
Reverse “L” surgical approach for the management of giant tumors of the cervicothoracic junction
Introduction
The cervicothoracic junction (CTJ) refers to the region between the sixth cervical vertebrae and the third thoracic vertebrae (1). Giant tumors of the CTJ have a low incidence rate and are poorly defined. Surgical resection has been established as the most appropriate means of treatment for these tumors (2-4). Anatomically, the CTJ is a challenging region to access for resection due to the surrounding vital nerves and vascular structures (5). The principle of surgical resection is to achieve R0 resection without adversely affecting the structure or function of the surrounding vasculature and neural network (6).
Complete resection of giant tumors of the CTJ is not easily achieved by either thoracic or unilateral cervical method (7-9). Many surgeons adopt the transmanubrial osteomuscular sparing approach (TMA) as one of several methods applied to the CTJ tumor resection. TMA has been reported to preserve the sternoclavicular joint without shoulder deformity (10). However, TMA is mostly limited to tumors extending from the mediastinum to the neck. We optimized the TMA surgical method to achieve complete resection of CTJ tumors while retaining the function of nearby essential nerves and vasculature. This study presents our initial findings using the reverse “L” surgical approach.
We present the following article in accordance with the “The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) Statement” reporting checklist (available at http://dx.doi.org/10.21037/jtd-20-288B).
Methods
Study population
This was a retrospective review of all patients who underwent reverse “L” approach for CTJ tumor resection at Xinhua Hospital affiliated to Shanghai Jiao Tong University School of Medicine. Before 2014, median sternotomy was the most commonly used procedure out of several methods applied at our center. From August 2014 to August 2018, 21 patients with surgical resection of cervicothoracic lesions via reverse “L” approach were identified from our database. The study was conducted in accordance with the Declaration of Helsinki and the Harmonized Tripartite Guideline for Good Clinical Practice from the International Conference on Harmonization. This study was approved by the Institutional Review Board (IRB). All patients or their legal representatives signed the IRB-approved consent form before the relevant data was collected for this study.
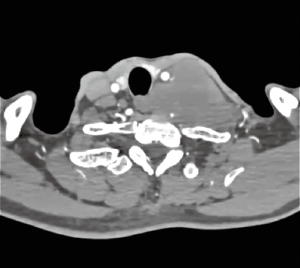
Before surgery, the resectability of the tumor and cardio-pulmonary function were carefully evaluated to ensure the patient was suitable for surgery. Chest-enhanced CT (Figure 1), abdominal ultrasound, brain computed tomography (CT), and radionuclide bone scan were performed to exclude metastases in malignant tumors.
Operative technique
The patient was placed in a supine position after the application of monitoring wires and general anesthesia via a double lumen endotracheal tube. Rolls were placed beneath the shoulders and the head was rotated 30°–45° away from the tumor (Figure 2).
A transverse incision was made superior to the clavicle, with a parallel course to the mid-portion of the suprasternal notch, continuing downward along the midline sternum to the 3rd or 4th interspace. After the subcutaneous tissue was fully separated, the upper sternum was segregated from the suprasternal fossa with a sternal saw. The sternum was cut to the 3rd or 4th intercostal space. The cut was subsequently extended to the costal space of the affected side. This resulted in the upper sternum being split in the shape of a reverse “L”. Bleeding from the edge of the sternum was prevented with bone wax. The upper sternum was opened with a small sternum opener (Finochietto 70 mm) to enable adequate exposure of the tumor. Special attention was given to the separation and protection of intramammary artery. When necessary, ligation of the intramammary artery was performed. The thoracic duct was identified, isolated, tied, and ligated. The critical vessels such as the nameless artery, subclavian artery, and superior vena cava were dissociated respectively and controlled distally.
For giant tumors of the CTJ, the removal of the entire tumor while preventing cancer cell spillage is optimal, although not always possible. In most cases, the tumor is dissected via piecemeal removal. In the current study, a drainage tube was placed at the conclusion of the dissection (Figure 3). The upper sternum was subsequently fixed with sternal steel wire or a butterfly plate (Figure 4). The subcutaneous and dermal layers of the incision were closed in layers. According to the pathological results and patients’ individual clinical conditions, we determined whether radiotherapy or chemotherapy was needed on a case-by-case basis. All patients underwent a regular review of the neck and chest via CT imaging.
Statistical analysis
The clinical characteristics and perioperative outcomes of the patients were analyzed using IBM SPSS 19.0 software package. Continuous variables were compared using two-sample t-tests. P<0.05 was considered statistically significant.
Results
In this study, giant tumors of the CTJ were successfully resected through reverse “L” surgical approach in all 21 patients (12 males and 9 females). No additional thoracoscopic assistance was needed. The median age of the patients was 46 (range, 13–75) years old. Neck and shoulder pain were the most commonly reported presentations, followed by a palpable mass. Nineteen patients underwent preoperative pathological puncture. There were 6 neurogenic tumors, 4 thyroid adenocarcinomas, 4 bronchogenic tumors, 1 adipose tissue and 4 epithelial tissues. However, 4 epithelial tumors were shown to have invaded adjacent structures. There were no clinical indications of malignancy. Postoperative pathological diagnosis of the resected tumors and the adjacent structures identified them as lymphomas. CT scans of 2 patients suggested the presence of angiomas, as shown by rich vasculature and obvious enhancement, negating the requirement for preoperative puncture. The 4 patients with bronchogenic tumors underwent neoadjuvant radiotherapy. They were treated with radiotherapy doses of 30–45 Gy. The patients’ demographic data, symptomatology and preoperative pathological diagnosis are recorded in Table 1.

Full table
Reverse “L” surgical approach was received from the left side in 14 patients and from the right side in 7 patients. No hospital deaths were observed. All patients who underwent endotracheal intubation were successfully extubated. The median operative time was 191.0 min (range, 113.0–348.0 min), and the postoperative hospital stay ranged from 3 to 7 days (Table 1). Bronchogenic tumor invasion was observed in 1 patient; this led to an axillary artery leak, which resulted in blood loss of 400 mL. A 10-cm angioma observed in the posterior mediastinum of another patient resulted in blood loss of 400 mL. A preoperative angiography was not performed, which contributed to the blood loss.
Postoperative pathological results showed 13 malignant cases and 8 benign cases. Eight of the 13 malignant tumors had adjacent structural involvement. To achieve R0 resection, the invaded adjacent structures were also resected. One case underwent superior vena cava artificial vascular replacement, 2 cases underwent unnamed vein ligature, 1 case underwent right axillary artery ligature, 1 case underwent ductus thoracicus ligature, and 3 cases underwent pulmonary lobe cuneiform resection. For bronchogenic tumors, the mean lymph node stations dissected were 5. Three cases of neurogenic tumors could not achieve R0 resection because the tumor originated from the spinal cord. All 4 cases of thyroid adenocarcinoma underwent adjuvant radionuclide therapy, and all 4 cases of bronchogenic tumors were treated with platinum-based adjuvant chemotherapy. The origins of the tumors, as well additional vascular procedures and complications, are detailed in Table 2.

Full table
Horner syndrome was observed in 1 case. Hoarseness occurred in 3 cases. Lymphatic leakage occurred in 1 case. Hemidiaphragm paralysis occurred in 1 case; although the phrenic nerve was clearly intact at the conclusion of the dissection, the patient developed hemidiaphragmatic palsy. These postoperative complications were transient, and the patients achieved full recovery through conservative treatment (Table 2). During follow-up, which ranged in length from 6–42 months, 11 of the 13 malignant patients showed no evidence of tumor recurrence. Two patients displaying bronchogenic tumors died of distant progression. Two postoperative deaths were observed, with the first occurring at 6 months and the second at 15 months after surgery.
Discussion
Giant tumors of the CTJ, which are located at the junction of the neck and mediastinum, are mostly caused by the upward growth of mediastinal tumors into the cervical root or the downward growth of cervical root tumors into the mediastinum (10-12). Surgical resection is the first-choice treatment for giant tumors of the CTJ (13,14). However, cervical or thoracic surgical approach does not provide sufficient exposure for achieving R0 resection (15,16). Although “trap-door” thoracotomy as a surgical approach can adequately reveal the tumor and prevent functional and anatomic alterations of the clavicle, the surgical trauma is significant and the postoperative recovery of the patient is slow (17,18). Over the last 20 years, several modified approaches have risen to facilitate resection (12). With the development of minimally invasive instruments and techniques seen in recent years, TMA surgery has become the preferred approach in cardiac and mediastinal surgery (19,20). According to the characteristics of giant tumors of the CTJ and the experience of previous methods, we optimized TMA by using a reverse “L” incision to resect giant tumors of the CTJ.
The TMA surgical approach offers wide surgical exposure with the possibility to perform en-bloc extended resection with no osteo-muscular sacrifice associated with good functional outcome (21). However, the application of TMA is mostly limited to tumors extending from the mediastinum to the neck. When the tumor volume of the neck is larger than the mediastinum, R0 resection is difficult to achieve through TMA. In contrast, a reverse “L” incision is more suitable for resecting tumors that extend from the neck to the mediastinum, when the volume of the neck is larger. The application of reverse “L” incision has progressively increased the rate of R0 resection.
Reverse “L” incision involves technical modifications. The sternum should be split at the 3rd or 4th interspace to adequately expose the tumor tissue of the mediastinum. Subsequently, the sternum should be cut transversely to the costal space (near the affected side), to prevent accidental splitting of the lower section of the sternum. Special attention is required to maintain the connection between the costal cartilage and sternum to keep the stability when the sternum is transversely sawed to the costal space. As the main nourishing artery of the sternum, protection of the intramammary artery should be emphasized, especially in elderly or diabetic patients. In elderly patients with thin sternums or osteoporosis, the upper section of the sternum should be fixed with a butterfly plate instead of a steel wire to avoid the shear force.
The resection of giant tumors of the CTJ was successfully completed through reverse “L” surgical approach in the 21 patients in this study. All of the patients were successfully extubated. No hospital deaths occurred, and none of the patients experienced delayed wound healing. All of the patients recovered and were discharged without incident. Due to the surgical field of vision being clear, the operation is safe and the postoperative complications are reduced.
This study has several limitations. First, the patient cohort was heterogeneous in terms of pathology. The evaluation of safety and risk factors calls for a control group and a comparison with another surgical approach. Second, this was a single-institution study, which may have caused a potential bias. Third, the follow-up period was too short to reach any oncologic considerations. Longer-term prospective data and patient follow-up are needed to fully evaluate the outcomes of this technique in comparison to other surgical approaches.
Acknowledgments
Funding: This work was funded by National Natural Science Foundation of China (Grant No. 81772459).
Footnote
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at http://dx.doi.org/10.21037/jtd-20-288B
Data Sharing Statement: Available at http://dx.doi.org/10.21037/jtd-20-288B
Peer Review File: Available at http://dx.doi.org/10.21037/jtd-20-288B
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/jtd-20-288B). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013) and the Harmonized Tripartite Guideline for Good Clinical Practice from the International Conference on Harmonization. This study was reviewed and approved by institutional ethics committee of Xinhua Hospital affiliated to Shanghai Jiao Tong University School of Medicine (approval number XHEC-D-2020-038). All patients enrolled completed the informed consent form.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Liu YL, Hao YJ, Li T, et al. Trans-upper-sternal approach to the cervicothoracic junction. Clin Orthop Relat Res 2009;467:2018-24. [Crossref] [PubMed]
- Dalbayrak S, Yaman O, Yilmaz M, et al. Results of the transsternal approach to cervicothoracic junction lesions. Turk Neurosurg 2014;24:720-5. [PubMed]
- Christison-Lagay ER, Darcy DG, Stanelle EJ, et al. "Trap-door" and "clamshell" surgical approaches for the management of pediatric tumors of the cervicothoracic junction and mediastinum. J Pediatr Surg 2014;49:172-6; discussion 176-7. [Crossref] [PubMed]
- Park JH, Im SB, Jeong JH, et al. The Transmanubrial Approach for Cervicothoracic Junction Lesions: Feasibility, Limitations, and Advantages. J Korean Neurosurg Soc 2015;58:236-41. [Crossref] [PubMed]
- Aigner C, Reza Hoda MA, Klepetko W. Combined Cervicothoracic Approaches for Complex Mediastinal Masses. Thorac Surg Clin 2009;19:107-12. [Crossref] [PubMed]
- Kayawake H, Chen-Yoshikawa TF, Date H. Dual approach for large mediastinal tumors in the thoracic outlet: transmanubrial osteomuscular sparing approach and video-assisted thoracoscopic surgery. J Cardiothorac Surg 2019;14:42. [Crossref] [PubMed]
- Spaggiari L, Pastorino U. Transmanubrial approach with antero-lateral thoracotomy for apical chest tumor. Ann Thorac Surg 1999;68:590-3. [Crossref] [PubMed]
- Park HY, Lee SH, Park SJ, et al. Surgical management with radiation therapy for metastatic spinal tumors located on cervicothoracic junction: a single center study. J Korean Neurosurg Soc 2015;57:42-9. [Crossref] [PubMed]
- Korst RJ, Burt ME. Cervicothoracic tumors: results of resection by the "hemi-clamshell" approach. J Thorac Cardiovasc Surg 1998;115:286-94; discussion 294-5. [Crossref] [PubMed]
- Pan X, Gu C, Wang R, et al. Transmanubrial osteomuscular sparing approach for resection of cervico-thoracic lesions. J Thorac Dis 2017;9:3062-8. [Crossref] [PubMed]
- Wang VY, Chou D. The cervicothoracic junction. Neurosurg Clin N Am 2007;18:365-71. [Crossref] [PubMed]
- Baker JF, Shafqat A, Devitt A, et al. Surgical management of metastatic lesions at the cervicothoracic junction. J Craniovertebr Junction Spine 2015;6:115-9. [Crossref] [PubMed]
- Le H, Balabhadra R, Park J, et al. Surgical treatment of tumors involving the cervicothoracic junction. Neurosurg Focus 2003;15:E3. [Crossref] [PubMed]
- Rusca M, Carbognani P, Bobbio P. The modified "hemi-clamshell" approach for tumors of the cervicothoracic junction. Ann Thorac Surg 2000;69:1961-3. [Crossref] [PubMed]
- Matsuguma H, Nakahara R, Ishikawa Y, et al. Transmanubrial osteomuscular sparing approach for lung cancer invading the anterior part of the thoracic inlet. Gen Thorac Cardiovasc Surg 2010;58:149-54. [Crossref] [PubMed]
- Huang YX, Tian NF, Chi YL, et al. Mini-open anterior approach to the cervicothoracic junction: a cadaveric study. Eur Spine J 2013;22:1533-8. [Crossref] [PubMed]
- Radek A, Maciejczak A, Kowalewski J, et al. Trans-sternal approach to the cervicothoracic junction. Neurol Neurochir Pol 1999;33:1201-13. [PubMed]
- Lebreton G, Baste JM, Thumerel M, et al. The hemiclamshell approach in thoracic surgery: indications and associated morbidity in 50 patients. Interact Cardiovasc Thorac Surg 2009;9:965-9. [Crossref] [PubMed]
- Paparella D, Malvindi PG, Santarpino G, et al. Full sternotomy and minimal access approaches for surgical aortic valve replacement: a multicentre propensity-matched study. Eur J Cardiothorac Surg 2020;57:709-16. [PubMed]
- Mikus E, Calvi S, Campo G, et al. Full Sternotomy, Hemisternotomy, and Minithoracotomy for Aortic Valve Surgery: Is There a Difference? Ann Thorac Surg 2018;106:1782-8. [Crossref] [PubMed]
- Spaggiari L, Calabrese L, Gioacchino G, et al. Cervico-thoracic tumors resection through transmanubrial osteomuscular sparing approach. Eur J Cardiothorac Surg 1999;16:564-7. [Crossref] [PubMed]





