
Response letter: treatment of patent ductus arteriosus when pharmacologic or conservative approaches fail—a never-ending story
The development of neonatology that has taken place in the recent years has significantly increased the survival rate of even extremely premature newborns delivered as early as in the 22nd week of pregnancy with a birth weight not exceeding 500 grams. Unfortunately, prematurity is the most potent factor that have impact on the prevalence of patent ductus arteriosus (PDA). Children with PDA who fail to respond to conservative or pharmacological treatment require mechanical closure; however, the choice of optimal invasive strategy still remains the hot topic of neonatology and pediatric cardiac surgery.
We would like to thank Fraisse and colleagues (1) for their interest in our investigation of thoracoscopic clipping of PDA in all aged children and for their knowledgeable comments on our paper. Professor Fraisse raised the problem of the long learning curve and limited number of cases. The mentioned procedure should be limited only to a few centers to ensure adequate volume of patients and to provide proficiency in VATS procedure. It is worth mentioning that our center is the only one in Poland where VATS is the primary approach to surgical PDA closure in children. Thus, we do operate on children from the whole country and it this fact can explain the relatively large group of patients. Of note, all VATS-PDA closures in our department were performed by the same surgical team that consisted of two cardiac surgeons with skills in thoracoscopic surgeries and traditional closure of PDA with posterolateral thoracotomy (2).
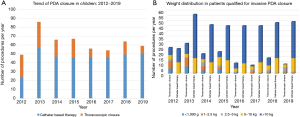
In his editorial letter, Prof. Fraisse noted the potential concerns with the patient selection for thoracoscopic PDA closure in our study. Current knowledge regarding the outcomes of transcatheter and thoracoscopic PDA closure is very limited; therefore, we still do not have the clear recommendations regarding the most optimal procedures to undertake when non-invasive methods fail. Two meta-analyses done by Lam et al. (3) and by Wang et al. (4) presented comparable results after transcatheter and surgical PDA closure. Both groups suggest a higher rate of residual shunts and longer length of stay after catheter-based therapy. However, both studies have serious limitations. They analyze data from two decades ago, which obviously do not reflect the current practice in pediatric surgery and interventional cardiology. Furthermore, both meta-analyses included patients treated with a variety of transcatheter devices and different surgical methods. Liem et al. (5) published the first randomized clinical trial, which compared VATS and transcatheter PDA closure. The authors reported a shorter operative time (32±12 vs. 20±3 min, P<0.001) and longer hospital stay after VATS. Chen et al. (6) in 2011 in a retrospective analysis of 294 children with PDA treated using thoracoscopic surgery (n=196) or transcatheter Amplatzer occlusion (n=98) reported neither early mortality nor cardiac-related deaths during the long-term follow-up period in both groups. There is not a single publication that suggests that either method provides lower early or long-term mortality. Although, we observe a trend that favors the conservative treatment over the catheter-based therapy (7). This can also be found in our patients where a decreasing number of preterm infants were qualified for VATS-PDA closure (see Figure 1A). The medical and technological progress has enable to perform the transcatheter PDA closure even in babies below 1,000 grams (8). Sathanandam et al. (9) studied 80 preterm infants born <27 weeks, weighing <100 grams at birth and <2,000 grams during transcatheter PDA closure and they could boast excellent results. They have modified their technique choosing vein access with transthoracic echocardiography guidance to avoid the arterial approach, what could result in acute arterial injury and limb loss (9).
Of note, the treatment strategy is the decision of the Pediatric Heart Team, consisting of pediatrician, neonatologist, cardiac surgeon, cardiologist and anesthesiologist. Every time, the current state of knowledge, therapeutic options, surgical results are first presented to the parents and the final decision is always made together with them. Patients with large ductal diameter, very small weight, presenting infection, subjects in a bad preprocedural clinical condition and with calcification of the duct were definitely excluded from transcatheter therapy. Thoracoscopic surgery was also the favored method of PDA closure in children <5 kg (2,10). All thoracoscopic procedures were performed as primary intervention. Since a few years ago, we have started offering the transcatheter method also for smaller babies, including preterm infants in our region; however, transcatheter therapy seems to be sill reserved for children heavier than 5 kg (Figure 1B). Due to the development of our pediatric invasive cardiology, probably a part of our VATS patients would be currently qualified for catheter-based intervention.
In summary, the thoracoscopic PDA closure should be performed only in the selected centers with VATS and surgical closure experience to minimize the effect of the learning curve. The development of transcatheter devices allows to operate even on preterm infants with extremely low birth weight. However, the current evidences are not enough to favor any method. The decision should always be based on the center's experience, Pediatric Heart Team statement and parents’ wish. A large multicenter prospective study comparing transcatheter and thoracoscopic is urgently needed to end this dispute and to finally create clear guidelines for PDA closure management in children.
Acknowledgments
Funding: None.
Footnote
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/ jtd-20-1802). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Fraisse A, Michielon G, Kempny A. What is the role of video-assisted thoracoscopy for patent ductus arteriosus ligation in the era of transcatheter closure? J Thorac Dis 2019;11:4090-1. [Crossref] [PubMed]
- Stankowski T, Aboul-Hassan SS, Seifi-Zinab F, et al. Descriptive review of patent ductus arteriosus ligation by video-assisted thoracoscopy in pediatric population: 7-year experience. J Thorac Dis 2019;11:2555-63. [Crossref] [PubMed]
- Lam JY, Lopushinsky SR, Ma IWY, et al. Treatment Options for Pediatric Patent Ductus Arteriosus: Systematic Review and Meta-analysis. Chest 2015;148:784-93. [Crossref] [PubMed]
- Wang K, Pan X, Tang Q, et al. Catheterization therapy vs surgical closure in pediatric patients with patent ductus arteriosus: a meta-analysis. Clin Cardiol 2014;37:188-94. [Crossref] [PubMed]
- Liem NT, Tung CV, Van Linh N, et al. Outcomes of thoracoscopic clipping versus transcatheter occlusion of patent ductus arteriosus: randomized clinical trial. J Pediatr Surg 2014;49:363-6. [Crossref] [PubMed]
- Chen H, Weng G, Chen Z, et al. Comparison of long-term clinical outcomes and costs between video-assisted thoracoscopic surgery and transcatheter amplatzer occlusion of the patent ductus arteriosus. Pediatr Cardiol 2012;33:316-21. [Crossref] [PubMed]
- O'Byrne ML, Millenson ME, Grady CB, et al. Trends in transcatheter and operative closure of patent ductus arteriosus in neonatal intensive care units: Analysis of data from the Pediatric Health Information Systems Database. Am Heart J 2019;217:121-30. [Crossref] [PubMed]
- Regan W, Benbrik N, Sharma SR, et al. Improved ventilation in premature babies after transcatheter versus surgical closure of patent ductus arteriosus. Int J Cardiol 2020;311:22-7. [Crossref] [PubMed]
- Sathanandam S, Balduf K, Chilakala S, et al. Role of Transcatheter patent ductus arteriosus closure in extremely low birth weight infants. Catheter Cardiovasc Interv 2019;93:89-96. [Crossref] [PubMed]
- Stankowski T, Aboul-Hassan SS, Fritzsche D, et al. Surgical closure of patent ductus arteriosus in extremely low birth weight infants weighing less than 750 grams. Kardiol Pol 2018;76:750-4. [Crossref] [PubMed]


