
Prevalence of influenza and pneumococcal vaccination in chronic obstructive pulmonary disease patients in association with the occurrence of acute exacerbations
Introduction
Chronic obstructive pulmonary disease (COPD) can be described as a chronic inflammatory disease. It is associated with an irreversible airflow limitation and causes a progressive deterioration of pulmonary functions, accompanied by symptoms including regular sputum production, chronic cough, breathlessness and reduced physical activity (1). Patients have a higher risk for respiratory tract infection, therefore a growth in the frequency of acute exacerbations of the disease can be observed. As a consequence of acute exacerbations, morbidity and mortality increase (2). Although mostly rhinovirus causes exacerbations, influenza is also known as an important factor in triggering exacerbations of COPD that lead to hospitalization in most cases, and it can contribute, as a major factor, to mortality and morbidity in COPD (3). Based on the various mechanisms, an increased production of specific cell adhesion molecules and impaired mucociliary clearance can mediate the attachments of viruses and bacteria to the airway epithelium (4), and because of these processes, patients with COPD are more likely to develop influenza (5) and pneumococcal pneumonia (6).
Currently, the annual influenza vaccination of COPD patients is a top priority and pneumococcal vaccination is recommended in 5 years (7). Kopsaftis et al. reviewed six randomised controlled trials about the efficiency of influenza vaccination in patients with chronic bronchitis or COPD. The studies included 2,562 patients. Based on their reports, influenza vaccine reduced the number of exacerbations compared to placebo in patients with COPD (8).
Schembri et al. found association between influenza vaccination and a 41% reduction in the risk of all-cause mortality (9). Although most international consensus guidelines advocate vaccination, and the positive effects of vaccinating patients with COPD have been proven, a significant percentage of patients still remain unvaccinated (10). A considerable effect of multiple psychosocial factors and preexisting health beliefs must be taken into account in the decision to accept vaccination (11). A great opportunity was provided to explore the reasons behind the advancement of the “anti-vaccine movement” during the swine flu pandemic in 2009. They analyzed interviews with public criticizers of the pandemic flu vaccine, and identified several common motivating factors. These included concerns over safety stemming from the belief that the vaccine and its side effects had not been properly investigated, as seemingly the product was released onto the market in a short time, and the belief that pharmaceutical companies make a big impact on this process because of their financial interest. Another belief was that the vaccine may contain other “dangerous” ingredients, so by receiving the vaccine, their chance to develop other “serious diseases” may increase. The contrasting opinion was that pandemic influenza did not pose “a serious threat to the health of most individuals” meaning that the risks of vaccination outweighed those of influenza infection (12). Public health initiatives are necessary to emphasize the importance of influenza and pneumococcal vaccination, and to facilitate the increase of vaccination rates in this patient population. The purpose of this study was to determine the prevalence of influenza and pneumococcal vaccination in the population of COPD patients, and to investigate the effectiveness of vaccines in terms of reduction of the risk of severe, acute exacerbations of COPD.
Methods
Study design and population
The study involved 250 COPD patients hospitalized at the Pulmonary Rehabilitation Department. Inclusion criteria were age over 40 and the diagnosis of COPD based on the clinical feature and lung function (post-bronchodilation FEV1/FVC <70%). Patients were selected by simple randomized sampling according to the data of respiratory functions, comorbidities and anthropometric details, which had been retrieved from the electronic health record system. As relevant comorbidities, we included congestive heart failure, coronary artery disease, hypertension, malignancy, diabetes, osteoporosis, metabolic syndrome, anxiety, and mood disorder. The study was approved by the Ethical Committee of the National Koranyi Institute for Pulmonology, Budapest, Hungary, under the registration number of 25/2017. All patients enrolled completed the informed consent form. The study conformed to the provisions of the Declaration of Helsinki (as revised in 2013).
Collected characteristics
We collected the sociodemographic characteristics for each patient, including age, gender, alcohol consumption, smoking, years since their COPD diagnosis, treatments, the number and severity of COPD exacerbations, and the history of 23 pneumococcal and influenza vaccination cases (seasons 2017–2018). In our questionnaire, we asked the patients’ opinion about vaccination and whether they have been informed about the pathogens and vaccines by their physician. COPD exacerbation was defined as a significant change of the patient’s initial symptoms (dyspnea, cough, sputum production), or if at least two of the following four symptoms exist (Anthonisen criteria): (I) an increase in purulent sputum, (II) deterioration in lung function, worsening of respiratory complaints, (III) fever, or (IV) leukocytosis. In the case of moderate exacerbation, the prescription of an antibiotic or systemic corticosteroid was required, while the definition of severe exacerbation when the patient had to be hospitalized for more than 24 hours, and received non-invasive or mechanical ventilation. Based on whether they had received influenza vaccination or not in the 2017–2018 campaign, patients were classified in two cohorts. Participants were also categorized into four groups according to their degree of bronchial obstruction, based on FEV1 data defined by the Global Initiative for Chronic Obstructive Lung Disease (GOLD) guidelines; mild: FEV1 ≥80%; moderate: 50% FEV1 <80%; severe: 30% FEV1 <50%; very severe: FEV1 <30% (GOLD stages 1–4). Body mass index (BMI) was used as the independent variable. It is calculated as weight divided by height squared (kg/m2). All participants were classified into four subgroups, underweight patients had a BMI under 18.5 (BMI <18.5), the BMI of average weight patients were between 18.5 and 25 (18.5≤ BMI <25), overweight participants had their BMI between 25 and 30 (25≤ BMI <30) and obese patients’ BMI values were over 30 (BMI ≥30). The categorization was based on the standard of World Health Organization (WHO).
Statistical analysis
Shapiro-Wilk test was used to confirm the quantitative variables normal distribution which was followed by Student’s t-test for comparisons. Chi-squared test was used for comparisons of the proportions of categorical and discrete variables. We estimated odds ratios (OR) using unconditional logistic regression with 95% confidence intervals (95% CIs). According to COPD severity (GOLD stages 1–2 versus GOLD stages 3–4), associations for a history of influenza and pneumococcal vaccination were stratified. Factors influencing vaccine uptake (age, gender, smoking status, comorbidities, and COPD GOLD stage) were analyzed by logistic regression. The study was registered in the ISRCTN registry with the ID ISRCTN13019180, and before the statistical analysis was performed, data were anonymised. A value of P<0.05 was accepted for significance.
Results
The prevalence of influenza and pneumococcal vaccination coverage with principal clinical and sociodemographic characteristics is presented in Table 1. In total, we examined the data of 250 patients with chronic obstructive pulmonary disease, the sample consisted of 109 male patients (43.6%) and 141 female patients (56.4%). The average age of the observed population was 66.62 years (±8.34), 67.30 (±8.54) years for men, 66.09 (±8.16) years for women. Seven point two percent (n=18) of the patients were non-smoking. The observed patients had been smoking an average of 19.9 cigarettes a day for 37.16 years. One third of them (30.4%) (n=76) are still active smokers. COPD had been diagnosed approximately 8 years ago on average, and they had taken inhaled medications for 7.7 years. Patients who had successfully quit smoking had smoked their last cigarette 5 years before the study was conducted, on average.

Full table
Four point eight percent (n=12) of the 250 patients were classified as GOLD I (mild) stage, 35.6% (n=89) as GOLD II (moderate) stage, 46.4% (n=116) as GOLD III (severe) stage and, 13.2% (n=33) as GOLD IV (very severe) stage. The average values of FEV1%pred, registered after bronchodilatation were GOLD I: 93.50%, GOLD II: 61.98%, GOLD III: 41.24%, GOLD IV: 20.11%.
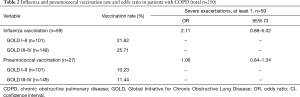
The vaccination rates were 23.6% for influenza, and 10.8% for pneumococcus, only 6% of patients received both vaccinations. The vaccination rate was higher for more severe forms of COPD in both vaccinations (Table 2). Influenza vaccination coverage was 26.6% in men and 21.2% in women, the pneumococcal vaccination rate was 13.7% in male patients and 8.5% in female patients, and the vaccination rate was higher in elderly patients, and in patients with comorbidities. Thirteen point two percent of smokers were vaccinated against influenza and 5.2% against pneumococcus. The influenza vaccination rate among non-smokers was 28.2%, and it was significantly different from the pneumococcal vaccination rate (13.2%) (P<0.05).
Full table
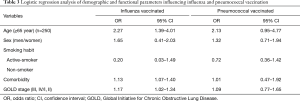
We found statistically significant association between influenza and pneumococcal vaccination and the reduced risk of severe exacerbations, influenza vaccination OR: 2.11 (95% CI: 0.88–5.02) and pneumococcal vaccination OR: 1.06 (95% CI: 0.84–1.34) were detected (Table 2) and patients (15/250) with both vaccination (influenza and pneumococcal vaccine) OR: 2.37 (95% CI: 1.39–4.08). Logistic regression analysis of demographic and functional parameters influencing influenza and pneumococcal uptake are in Table 3. It describes how more advanced age (≥65 years), the presence of comorbidities, and more severe COPD disease were related positively with both influenza and pneumococcal uptake, while the presence of active smoking was associated with lower influenza and pneumococcal vaccination rates (Table 3).
Full table
Only 28.4% (n=71) of the patients were informed by their physician about the necessity of vaccination because of their chronic illness. Thirty-six percent (n=90) of the patients found vaccination against influenza beneficial, while 26.0% (n=65) considered pneumococcal vaccination as useful. According to 31.2% (n=78) of the patients, the influenza virus causes only mild illness and 54.0% (n=135) of them had never heard about the Pneumococcus bacteria. Only 10.0% (n=25) of the observed patients had received treatment with bacterial lysate medicines (OM85-BV, Broncho-Vaxom), none of them had received other immunomodulators (Ribomunyl, Isoprinosine). Sixty-nine point six percent (n=174) of the patients had taken antibiotics in the preceding year, twice a year on average. Fifty-six point eight percent (n=142) of them received oral steroid cure, twice a year on average. Due to the deterioration of their condition, 36.8% (n=92) of the patients needed non-invasive or mechanical ventilation, twice a year on average.
Discussion
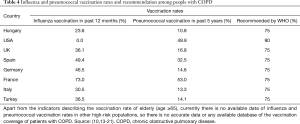
In our study, the influenza vaccination rate of the observed Hungarian COPD patients, aged 40 years or above was 23.6%, which is below the internationally targeted 75% set by the WHO. The pneumococcal vaccination rate was 10.8%. Studies from other countries reported similar conditions as well (Table 4). According to the UK primary care consultation database, the influenza vaccination coverage rate of the COPD patients in the country was 36.1% (13) and the PPV23 vaccination rate was 16.8% (14). The influenza vaccination rate was 30.5%, while the pneumococcal vaccination rate was 13.3% in Italy in an epidemiological study (15). The rates were 36.5% for influenza and 14.1% for pneumococcus in Turkey (16). A clinical study observed 46.5% influenza and 14.6% pneumococcal vaccination in Germany (17). Influenza and pneumococcal vaccination were higher in the elderly, more severe COPD population with comorbidities and who quit smoking in our research, which are similar to other previous studies (18,19).
Full table
Our findings have proven that influenza and pneumococcal vaccination is associated with a decreased risk of acute exacerbations among patients with COPD, including severe exacerbations requiring hospitalisation. Similar results were found by Garrastazu et al. Their retrospective cohort study included 899 COPD patients from Spain. They reported that in the year following immunization, influenza vaccination significantly reduced the risk of severe exacerbations requiring hospitalization [OR 0.54 (95% CI: 0.35–0.84)], a better effect was found in patients with more severe COPD (22). A randomized controlled trial (RCT), including 596 patients showed a significant efficacy of 76% (95% CI: 20–93%, P=0.013) of PPV23 against community-acquired pneumonia (CAP) in patients less than 65 years of age. It proved to be nearly significant at 48% (95% CI: 27–80%, P=0.076) in patients with severe airflow obstruction, and showed the best results when both characteristics were present (23).
Influenza and pneumococcal vaccination rates have been shown to be suboptimal among COPD patients in our study. Vandenbos et al. (24) found negative attitudes against influenza vaccinations and lack of recommendation from general practitioners or other doctors as main reasons for refusing. Patients do not believe in the effectiveness of vaccines, do not believe that they are exposed to this risk, and patients are also concerned about the undesirable side effects of vaccines in the study of Ciblak et al. (25).
The WHO also reports vaccine insecurity and non-vaccination among the top 10 threats to the world (20). Only one third (36.0%) of patients considered the influenza vaccine useful, while only a quarter (26.0%) thought that pneumococcal vaccine is beneficial, more than half of the patients (54.0%) had never heard of Pneumococcus bacteria in our present study in the Hungarian population similarly to other countries. In addition, in recent decades, anti-vax movements have taken root in many countries (26). Members of these movements most often live in developed countries, where the incidence of vaccine-preventable diseases is typically low. They spread their false and misleading information about the composition, side effects and harmful consequences of vaccines on a variety of Internet interfaces, social media sites and among themselves, causing great harm.
COPD patients are advised to receive influenza vaccination annually, but it is also recommended to other populations at risk, such as anybody over the age of 65, patients with chronic illnesses, health care workers, caregivers, or others at a higher risk of complications. Pneumococcal vaccination is recommended to everybody over 50, smokers (regardless of their age and comorbidities), patients under immunosuppresive therapy, patients with cochlear implants or cranial injury, to patients of any age with chronic diseases (such as diabetes, respiratory, renal, liver, heart diseases), and patients with asplenia, as they are more susceptible to severe pneumococcal infections (21,27).
A meta-analysis of influenza vaccination in the elderly (≥65 years) population found that respiratory disease was reduced by 56%, pneumonia by 53%, hospitalization by 50%, and all-cause mortality by up to 68% with vaccination at the time of an influenza pandemic. Most studies showed that vaccination is clearly effective (28), yet vaccination is very low. After 1 year of follow-up, RCT studies reported that influenza-vaccinated patients experienced significantly (P=0.005) reduced exacerbations and influenza-like illnesses (ILIs) compared to the non-vaccinated population (29).
About 40% of CAP requiring hospital admission in adults is caused by Streptococcus pneumoniae (pneumococcus) (30). In Europe, the incidence of CAP was dramatically higher in persons with severe COPD. In the general population, 1.07–1.2/1,000 person-years incidence was found, while the number of cases in the population of COPD patients were 20-fold higher (22.4/1,000 person-year) (30). Despite accessible and adequate antimicrobial therapy in the past 60 years, severe pneumococcal infections with bacteraemia are still responsible for approximately 12% of the mortality (31). In addition to the fact that usually pneumonia has a poor outcome for COPD patients, healthcare systems also have to deal with its serious consequences. With COPD patients, productivity costs and direct medical costs associated with hospitalization for CAP are twice as high as with patients with no comorbidities. Substantial benefits could be provided to patients and the society as well by preventing pneumonia in patients with COPD (32). The effectiveness of antibiotic therapy is limited, and as a result of antibiotic resistance, it is becoming more significant, while the number of individuals at a high risk of infection is increasing in the population. The importance of prevention must be emphasized based on these observations (33).
An analysis of COPD patients aged 55 or above showed that in vaccinated participants, the hazard ratio of acute coronary syndrome requiring hospitalization was significantly lower than in unvaccinated participants. Sung et al. also reported the relevance of repeating influenza vaccinations in the same patient across several study seasons, as it has a significant benefit (P<0.001) (34). PCV13 and seasonal influenza vaccine can be given at the same time, as the vaccines have no effect on each other, however, it provides us a good opportunity to avoid missed occasions for vaccination (35). Moreover, applying the two vaccines together have an additive effect in reducing the mortality due to influenza or pneumonia and the risk of hospitalization for pneumonia (36). Effective pneumococcal vaccination could also be of great help in reducing the need for antibiotic treatments, which is an important aspect, as the reduction of antibiotic treatments could result in a delay or prevention in the colonization of the lungs by antibiotic-resistant bacteria (37).
A single-centre study of 187 COPD patients admitted with an acute exacerbation (109 pre-intervention, 78 post-intervention) was performed by Bhatt et al. in Alabama, US. The aim of the study was to determine whether 30-day all-cause recurrence rates of COPD exacerbations and overall costs could be reduced by multimodal intervention. It included a rapid check-up in a COPD clinic in case of post-acute exacerbations, a pack of tutorials to educate patients, and regular follow-up phone calls by a practice nurse. The primary outcomes have not shown any differences in their study. However, the observed post-intervention influenza vaccination rates (31% vs. 51%, P=0.011) and pneumococcal vaccination rates (37% vs. 82%, P<0.001) were significantly increased. The results of their study suggest that greater patient engagement with evidence-based care including vaccination could be expected in case of an acute admission, due to an exacerbation of COPD, despite the study had the limitation of its small sample size. Furthermore, the conclusion of the study is that the greatest effect on vaccination rates could be achieved by combining clinician and patient-focused interventions, using multimodal intervention methods (38).
Based on research evidence, to optimize the care of COPD patients and to increase vaccination rates in high-risk populations, adopting a holistic approach may be more efficient, and so would be targeting several different aspects of care simultaneously. For instance, during smoking cessation, counseling vaccine recommendations and other aspects of evidence-based care should be highlighted as well (39). Patients who built trust with their physician are more likely accept and respect treatment recommendations, as trust is a key determinant of patient behaviour. Therefore, this factor must be kept in mind during vaccination consultations (40). Recent research has shown that focusing on cultivating “positive patient-doctor relationships based on listening and understanding” by applying a patient-centered, narrative medication method helps establish a good cooperation and can improve adherence to treatment recommendations in COPD patients (41,42). The importance of influenza vaccination cannot be stressed enough; annual immunization against influenza administered together with pneumococcal vaccination significantly decreases the number and severity of complications in older patients as well.
Limitations and strengths of the study
Several limitations of our study should be noted. First, sociodemographic variables, such as educational level and marital status were not available. Second, we could only conclude the association between influenza and pneumococcal vaccination and the risk of occurrence of acute exacerbation. Third, in our study, we applied GOLD I–IV classification, because data [modified Medical Research Council (mMRC) or COPD assessment test (CAT) results] necessary for the current GOLD A–D classification were not available. Despite the listed limitations, we have to mention the important strengths of the study. The association between influenza and pneumococcal vaccination and the risk of acute exacerbation of COPD patients at the Department of Pulmonary Rehabilitation of the National Koranyi Institute of Pulmonology, Budapest had not been reported before.
Conclusions
In conclusion, along with the available evidence, the findings of this study support the association between influenza and pneumococcal vaccination and the decreasing risk of COPD exacerbations in the following year. The overall prevalence of influenza and pneumococcal vaccination was under the optimal level, despite the evidence for its protective effect. Therefore, these high-risk patients are recommended to receive annual influenza vaccination, pneumococcal vaccination every 5 years and should be informed about their vaccination opportunities by their physician during their treatment. Older age, the presence of comorbidities, and more severe GOLD stages had a positive effect on the uptake of both influenza and pneumococcal vaccinations. Further large-scale prospective studies are required to analyse the effectiveness of influenza and pneumococcal vaccination in patients with COPD.
Acknowledgments
We would like to thank the National Koranyi Institute for Pulmonology for their support and practical help. We would like to thank Istvan Gaudi`s work in controlling the statistical analysis.
Funding: None.
Footnote
Data Sharing Statement: Available at http://dx.doi.org/10.21037/jtd-20-814
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/jtd-20-814). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was approved by the Ethical Committee of the National Koranyi Institute for Pulmonology, Budapest, Hungary, under the registration number of 25/2017. All patients enrolled completed the informed consent form. The study conformed to the provisions of the Declaration of Helsinki (as revised in 2013).
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Varga J, Szilasi M. Common manifestation of airway diseases: chronic obstructive pulmonary disease and asthma bronchiale. Open Access J Sci 2018;2:26-31. [Crossref]
- Varga J. editor. A pulmonológiai rehabilitáció kézikönyve (Hungarian). Budapest: SpringMed Kiadó, 2018.
- Varga J. Krónikus obstruktív tüdőbetegség (COPD) (Hungarian). Háziorvos Továbbképző Szemle 2010;15:2-6.
- Fekete M, Pongor V, Fehér Á, et al. Krónikus légzőszervi betegek tápláltsági állapotának vizsgálata – klinikai megfigyelések Orv Hetil 2019;160:908-13. [Crossref] [PubMed]
- Mallia P, Johnston SL. Influenza infection and COPD. Int J Chron Obstruct Pulmon Dis 2007;2:55-64. [Crossref] [PubMed]
- Müllerova H, Chigbo C, Hagan GW, et al. The natural history of community-acquired pneumonia in COPD patients: A population database analysis. Respir Med 2012;106:1124-33. [Crossref] [PubMed]
- Böszörményi Nagy Gy, Balikó Z, Kovács G, et al. Egészségügyi szakmai irányelv a krónikus obstruktív tüdőbetegség (COPD) diagnosztikájáról és kezeléséről, az alap, a szak és a sürgősségi ellátás területén. Med Thor 2014;67:76112.
- Kopsaftis Z, Wood-Baker R, Poole P. Influenza vaccine for chronic obstructive pulmonary disease (COPD). Cochrane Database Syst Rev 2018;6:CD002733. [PubMed]
- Schembri S, Morant S, Winter JH, et al. Influenza but not pneumococcal vaccination protects against all-cause mortality in patients with COPD. Thorax 2009;64:567-72. [Crossref] [PubMed]
- Mereckiene J. Seasonal influenza vaccination in Europe: Vaccination recommendations and coverage rates in the EU Member States for eight influenza seasons, 2007-2008 to 2014-2015. 2017.v-pp. Available online: https://www.ecdc.europa.eu/sites/portal/files/documents/influenza-vaccination-2007–2008-to-2014–2015.pdf. Accessed 3 January 2020.
- Schmid P, Rauber D, Betsch C, et al. Barriers of Influenza Vaccination Intention and Behavior - A Systematic Review of Influenza Vaccine Hesitancy, 2005 - 2016. PLoS One 2017;12:e0170550. [Crossref] [PubMed]
- Ward JK. Rethinking the antivaccine movement concept: A case study of public criticism of the swine flu vaccine's safety in France. Soc Sci Med 2016;159:48-57. [Crossref] [PubMed]
- Coupland C, Harcourt S, Vinogradova Y, et al. Inequalities in uptake of influenza vaccine by deprivation and risk group: Time trends analysis. Vaccine 2007;25:7363-71. [Crossref] [PubMed]
- Lee TA, Weaver FM, Weiss KB. Impact of pneumococcal vaccination on pneumonia rates in patients with COPD and asthma. J Gen Intern Med 2007;22:62-7. [Crossref] [PubMed]
- Chiatti C, Barbadoro P, Marigliano A, et al. Determinants of influenza vaccination among the adult and older Italian population with chronic obstructive pulmonary disease: a secondary analysis of the multipurpose ISTAT survey on health and health care use. Hum Vaccin 2011;7:1021-5. [Crossref] [PubMed]
- Aka Aktürk Ü, Görek Dilektaşlı A, Şengül A, et al. Influenza and Pneumonia Vaccination Rates and Factors Affecting Vaccination among Patients with Chronic Obstructive Pulmonary Disease. Balkan Med J 2017;34:206-11. [Crossref] [PubMed]
- Schoefer Y, Schaberg T, Raspe H, et al. Determinants of influenza and pneumococcal vaccination in patients with chronic lung diseases. J Infect 2007;55:347-52. [Crossref] [PubMed]
- Eagan TM, Hardie JA, Jul-Larsen Å, et al. Self-reported influenza vaccination and protective serum antibody titers in a cohort of COPD patients. Respir Med 2016;115:53-9. [Crossref] [PubMed]
- Santaularia J, Hou W, Perveen G, et al. Prevalence of influenza vaccination and its association with health conditions and risk factors among Kansas adults in 2013: A cross-sectional study. BMC Public Health 2016;16:185. [Crossref] [PubMed]
- WHO. Ten threats to global health in 2019. 2020. WHO, Geneva. Available online: https://www.who.int/news-room/feature-stories/tenthreats-to-global-health-in-2019. accessed 10 January 2020.
- Fehér Á, Fekete M, Varga JT, et al. Az orvostanhallgatók vakcinológiai tájékozottsága. Orv Hetil 2019;160:1193-9. [Crossref] [PubMed]
- Garrastazu R, García-Rivero JL, Ruiz M, et al. Prevalence of Influenza Vaccination in Chronic Obstructive Pulmonary Disease Patients and Impact on the Risk of Severe Exacerbations. Arch Bronconeumol 2016;52:88-95. [PubMed]
- Alfageme I, Vazquez R, Reyes N, et al. Clinical efficacy of antipneumococcal vaccination in patients with COPD. Thorax 2006;61:189-95. [Crossref] [PubMed]
- Vandenbos F, Gal J, Radicchi B. Vaccination coverage against influenza and pneumococcus for patients admitted to a pulmonary care service. Rev Mal Respir 2013;30:746-51. [Crossref] [PubMed]
- Ciblak MA, Platformu G. Influenza vaccination in Turkey: prevalence of risk groups, current vaccination status, factors influencing vaccine uptake and steps taken to increase vaccination rate. Vaccine 2013;31:518-23. [Crossref] [PubMed]
- Pandolfi F, Franza L, Todi L, et al. The Importance of Complying with Vaccination Protocols in Developed Countries: "Anti-Vax" Hysteria and the Spread of Severe Preventable Diseases. Curr Med Chem 2018;25:6070-81. [Crossref] [PubMed]
- Varga J, Palinkas A, Lajko I, et al. Pulmonary Arterial Pressure Response During Exercise in COPD: A Correlation with C-Reactive Protein (hsCRP). Open Respir Med J 2016;10:1-11. [Crossref] [PubMed]
- Gross PA, Hermogenes AW, Sacks HS, et al. The efficacy of influenza vaccine in elderly persons. Ann Intern Med 1995;123:518-27. [Crossref] [PubMed]
- Wongsurakiat P, Maranetra KN, Wasi C, et al. Acute respiratory illness in patients with COPD and the effectiveness of influenza vaccination: a randomized controlled study. Chest 2004;125:2011-20. [Crossref] [PubMed]
- Ludwig E, Mészner Z. Hungarian Society of Infectious Disease and Clinical Microbiology, Vaccinology Section. Prevention of Streptococcus pneumoniae (pneumococcal) infections in adults. Orv Hetil 2014;155:1996-2004. [Crossref] [PubMed]
- Torres A, Peetermans WE, Viegi G, et al. Risk factors for community acquired pneumonia in adults in Europe: a literature review. Thorax 2013;68:1057-65. [Crossref] [PubMed]
- Polsky D, Bonafede M, Suaya JA. Comorbidities as a driver of the excess costs of community-acquired pneumonia in U.S. commercially-insured working age adults. BMC Health Serv Res 2012;12:379. [Crossref] [PubMed]
- Esposito S, Bonanni P, Maggi S, et al. Recommended immunization schedules for adults: Clinical practice guidelines by the Escmid Vaccine Study Group (EVASG), European Geriatric Medicine Society (EUGMS) and the World Association for Infectious Diseases and Immunological Disorders (WAidid). Hum Vaccin Immunother 2016;12:1777-94. [PubMed]
- Sung LC, Chen CI, Fang YA, et al. Influenza vaccination reduces hospitalization for acute coronary syndrome in elderly patients with chronic obstructive pulmonary disease: a population-based cohort study. Vaccine 2014;32:3843-9. [Crossref] [PubMed]
- Schwarz TF, Flamaing J, Rumke HC, et al. A randomized, double-blind trial to evaluate immunogenicity and safety of 13-valent pneumococcal conjugate vaccine given concomitantly with trivalent influenza vaccine in adults aged ≥65 years. Vaccine 2011;29:5195-202. [Crossref] [PubMed]
- Gilchrist SA, Nanni A, Levine O. Benefits and effectiveness of administering pneumococcal polysaccharide vaccine with seasonal influenza vaccine: an approach for policymakers. Am J Public Health 2012;102:596-605. [Crossref] [PubMed]
- Kraicer-Melamed H, O’Donnell S, Quach C. The effectiveness of pneumococcal polysaccharide vaccine 23 (PPV23) in the general population of 50 years of age and older: a systematic review and meta-analysis. Vaccine 2016;34:1540-50. [Crossref] [PubMed]
- Bhatt SP, Wells JM, Iyer AS, et al. Results of a Medicare Bundled Payments for care Improvement initiative for chronic obstructive pulmonary disease readmissions. Ann Am Thorac Soc 2017;14:643-8. [Crossref] [PubMed]
- Turner AM, Lim WS, Rodrigo C, et al. A care-bundles approach to improving standard of care in AECOPD admissions: Results of a national project. Thorax 2015;70:992-4. [Crossref] [PubMed]
- Birkhäuer J, Gaab J, Kossowsky J, et al. Trust in the health care professional and health outcome: A meta-analysis. PLoS One 2017;12:e0170988. [Crossref] [PubMed]
- Varga JT. Smoking and pulmonary complications: respiratory prehabilitation. J Thorac Dis 2019;11:S639-44. [Crossref] [PubMed]
- Sanei F, Wilkinson T. Influenza vaccination for patients with chronic obstructive pulmonary disease: understanding immunogenicity, efficacy and effectiveness. Ther Adv Respir Dis 2016;10:349-67. [Crossref] [PubMed]


