Flexible bronchoscopic excision of a tracheal mass under extracorporeal membrane oxygenation
Introduction
Tracheal tumor is a rare but life-threatening condition due to obstruction of the airway (1). Management of a tracheal tumor is very challenging and includes surgical resection, radiotherapy, and therapeutic bronchoscopy (2-4). Herein, we present a very rare case of an 88-year-old female patient with a tracheal mass due to direct invasion of a mediastinal teratoma. We successfully resected the tracheal mass with flexible bronchoscopic electrocautery under extracorporeal membrane oxygenation (ECMO) without any complications.
Case presentation
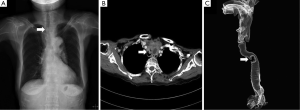
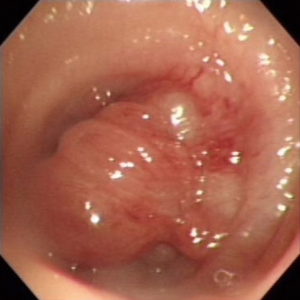
An 88-year-old woman presented to our hospital with a 3-month history of dyspnea at rest and a productive cough. The patient was bedridden for several days before admission. Upon admission, physical exams revealed wheezing during respiration, and routine laboratory studies were all non-specific. Chest X-ray and chest CT revealed an enhancing mass, about 5.0 cm × 3.9 cm, in the upper anterior mediastinum and a nodular lesion in the trachea, about 1.1 cm × 0.7 cm, suggesting invasion of the mediastinal mass causing near total obliteration of the tracheal lumen. Furthermore, there was severe tracheal curvature and deviation to the right side due to the mediastinal mass (Figure 1). Flexible bronchoscopy revealed a polypoid mass, measuring about 1.5 cm in diameter and obliterating nearly the entire lumen of the trachea. The mass was located about 3 cm below the vocal cords and resulted in severe deviation and curvature of the trachea (Figure 2). We could not access the tissue for pathological confirmation or perform further manipulation because the patient tolerated the procedure poorly. We decided on an emergent salvage operation for the tracheal mass through bronchoscopic intervention because the mediastinal mass invading the trachea and other major vessels were thought to be inoperable. Due to the patient’s condition, the operation had to be performed with a secure airway and general anesthesia. ECMO was set up before the induction of general anesthesia due to risk of ventilation failure after induction of general anesthesia and airway obstruction due to bleeding. Resection of the trachea or tracheal mass and placement of tracheostomy or endotracheal intubation for secure airway were deemed to be impossible. Heparin 400 IU was injected and cannulation was performed by means of bilateral femoral veins (17 Fr on the right side for inflow, 21 Fr on the left side for outflow) under local anesthesia. The induction of general anesthesia was initiated with a laryngeal mask, and the patient tolerated it well. ECMO was then gently started. Because the severe deviation and curvature of the trachea and the characteristics of the mass (location and near total obliteration of lumen) were thought to preclude the rigid bronchoscopic procedure, we performed the procedure with a flexible bronchoscope. However, rigid bronchoscope was set up in order to cope with possible emergent situations, such as major bleeding, tracheal perforation, and tracheal collapse during the procedure.
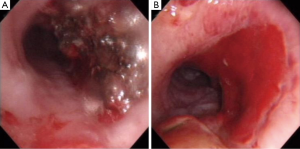
An 8.5-mm endotracheal tube was placed just above the tracheal mass under guidance with flexible bronchoscopy (Olympus, BF-1T260: an external diameter of 6.0 mm and a 2.8-mm working channel) in order to use the channel for other bronchoscopic instruments during manipulation of the tracheal mass. An electrocautery probe was passed through the working channel of the bronchoscope and placed at the tumor. During the procedure, a suction probe and a grasper were delivered though the endotracheal tube outside the bronchoscope. The resected mass was removed with the grasper, and the mass attached to the electrocautery probe was removed simultaneously with withdrawal of the bronchoscope. The mass easily bled with touching; however, it was resected without difficulty by using cauterization. Postoperative bronchoscopy showed the tumor was nearly completely resected (Figure 3). After resection of the mass, a 7-mm endotracheal tube was placed, and mechanical ventilation was initiated. The patient was weaned successfully from ECMO in the operating room. Total ECMO time was 140 minutes. The whole procedure was uneventful, and the patient was weaned from mechanical ventilation on the first postoperative day. Dyspnea at resting and wheezing resolved after weaning off of mechanical ventilation, and the patient was weaned off supplemental oxygen on the second postoperative day. The patient was discharged without supplemental oxygen on the eighth postoperative day. The final pathology findings revealed that the trachea mass resulted from direct invasion of the malignant teratoma.
Discussion
The management of a tracheal tumor depends on the characteristics of the tumor (size, location, pathology, degree of obstruction) and the patients’ general condition (1,2). In the present case, we devised a new method of resecting a tracheal mass because we could not perform tracheostomy or place endotracheal intubation to secure the airway due to the mediastinal and the tracheal masses.
Rigid bronchoscopy is usually recommended for the management of tracheal tumors (3-6). Rigid bronchoscopic procedures are known to have several benefits, including simultaneous inspection and management of lesions (3-6). In addition, they make the maintenance of adequate ventilation and oxygenation possible through the side port during the procedure (5,6). It is less invasive and risky than ECMO or tracheostomy (5,6). The role of rigid bronchoscopic intervention may be palliative, or in some cases may serve as a “bridge” to spare time for curative therapies (6). Despite these benefits, distal dislodgement of a tracheal tumor during the procedure is possible, and rigid bronchoscopy itself may lead to severe desaturation, tracheal wall penetration, or laryngeal edema and bronchospasm (3-6). Limitations of the rigid bronchoscope include inability to observe or treat lesions beyond the mainstem bronchus and patient-specific conditions such as inability to hyperextend neck or open mouth wide due to disease or trauma (3-6). High-frequency jet ventilation is a traditional method for securing an airway during rigid bronchoscopy (4); however, complete tracheal obstruction has been known to be a contraindication for jet ventilation because of inadequate outflow from the lungs (4).
In the present case, the severe curvature and deviation of the trachea, the characteristics of the mass, and the risk of ventilation failure during the procedure or after induction of general anesthesia precluded rigid bronchoscopic procedure. Similarly, flexible bronchoscopy was not a good option because of its blocking effect within the endotracheal tube which can inhibit adequate ventilation and its smaller working channel which may endanger the patient, especially during emergency situations (3,5). Therefore, ECMO was established before the procedure to support adequate ventilation and oxygenation. Flexible bronchoscopic manipulation with an electrocautery probe and other endoscopic instruments (grasper, suction probe) through another channel enabled the procedure to be performed safely and completely. However, rigid bronchoscope was set up in order to cope with possible emergent situations, such as major bleeding, tracheal perforation, and tracheal collapse.
Many studies have suggested that bronchoscopic manipulation with an electrocautery probe is available in most hospitals, and this technique, which has the ability to use electrocautery for rapid palliation and immediate tumor debulking, can be used quite readily (2,6). Furthermore, the energy delivery of electrocautery is superficial, with a minimal risk of perforation (7).
The role of ECMO in management of critical airway obstruction, including its use with interventional bronchoscopy has been previously reported (8-10). The use of ECMO provides secure ventilation and oxygenation, allowing management of the critical tracheal tumor through flexible or rigid bronchoscopy without necessity of cocurrent ventilation though the trachea (8,9). In addition, ECMO has been known as a useful means of cardiopulmonary support in critical patients for nonconventional indications such as tracheal surgery, pulmonary artery embolism, and tumorous airway obstruction (10). Limitations associated with ECMO include high cost, bleeding caused by heparin, thromboembolism, vascular injury caused by cannulation, and ischemia of the limb distal to an arterial cannula (10). Placing an endotracheal tube under bronchoscopic guidance allows other endoscopic instruments (grasper, suction probe) to be available for bleeding control and tumor resection.
In summary, tracheal obliteration by a tracheal mass is a life-threatening condition, and the management is very challenging. When the management of a difficult airway and tracheal mass by conventional methods is impossible, our technique in the present case was shown to be very useful.
Acknowledgements
Disclosure: The authors declare no conflict of interest.
References
- Wu CC, Shepard JA. Tracheal and airway neoplasms. Semin Roentgenol 2013;48:354-64. [PubMed]
- Beamis JF Jr. Interventional pulmonology techniques for treating malignant large airway obstruction: an update. Curr Opin Pulm Med 2005;11:292-5. [PubMed]
- Bolliger CT, Sutedja TG, Strausz J, et al. Therapeutic bronchoscopy with immediate effect: laser, electrocautery, argon plasma coagulation and stents. Eur Respir J 2006;27:1258-71. [PubMed]
- Brodsky JB. Bronchoscopic procedures for central airway obstruction. J Cardiothorac Vasc Anesth 2003;17:638-46. [PubMed]
- Gorden JA, Ernst A. Endoscopic management of central airway obstruction. Semin Thorac Cardiovasc Surg 2009;21:263-73. [PubMed]
- Jeon K, Kim H, Yu CM, et al. Rigid bronchoscopic intervention in patients with respiratory failure caused by malignant central airway obstruction. J Thorac Oncol 2006;1:319-23. [PubMed]
- Kennedy MP, Morice RC, Jimenez CA, et al. Treatment of bronchial airway obstruction using a rotating tip microdebrider: a case report. J Cardiothorac Surg 2007;2:16. [PubMed]
- Lang G, Taghavi S, Aigner C, et al. Extracorporeal membrane oxygenation support for resection of locally advanced thoracic tumors. Ann Thorac Surg 2011;92:264-70. [PubMed]
- Vaporciyan AA, Rice D, Correa AM, et al. Resection of advanced thoracic malignancies requiring cardiopulmonary bypass. Eur J Cardiothorac Surg 2002;22:47-52. [PubMed]
- Hong Y, Jo KW, Lyu J, et al. Use of venovenous extracorporeal membrane oxygenation in central airway obstruction to facilitate interventions leading to definitive airway security. J Crit Care 2013;28:669-74. [PubMed]


