Benign esophago-pulmonary fistula complicating achalasia: case report and literature review
Introduction
Fistula between esophagus and airway is not uncommon, it always derives from congenital abnormality, traumatic injury, neoplastic tumor invasion, foreign body erosion or iatrogenic injury (1,2). Rarely, the esophago-respiratory fistula appeared in diverticulitis patient who commonly presented with middle thoracic diverticulas (3-6). However, the achalasia, another common benign disease of esophagus also plays an important role in this kind of fistula formation, which has not yet been well recognized. In previous studies, only four cases of English literature were reported about benign esophago-pulmonary fistula associated with achalasia, with the mechanism of fistula formation left being a mistery (7-10). Here, our case is the fifth one. After a simple review of these related cases, we summarize the features of those reported patients and discuss the possible mechanisms as well as the treatment strategies.
Case presentation
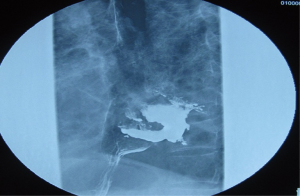
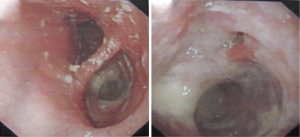
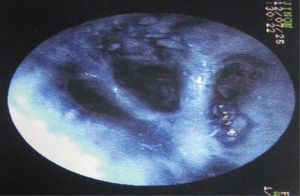
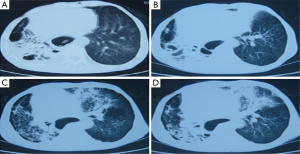
A 58-year-old male patient was admitted to our hospital for a long history of difficulty in swallowing for 15 years and chronic cough with dirty sputum for 3 years. He also complained of moderate shortness of breath and progressive loss of body-weight for 18 kg in the recent six months. He ever went to see a physician in local clinic with complicating of fever for several times and was being treated on the consideration of a recurrent pneumonia. But the discomforts did not relieve obviously after systematic anti-inflammation treatment. It was not until 7 days ago that the upper gastrointestinal radiography was performed, when an esophago-respiratory fistula was suspected and he was transferred to our center for surgical intervention. On admission, he showed severe malnutrition with body weight of only 41.5 kg and BMI of 16.6. His body temperature was 37.3 °C, with the heart rate of 100 per minute, respiratory rate of 24 per minute and blood pressure of 100/60 mmHg. Chest auscultation revealed a significant moist rales of the right lung and mind rales in the upper of the left lung. The chest CT scan showed diffuse lung tissue inflammatory destruction, which was obvious in the right lung, with over-dilation of the lower part of the thoracic esophagus (Figure 1). The esophagram presented with a leakage of barium into the right lower lobe after barium was swallowed, and showed a dilated lower esophagus and a smooth, tapered, distal narrowing at the gastroesophageal junction, which was referred to as “bird’s beak appearance” and was typical of achalasia (Figure 2). The upper endoscopy indicated that the large holes on the right wall of the lower esophagus with the cardia was narrowed (Figure 3). After it was irrigated through the holes, methylene blue was soon found in the right lower bronchus under bronchoscopy (Figure 4), which confirmed a fistula between esophagus and the right lower lobe. However, the repeated biopsies supported only benign fistula. The esophageal manometry also supported the existence of achalasia. Then, a benign esophago-pulmonary fistula secondary to achalasia was diagnosed. We performed Heller’s myotomy as well as fundoplication through trans-abdominal route and colon replacement of the esophagus through retro-sternal procedure, with the thoracic esophageal fistula as well as the right lung left being intact. The surgery was successful and he was discharged 15 days later after operation. He is going on well and has received more body weight of 10 kg.
Discussion
Esophago-pulmonary fistula is not rare in clinical practice. However, the achalasia-associated one seems to be rare. Although the relationship between achalasia and esophageal fistula formation is still not clear. In the literatures, aortic esophageal fistula, esophago-esophageal fistula, esophago-cardiac fistula, esophago-pericardial fistula, atrio-esophageal fistula and malignant esophago-pulmonary fistula were being reported in achalasia patients with fatal outcome (11-16), which have told us that achalasia could have served as a danger factor in esophageal fistula formation and needed to be investigated more. As one of the surrounding organs in limited space of the thoracic space, the pulmonary is unavoidable to be affected occasionally, with the achalasia-associated esophageal-respiratory fistula surely being possible.
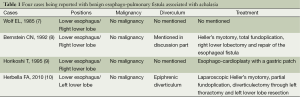
However, what are the links between achalasia and esophageal-pulmonary fistula? As it has been mentioned before, the achalasia-related fistula between digestive tract and respiratory tract usually occurred together with malignancy of the esophagus (16). Such condition is never difficult to be understood, for direct invasion is an inherent characteristic of the malignancy, which may promote the fistula formation. On the contrary, the benign fistula occurred in achalasia patient left to be a mystery. Does it was a coincidence or there is a mechanism? Historically, only four cases were reported with esophago-pulmonary fistula complicating achalasia in the absence of malignancy, which have been summarized in Table 1 (7-10). All of them occurred between lower esophagus and the lower lobe. Three of them presented leakages into the right lower-lobe (7-9), and one into the left (10). Of which, Herbella FA’s study presented with an epiphrenic diverticulum (10), and Bernstein CN’s study analyses a likely diverticulitis formation in the fistula development process (8). We agree with the same hypothesis that diverticulitis plays an important role in fistula formation. Two aspects described in literatures can support the idea. First, diverticulum, such as middle thoracic, traction or epiphrenic diverticula was often being watched resulting from motor disorder of the esophageal sphincter, such as achalasia, which are featured as an incomplete or absent relaxation of the lower esophageal sphincter and aperistalsis of the esophageal body, and easily leads to over-dilation of local esophageal followed by diverticula formation (8,17,18). Second, esophago-respiratory fistula due to fistulation with a diverticulum nearly all comprised middle thoracic, traction diverticula or epiphrenic diverticula (3-5,10). However, in our opinion, the inflammation may be the critical factor penetrating into the process from achalasia to diverticulum formation and then to fistulalization, and what deserved to be emphasized now is the diverticulitis, rather than diverticulum itself. Historically, there is also another case report describing an achalasia associated with esophageal diverticulitis leading to esophageal perforation and a walled off abscess (19), Although there was no esophageal pulmonary fistulalization. It still supports our idea.
Full table
On the treatment strategy, no consensus has been achieved yet for esophago-pulmonary fistula in achalasia patients. However, Heller’s myotomy as well as fundoplication seems to be necessary in most patients (7-10), even with or without repairment of esophagus fistula and damaged lung resection. Our case is of no exception. We performed the myotomy and fundoplication to alleviate the symptoms caused by achalasia. Except for the above, the additional surgical approach varied often in different patients with different conditions seen from the four cases reported before. For example, Bernstein CN’s study performed lower lobectomy as well as repair of the esophageal fistula (8). Horikoshi’s study only performed Esophago-cardioplasty with a gastric patch (9), while Herbella FA’s study have done a diverticulectomy as well as resection of left lower lobe (10). However, the common point is fistula repairment as well as resection of the damaged lung. Our case is different. The fistula size is too large to be repaired and the other pulmonary tissue except for the right lower lobe is also damaged severely with poorly pulmonary function allowed for radical resection. So we choose colon replacement of the esophagus instead, but left the thoracic esophageal fistula as well as the right lung being intact that also bring with the patient a well prognosis.
In conclusion, achalasia should be considered as one of the rare causes of benign esophago-pulmonary fistula formation. The possible mechanism may be the chronic inflammatory erosion with or without diverticulum. The common treatment strategy are myotomy and fundoplication, with fistula repairment as well as resection of the damaged lung. However, it often varies in different conditions.
Acknowledgements
Disclosure: The authors declare no conflict of interest.
References
- Balazs A, Galambos Z, Kupcsulik PK. Characteristics of esophagorespiratory fistulas resulting from esophageal cancers: a single-center study on 243 cases in a 20-year period. World J Surg 2009;33:994-1001. [PubMed]
- Deshpande G, Samarasam I, Banerjee S, et al. Benign esophagorespiratory fistula: a case series and a novel technique of definitive management. Dis Esophagus 2013;26:141-7. [PubMed]
- Stewart WR, Klassen KP, Horava AP. Esophagobronchial fistula due to esophageal traction diverticulum; review of literature and report of case. AMA Arch Surg 1958;76:317-21. [PubMed]
- Svane S. Oesophagobronchial fistula through a midoesophageal diverticulum associated with fatal pulmonary bleeding. Scand Cardiovasc J 1997;31:243-4. [PubMed]
- Minkari T. Benign transpulmonary esophagobronchial fistula associated with a traction diverticulum. J Int Coll Surg 1963;40:393-9. [PubMed]
- De Giacomo T, Francioni F, Venuta F, et al. Benign esophageal-respiratory fistulae. The surgical treatment and results of 10 cases. Minerva Chir 1993;48:311-6. [PubMed]
- Wolf EL, Frager D, Goldman MJ, et al. Achalasia complicated by esophagobronchial fistula. Am J Gastroenterol 1985;80:584-5. [PubMed]
- Bernstein CN, Snape WJ Jr. Achalasia and development of benign esophagobronchial fistula. Dig Dis Sci 1992;37:609-12. [PubMed]
- Horikoshi T, Horie T, Sekiguchi T, et al. Esophagocardioplasty for achalasia in closure of a complicated esophagobronchial fistula. Am J Gastroenterol 1995;90:1348-9. [PubMed]
- Herbella FA, Del Grande JC. Benign esophagopulmonary fistula through an epiphrenic diverticulum and asymptomatic achalasia. Dig Dis Sci 2010;55:1177-8. [PubMed]
- Macpherson DJ, Thompson WR. Aortic esophageal fistula secondary to achalasia accompanied by megaesophagus and esophageal ulceration. N Engl J Med 1958;259:1027. [PubMed]
- Knauer CM, McLaughlin WT, Mark JB. Esophago-esophageal fistula in a patient with achalasia. Gastroenterology 1970;58:223-8. [PubMed]
- Strong RW. Oesophago-cardiac fistula complicating achalasia. Postgrad Med J 1974;50:41-4. [PubMed]
- Breatnach E, Han SY. Pneumopericardium occurring as a complication of achalasia. Chest 1986;90:292-3. [PubMed]
- Achouh P, Pouly J, Azarine A, et al. Atrio-esophageal fistula complicating esophageal achalasia. Interact Cardiovasc Thorac Surg 2011;13:211-3. [PubMed]
- Frank MS, Brandt LJ, Haas K, et al. Malignant esophagopulmonary fistula complicating achalasia. Am J Gastroenterol 1979;71:206-9. [PubMed]
- Borrie J, Wilson RL. Oesophageal diverticula: principles of management and appraisal of classification. Thorax 1980;35:759-67. [PubMed]
- Debas HT, Payne WS, Cameron AJ, et al. Physiopathology of lower esophageal diverticulum and its implications for treatment. Surg Gynecol Obstet 1980;151:593-600. [PubMed]
- Case records of the Massachusetts General Hospital. Weekly clinicopathological exercises. Case 32-1982. A 65-year-old man with dysphagia and dilatation of the esophagus. N Engl J Med 1982;307:426-33. [PubMed]