. [Crossref] [PubMed]
- Joudinaud TM, Fadel E, Thomas-de-Montpreville V, et al. Fatal giant cell myocarditis after thymoma resection in myasthenia gravis. J Thorac Cardiovasc Surg 2006;131:494-5. [Crossref] [PubMed]
- Tanahashi N, Sato H, Nogawa S, et al. A case report of giant cell myocarditis and myositis observed during the clinical course of invasive thymoma associated with myasthenia gravis. Keio J Med 2004;53:30-42. [PubMed]
- Suzuki S, Baba A, Kaida K, et al. Cardiac involvements in myasthenia gravis associated with anti-Kv1.4 antibodies. Eur J Neurol 2014;21:223-30. [Crossref] [PubMed]
- Xu J, Brooks EG. Giant Cell Myocarditis: A Brief Review. Arch Pathol Lab Med 2016;140:1429-34. [Crossref] [PubMed]
- Ball SL, Cocks HC. Thymoma complicated by deep vein thrombosis of the arm. BMJ Case Rep 2015;2015:bcr2015213404. [Crossref] [PubMed]
- Ferré EM, Break TJ, Burbelo PD, et al. Lymphocyte-driven regional immunopathology in pneumonitis caused by impaired central immune tolerance. Sci Transl Med 2019;11:eaav5597. [Crossref] [PubMed]
- Maiolo C, Fuso L, Benedetto RT, et al. A case of nonspecific interstitial pneumonia associated with thymoma. Sarcoidosis Vasc Diffuse Lung Dis 2003;20:75-6. [PubMed]
- Ogoshi T, Ishimoto H, Yatera K, et al. A case of Good syndrome with pulmonary lesions similar to diffuse panbronchiolitis. Intern Med 2012;51:1087-91. [Crossref] [PubMed]
- Maekawa R, Shibuya H, Hideyama T, et al. A case of myasthenia gravis with invasive thymoma associated with diffuse panbronchiolitis, alopecia, dysgeusia, cholangitis and myositis. Rinsho Shinkeigaku 2014;54:703-8. [Crossref] [PubMed]
- Kurukumbi M, Weir RL, Kalyanam J, et al. Rare association of thymoma, myasthenia gravis and sarcoidosis: a case report. J Med Case Rep 2008;2:245. [Crossref] [PubMed]
- Hato T, Yamaguchi M, Sugiyama A, et al. Hatched "egg" of thymoma with sarcoidosis. World J Surg Oncol 2019;17:151. [Crossref] [PubMed]
- Stilwell KT, Musick SR, Cebe KM, et al. Thymoma-Induced Autoimmune Hepatitis: A Rare Paraneoplastic Syndrome. Cureus 2019;11:e5637. [Crossref] [PubMed]
- Kim JH, Kim BH, Kim YW, et al. Autoimmune cholangitis in a patient with thymoma. J Gastroenterol Hepatol 2004;19:1324-7. [Crossref] [PubMed]
- Colaut F, Toniolo L, Sperti C, et al. Autoimmune-like pancreatitis in thymoma with myasthenia gravis. Chir Ital 2002;54:91-4. [PubMed]
- Sader C, Sharma S, Edwards MG. Graft-versus-host disease-type colitis: an unusual association of malignant thymoma. Ann Thorac Surg 2002;73:1947-8. [Crossref] [PubMed]
- Lowry PW, Myers JD, Geller A, et al. Graft-versus-host-like colitis and malignant thymoma. Dig Dis Sci 2002;47:1998-2001. [Crossref] [PubMed]
- Offerhaus GJ, Schipper ME, Lazenby AJ, et al. Graft-versus-host-like disease complicating thymoma: lack of AIRE expression as a cause of non-hereditary autoimmunity? Immunol Lett 2007;114:31-7. [Crossref] [PubMed]
- Wang MH, Wong JM, Wang CY. Graft-versus-Host disease-like syndrome in malignant thymoma. Scand J Gastroenterol 2000;35:667-70. [Crossref] [PubMed]
- Kirk BW, Freedman SO. Hypogammaglobulinemia, thymoma and ulcerative colitis. Can Med Assoc J 1967;96:1272-7. [PubMed]
- Okubo K, Kondo N, Okamoto T, et al. Excision of an invasive thymoma: a cure for ulcerative colitis? Ann Thorac Surg 2001;71:2013-5. [Crossref] [PubMed]
- Musthafa CP, Moosa A, Chandrashekharan PA, et al. Intestinal pseudo-obstruction as initial presentation of thymoma. Indian J Gastroenterol 2006;25:264-5. [PubMed]
- Greenburg DL, Mo CC, Hemmer PA. IVIG for thymoma-associated pseudo-obstruction: report of successful treatment. Eur Neurol 2007;58:116-7. [Crossref] [PubMed]
- Sekiguchi Y, Takahashi H, Mori M, et al. Potassium channel antibody-associated encephalitis with hypothalamic lesions and intestinal pseudo-obstruction. J Neurol Sci 2008;269:176-9. [Crossref] [PubMed]
- Malhotra K, Georgiades IB, Davies J. Functional colonic obstruction in an adult as a presenting feature of thymoma. Ann R Coll Surg Engl 2011;93:e61-3. [Crossref] [PubMed]
- Carvalho EÁ, Portela AR, Oliveira MVB, et al. Gastric pseudo-obstruction as an initial manifestation of thymoma. J Bras Pneumol 2019;45:e20190081. [Crossref] [PubMed]
- Bacchetta J, Juillard L, Cochat P, et al. Paraneoplastic glomerular diseases and malignancies. Crit Rev Oncol Hematol 2009;70:39-58. [Crossref] [PubMed]
- Ngoh CLY, Goh GHS, Wong WK. Paraneoplastic relapsing minimal change disease associated with type A thymoma in an elderly patient: A case report and literature review. Med J Malaysia 2019;74:97-8. [PubMed]
- Yoo SH, Kim HJ, Kim JH, et al. Nephrotic syndrome associated with metastatic thymoma treated with chemotherapy. Medicine (Baltimore) 2017;96:e5408. [Crossref] [PubMed]
- Myoga H, Akimoto T, Mato N, et al. Nephrotic Syndrome and a Retroperitoneal Mass: A Case Report of a Patient with Recurrent Invasive Thymoma. Intern Med 2017;56:3317-22. [Crossref] [PubMed]
- Hor JY, Lim TT, Cheng MC, et al. Thymoma-associated myasthenia gravis and LGI1-encephalitis, with nephrotic syndrome post-thymectomy. J Neuroimmunol 2018;317:100-2. [Crossref] [PubMed]
- Gharwan H, Tomita Y, Lee MJ, et al. Alterations of immune cell subsets in relapsed, thymoma-associated minimal change disease: A case report. Oncol Lett 2015;10:1155-8. [Crossref] [PubMed]
- Jhaveri KD, Shah HH, Patel C, et al. Glomerular diseases associated with cancer, chemotherapy, and hematopoietic stem cell transplantation. Adv Chronic Kidney Dis 2014;21:48-55. [Crossref] [PubMed]
- Ryu J, Ryu H, Kim S, et al. Comparison of cancer prevalence between patients with glomerulonephritis and the general population at the time of kidney biopsy. PLoS One 2019;14:e0224024. [Crossref] [PubMed]
- de Oliveira Filgueira PH, Vasconcelos LF, da Silva GB, et al. Paraneoplastic syndromes and the kidney. Saudi J Kidney Dis Transpl 2010;21:222-31. [PubMed]
- Moutasim KA, Poate TW, Setterfield JF, et al. A case of vulvovaginal gingival lichen planus in association with Good's syndrome. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2008;105:e57-60. [Crossref] [PubMed]
- Hechtman JF, Chepovetsky JA, Strauchen JA, et al. Thymomas diagnosed during pregnancy: two cases in young women without paraneoplastic or autoimmune disease. Ann Diagn Pathol 2012;16:392-6. [Crossref] [PubMed]
- Gibson LE, Muller SA. Dermatologic disorders in patients with thymoma. Acta Derm Venereol 1987;67:351-6. [PubMed]
- Beck S, Slater D, Harrington CI. Fatal chronic cutaneous herpes simplex associated with thymoma and hypogammaglobulinaemia. Br J Dermatol 1981;105:471-4. [Crossref] [PubMed]
- Wadhera A, Maverakis E, Mitsiades N, et al. Thymoma-associated multiorgan autoimmunity: a graft-versus-host-like disease. J Am Acad Dermatol 2007;57:683-9. [Crossref] [PubMed]
- Zhu X, Zhang B. Paraneoplastic pemphigus. J Dermatol 2007;34:503-11. [Crossref] [PubMed]
- Kridin K. Pemphigus group. overview, epidemiology, mortality, and comorbidities. Immunol Res 2018;66:255-70. [Crossref] [PubMed]
- Maruta CW, Miyamoto D, Aoki V, et al. Paraneoplastic pemphigus: a clinical, laboratorial, and therapeutic overview. An Bras Dermatol 2019;94:388-98. [Crossref]
- Takeshita K, Amano M, Shimizu T, et al. Thymoma with pemphigus foliaceus. Intern Med 2000;39:742-7. [Crossref] [PubMed]
- Lim JM, Lee SE, Seo J, et al. Paraneoplastic Pemphigus Associated with a Malignant Thymoma: A Case of Persistent and Refractory Oral Ulcerations Following Thymectomy. Ann Dermatol 2017;29:219-22. [Crossref] [PubMed]
- Motegi S, Uchiyama A, Yamada K, et al. Lichen planus complicated with thymoma: Report of three Japanese cases and review of the published work. J Dermatol 2015;42:1072-7. [Crossref] [PubMed]
- Teramura K, Kato T, Nishikawa J, et al. Oral lichen planus and lichen planopilaris complicated with thymoma. J Dermatol 2019;46:e237-9. [Crossref] [PubMed]
- Miyagaki T, Sugaya M, Miyamoto A, et al. Oral erosive lichen planus associated with thymoma treated with etretinate. Australas J Dermatol 2013;54:e25-7. [Crossref] [PubMed]
- Khan S, Campbell A, Hunt C, et al. Lichen planus in a case of Good's syndrome (thymoma and immunodeficiency). Interact Cardiovasc Thorac Surg 2009;9:345-6. [Crossref] [PubMed]
- Chan JC, Trendell-Smith NJ, Yeung CK. Scleromyxedema: a cutaneous paraneoplastic syndrome associated with thymic carcinoma. J Clin Oncol 2012;30:e27-9. [Crossref] [PubMed]
- Chave TA, Bamford WM, Harman KE. Acrokeratosis paraneoplastica associated with recurrent metastatic thymic carcinoma. Clin Exp Dermatol 2004;29:430-2. [Crossref] [PubMed]
- Mendes GB, Zanetti G, Marchiori E. Leser-Trelat Sign Secondary to Thymic Carcinoma. Arch Bronconeumol 2018;54:286-7. [PubMed]
- Altomare G, Capella GL, Frigerio E. Sweet's syndrome in a patient with idiopathic myelofibrosis and thymoma-myasthenia gravis-immunodeficiency complex: efficacy of treatment with etretinate. Haematologica 1996;81:54-8. [PubMed]
- Nakamagoe K, Furuta J, Shioya A, et al. A case of vitiligo vulgaris showing a pronounced improvement after treatment for myasthenia gravis. BMJ Case Rep 2009;2009:bcr07.2009.2091. [Crossref] [PubMed]
- O'Sullivan SS, Mullins GM, Neligan A, et al. Acquired generalised neuromyotonia, cutaneous lupus erythematosus and alopecia areata in a patient with myasthenia gravis. Clin Neurol Neurosurg 2007;109:374-5. [Crossref] [PubMed]
- Mangla A, Hamad H. Pure Red Cell Aplasia. StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2020.
- Moriyama S, Yano M, Haneda H, et al. Pure red cell aplasia associated with thymoma: a report of a single-center experience. J Thorac Dis 2018;10:5066-72. [Crossref] [PubMed]
- Balasubramanian SK, Sadaps M, Thota S, et al. Rational management approach to pure red cell aplasia. Haematologica 2018;103:221-30. [Crossref] [PubMed]
- Chiatamone Ranieri S, Trasarti S, Arleo MA, et al. Aplastic Anemia and Good Syndrome in a Heavily Treated Stage IV Thymoma Patient: A Case Report and Review of the Literature. Case Rep Hematol 2019;2019:1910923. [Crossref] [PubMed]
- Suzuki K, Inomata M, Shiraishi S, et al. Thymoma with autoimmune hemolytic anemia. Case Rep Oncol 2014;7:764-8. [Crossref] [PubMed]
- Hashizume T. Good's syndrome and pernicious anemia. Intern Med 2002;41:1062-4. [Crossref] [PubMed]
- Gendron N, Sicre de Fontbrune F, Guyard A, et al. Aplastic anemia related to thymoma: a survey on behalf of the French reference center of aplastic anemia and review of literature. Haematologica 2020;105:e333-6. [Crossref] [PubMed]
- Palmieri G, Selleri C, Montella L, et al. Thymoma followed by paroxysmal nocturnal hemoglobinuria: a unique clinical association in the context of multiorgan autoimmunity with a potential role for CD8+ T lymphocytes. Am J Hematol 2006;81:774-8. [Crossref] [PubMed]
- Akinosoglou K, Melachrinou M, Siagris D, et al. Good's syndrome and pure white cell aplasia complicated by cryptococcus infection: A case report and review of the literature. J Clin Immunol 2014;34:283-8. [Crossref] [PubMed]
- Uy K, Levin E, Mroz P, et al. A Rare Complication of Thymoma: Pure White Cell Aplasia in Good's Syndrome. Case Rep Hematol 2019;2019:1024670. [Crossref] [PubMed]
- Kobayashi Y, Ando K, Hata T, et al. Complete remission of pure white cell aplasia associated with thymoma after thymectomy and cyclosporine administration. Int J Hematol 2019;109:346-50. [Crossref] [PubMed]
- Tamburello A, Castelnovo L, Faggioli P, et al. Good's syndrome, a rare form of acquired immunodeficiency associated with thymomas. Clin Pract 2019;9:1112. [Crossref] [PubMed]
- Tabata R, Tabata C, Yamamoto N, et al. Progressive peripheral CD8(+) T lymphocytosis complicated by pure red cell aplasia following immunosuppressive therapy for thymoma-associated myasthenia gravis. Int Immunopharmacol 2018;63:14-8. [Crossref] [PubMed]
- Gay CM, William WN Jr, Wang SA, et al. Thymoma complicated by acquired amegakaryocytic thrombocytopenia and pure red cell aplasia. J Natl Compr Canc Netw 2014;12:1505-9. [Crossref] [PubMed]
- Dahal S, Sharma E, Dahal S, et al. Acquired Amegakaryocytic Thrombocytopenia and Pure Red Cell Aplasia in Thymoma. Case Rep Hematol 2018;2018:5034741. [Crossref] [PubMed]
- Simkins A, Maiti A, Short NJ, et al. Acquired amegakaryocytic thrombocytopenia and red cell aplasia in a patient with thymoma progressing to aplastic anemia successfully treated with allogenic stem cell transplantation. Hematol Oncol Stem Cell Ther 2019;12:115-8. [Crossref] [PubMed]
- Yamamoto M, Iguchi G, Bando H, et al. Autoimmune pituitary disease: New concepts with clinical implications. Endocr Rev 2020;41:bnz003. [Crossref] [PubMed]
- Kubiszewska J, Szyluk B, Szczudlik P, et al. Prevalence and impact of autoimmune thyroid disease on myasthenia gravis course. Brain Behav 2016;6:e00537. [Crossref] [PubMed]
- Sobieszczańska M, Tubek S, Spychala S. Good's syndrome and hypoparathyroidism combined with hypocalcaemia, hypokalemia, hypomagnesemia, and hypophosphatemia-Case report. Immunol Lett 2016;172:132-3. [Crossref] [PubMed]
- Suzuki T, Suzuki S, Kitami A, et al. A thymoma associated with hyperparathyroidism. Thorac Cardiovasc Surg 1997;45:211-2. [Crossref] [PubMed]
- Byrne DJ, Gunn A, Davidson DL, et al. Parathyroid hyperplasia associated with thymoma. Postgrad Med J 1989;65:310-1. [Crossref] [PubMed]
- Bhandari S, Kumar R, Tripathi P, et al. Outcomes of hypercalcemia of malignancy in patients with solid cancer: a national inpatient analysis. Med Oncol 2019;36:90. [Crossref] [PubMed]
- Kumar N, Kumar R, Bera A, et al. Thymoma: clinical experience from a tertiary care institute from North India. J Cancer Res Ther 2013;9:235-9. [Crossref] [PubMed]
- Seker M, Gozu HI, Oven Ustaalioglu BB, et al. Myasthenia gravis and autoimmune Addison disease in a patient with thymoma. Clin Lung Cancer 2009;10:367-70. [Crossref] [PubMed]
- Donadio AC, Dragnev KH, Schwartz GK. Thymoma associated with syndrome of inappropriate antidiuretic hormone secretion and myasthenia gravis. South Med J 1998;91:278-9. [Crossref] [PubMed]
- Dupond JL, Essalmi L, Gil H, et al. Rituximab treatment of stiff-person syndrome in a patient with thymoma, diabetes mellitus and autoimmune thyroiditis. J Clin Neurosci 2010;17:389-91. [Crossref] [PubMed]
- Zou L, Xiong Z, Dun Y, et al. A case of rheumatoid arthritis associated with Hashimoto's thyroiditis and thymoma. Int J Rheum Dis 2017;20:1792-3. [Crossref] [PubMed]
- Miskovic R, Plavsic A, Peric-Popadic A, et al. Systemic Lupus Erythematosus and Secondary Antiphospholipid Syndrome after Thymectomy for Myasthenia Gravis - A Case Report. Open Access Maced J Med Sci 2015;3:439-42. [Crossref] [PubMed]
- Ben-Shahar M, Rosenblatt E, Green J, et al. Malignant thymoma associated with progressive systemic sclerosis. Am J Med Sci 1987;294:262-7. [Crossref] [PubMed]
- Tsai Y, Lin Y, Chen C, et al. Thymoma associated with myasthenia gravis and Sjogren syndrome. West Indian Med J 2013;62:264-5. [Crossref] [PubMed]
- Rudha Y, Starobinska E, Abdulqader Y, et al. Multicentric reticulohistiocytosis associated with thymic carcinoma. Rheumatology (Oxford) 2017;56:1706. [Crossref] [PubMed]
- Athanassiou P, Ioakimidis D, Weston J, et al. Type 1 cryoglobulinaemia associated with a thymic tumour: successful treatment with plasma exchange. Br J Rheumatol 1995;34:285-9. [Crossref] [PubMed]
- Nomura T, Kawasaki T, Tanabe T, et al. Ectopic cystic thymoma associated with Raynaud's phenomenon. Ann Thorac Cardiovasc Surg 2007;13:118-21. [PubMed]
- Liu T, Cai B, Feng R. Churg-Strauss syndrome presented as paraneoplastic syndrome with thymic neuroendocrine carcinoma: a case report. Rheumatol Int 2012;32:3683-5. [Crossref] [PubMed]
- Onishi A, Tanaka Y, Morinobu A. Spontaneous remission in large-vessel vasculitis: Takayasu arteritis and paraneoplastic disorder associated with thymic carcinoma. Scand J Rheumatol 2019;48:79-81. [Crossref] [PubMed]
- Rini BI, Gajewski TF. Polymyositis with respiratory muscle weakness requiring mechanical ventilation in a patient with metastatic thymoma treated with octreotide. Ann Oncol 1999;10:973-9. [Crossref] [PubMed]
- Kelly RJ, Browne SK, Rajan A, et al. Thymoma-associated paraneoplastic polymyositis. J Clin Oncol 2010;28:e378. [Crossref] [PubMed]
- Iacovelli R, Palazzo A, Conte D, et al. Dermatomyositis as first clinical appearance for a thymic epidermoid cell carcinoma. Acta Biomed 2010;81:68-71. [PubMed]
- Noël N, Le Roy A, Hot A, et al. Systemic lupus erythematosus associated with thymoma: A fifteen-year observational study in France. Autoimmun Rev 2020;19:102464. [Crossref] [PubMed]
- Hanafusa T, Azukizawa H, Kitaba S, et al. Diminished regulatory T cells in cutaneous lesions of thymoma-associated multi-organ autoimmunity: a newly described paraneoplastic autoimmune disorder with fatal clinical course. Clin Exp Immunol 2011;166:164-70. [Crossref] [PubMed]
- Hung CT, Tsai TF, Chen JS, et al. Thymoma-associated multiorgan autoimmunity. BMJ Case Rep 2019;12:e229163. [Crossref] [PubMed]
- Muramatsu K, Fujita Y, Inokuma D, et al. Cutaneous Manifestations of Thymoma-associated Multi-organ Autoimmunity: A Fatal Sign. Acta Derm Venereol 2016;96:818-9. [PubMed]
- Motoishi M, Okamoto K, Kaku R, et al. Thymoma-Associated Graft-Versus-Host-Like Disease With Skin Manifestations Improved by Complete Resection of Thymoma. Ann Thorac Surg 2015;100:1078-80. [Crossref] [PubMed]
- Gong L, Zhang P, Liu XY, et al. A rare thymoma case with seven paraneoplastic syndromes. Int J Clin Exp Med 2015;8:19517-23. [PubMed]
- Wolfe GI, Kaminski HJ, Aban IB, et al. Randomized Trial of Thymectomy in Myasthenia Gravis. N Engl J Med 2016;375:511-22. [Crossref] [PubMed]
- Comacchio GM, Marulli G, Mammana M, et al. Surgical Decision Making: Thymoma and Myasthenia Gravis. Thorac Surg Clin 2019;29:203-13. [Crossref] [PubMed]
- Marulli G, Schiavon M, Perissinotto E, et al. Surgical and neurologic outcomes after robotic thymectomy in 100 consecutive patients with myasthenia gravis. J Thorac Cardiovasc Surg 2013;145:730-5; discussion 735-6. [Crossref] [PubMed]
- Jaretzki A 3rd. Thymectomy for myasthenia gravis: analysis of controversies--patient management. Neurologist 2003;9:77-92. [Crossref] [PubMed]
- Daniel VC, Wright CD. Extended transsternal thymectomy. Thorac Surg Clin 2010;20:245-52. [Crossref] [PubMed]
- Maurizi G, D'Andrilli A, Sommella L, et al. Transsternal thymectomy. Thorac Cardiovasc Surg 2015;63:178-86. [PubMed]
- Aydin Y, Ulas AB, Mutlu V, et al. Thymectomy in Myasthenia Gravis. Eurasian J Med 2017;49:48-52. [Crossref] [PubMed]
- Friedant AJ, Handorf EA, Su S, et al. Minimally Invasive versus Open Thymectomy for Thymic Malignancies: Systematic Review and Meta-Analysis. J Thorac Oncol 2016;11:30-8. [Crossref] [PubMed]
- Wightman SC, Shrager JB. Non-Myasthenia Gravis Immune Syndromes and the Thymus: Is There a Role for Thymectomy? Thorac Surg Clin 2019;29:215-25. [Crossref] [PubMed]
- Fiorelli A, Natale G, Freda C, et al. Is thymomectomy equivalent to complete thymectomy in non-myasthenic patients with early-stage thymoma? Interact Cardiovasc Thorac Surg 2019;28:399-403. [Crossref] [PubMed]
- Li F, Tao Y, Bauer G, et al. Unraveling the role of ectopic thymic tissue in patients undergoing thymectomy for myasthenia gravis. J Thorac Dis 2019;11:4039-48. [Crossref] [PubMed]
- Geng Y, Zhang H, Wang Y. Risk factors of myasthenia crisis after thymectomy among myasthenia gravis patients: A meta-analysis. Medicine (Baltimore) 2020;99:e18622. [Crossref] [PubMed]
- Cata JP, Lasala JD, Williams W, et al. Myasthenia Gravis and Thymoma Surgery: A Clinical Update for the Cardiothoracic Anesthesiologist. J Cardiothorac Vasc Anesth 2019;33:2537-45. [Crossref] [PubMed]
- Berghmans T, Durieux V, Holbrechts S, et al. Systemic treatments for thymoma and thymic carcinoma: A systematic review. Lung Cancer 2018;126:25-31. [Crossref] [PubMed]
- Rouquette I, Taranchon-Clermont E, Gilhodes J, et al. Immune biomarkers in thymic epithelial tumors: expression patterns, prognostic value and comparison of diagnostic tests for PD-L1. Biomark Res 2019;7:28. [Crossref] [PubMed]
- Cho J, Kim HS, Ku BM, et al. Pembrolizumab for Patients With Refractory or Relapsed Thymic Epithelial Tumor: An Open-Label Phase II Trial. J Clin Oncol 2019;37:2162-70. [Crossref] [PubMed]
- Rajan A, Heery CR, Thomas A, et al. Efficacy and tolerability of anti-programmed death-ligand 1 (PD-L1) antibody (Avelumab) treatment in advanced thymoma. J Immunother Cancer 2019;7:269. [Crossref] [PubMed]
- Hann CL, Scherpereel A, Hellyer JA, et al. Role of Immunotherapy in Small Cell Lung Cancer, Thymic Epithelial Tumors, and Mesothelioma. Am Soc Clin Oncol Educ Book 2019;39:543-52. [Crossref] [PubMed]
- Zhao C, Rajan A. Immune checkpoint inhibitors for treatment of thymic epithelial tumors: how to maximize benefit and optimize risk? Mediastinum 2019;3:35. [Crossref] [PubMed]


