
How to optimize the treatment strategy for patients of pulmonary sequestration with an elevated risk of fatal hemorrhage during operation: case discussion
Introduction
Pulmonary sequestration (PS) is characterized by nonfunctioning pulmonary parenchyma, the blood supply of which always originates from a systemic artery, without tracheobronchial airway connection (1). PS is categorized into two subtypes: one is intralobar sequestrations (ILS), which are usually encapsulated in a standard pleural layer with normal lung tissue. Another is extralobar sequestrations (ELS), of which they are contained in a separate pleural lining apart from normal lung tissues (2).
Surgical resection of lesions and occlusion of the feeding vessel under radiographic control are the major treatment for PS (3-6). Complications reported after embolization include pain and pyrexia, pleural effusion, transient ischemia of the lower limb, recanalization of the artery and persistent chest-X ray changes (7). Surgery is regarded as the preferred treatment for PS (3,8-10), especially for those symptomatic PS. However, it is difficult to give an evidence-based argument for treatment of all sequestrations, particularly for those that are asymptomatic. It is crucial to weigh the negative effects of the risks of surgical morbidity against the risks of complications of the PS itself, especially for those are small or asymptomatic lesions. An increasing evidence have indicated that minimally invasive video-assisted thoracic surgery has many advantages in the treatment of PS. Comparing with open surgery, thoracoscopy can clearly reveal the hilar area and aberrant feeding area; other indicators including blood loss, duration of chest tube insertion, postoperative hospital stay and complications also have a slight advantages (10-14). However, some difficulties still exist. One is the identification of the aberrant artery. Repeated stimulation of inflammation changes the tissue’s microenvironment. Dense adhesions accompanied with proliferative vessels would make the surgical field bloody and blurred during dissection. Moreover, it is difficult to control the bleeding under VATS when unanticipated injuries of aberrant vessels occurred. Although endo cutter is not clearly indicated for cutting the branches of the aortic system, it is safe to use appropriate size of vascular stapler on arteries of good condition. In contrast with pulmonary vessels, which are rarely affected by atherosclerosis, the aberrant arteries of PS originated from aortic system are easily affected by atherosclerosis. Some reports described that it is the inflammation caused the increasing of the bleeding events, but rare demonstrated the negative impact of severe atherosclerosis on aberrant vessels, especially how to cut off safely under minimally invasive thoracic surgery. In this case report, we demonstrated a case of intralobar sequestration with a thickened, atherosclerosis of aberrant artery and how we treat it without an occurrence of fatal bleeding.
We present the following article in accordance with the CARE reporting checklist (available at http://dx.doi.org/10.21037/jtd-20-2059).
Case presentation
A 56-year-old male patient was admitted to the hospital with a lung mass in his right lower lobe. Two months before admission, he suffered a traffic accident, which resulted in multiple fractures on his left leg, and a mass was found at that time. The patient had a long history of cough with purulent sputum. One month before the trauma, the patient had copious expectoration with foul smell again. Until the emergency operation, the patient had not taken the symptoms seriously and had no later examinations. Two months after surgery, the patient came to our hospital for further treatment.
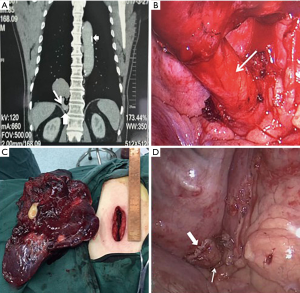
A contrast CT scan revealed a 7.5 cm mass in the right lower lobe. The mass was supplied by a thick aberrant artery, which stemmed from the thoracic aorta with multiple calcifications on both (Figure 1A). After fully assessed the lesion and this patient’s symptoms, PS had been diagnosed. Relevant check-ups, including coagulation tests, d-dimer, and venography of veins at both lower limbs indicated there were no recent thromboembolic events occurring. Sputum culture was negative either. After obtaining the patient’s informed consent for the operation, a uniportal VATS lobectomy was scheduled. No surgical-associated complications occurred, and the patient was discharged on the 5th days after the operation.
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this case report and any accompanying images.
Surgery
A 3.5 cm incision was made in the right 5th intercostal space between the posterior and mid-axillary lines, and a wound protector was applied. The entire operation was performed by using a 30° 10mm video-thoracoscope. Intra-operatively, we found the aberrant vessel was hard to be exposed, and therefore we decided to perform the right lower lobectomy first to create more space for better management of the vessel. After dissecting and cutting the branches of the lower pulmonary artery, bronchus and vein, the thick aberrant artery was exposed completely (Figure 1B). We found two features of the aberrant artery, one is the vascular wall, which is hard and fragile due to the impact of atheroma, the other is its diameter which surpass the safety range of the Hemo-o-lock clips (a device for clipping blood vessels); besides, cutting the thick, hard and fragile artery with atherosclerosis and calcification may cause a life-threatening hemorrhage due to an unstable stapling by using the endo cutter directly (Echelon Flex 45 stapler). Eventually, we enlarged the incision from 3.5 to 5 cm (Figure 1C) and inserted a vascular closure device (TX30v) to block the blood flow first and use endo cutter to clamp and cut the artery at 0.5 cm away from the proximal clamping site, no bleeding occurred (Figure 1D). The whole operation was completed in 180 min, the blood loss was about 80 mL. Only a 20-F chest tube was inserted via the uniportal incision and connected to a chest drainage device. The patient was discharged on the fifth postoperative day. After six months of follow-up, the patient completely recovered without surgical-related complications.
Pathology
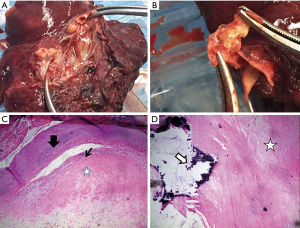
Macroscopically, the bronchi in the sequestrated lung were dilated and held a 5.5 cm lumen filled with purulent mucus (Figure 2A). The aberrant arterial wall was partly yellowish, suggesting the existence of atherosclerosis (Figure 2B). Microscopic examination showed epithelioid cell granuloma with coagulation necrosis. Atherosclerosis of the aberrant elastic artery was also found, in which accumulation of foamy cell macrophages and calcification were observed (Figure 2C,D).
iMDT discussion
Discussion among experts from the Liaoning Cancer Hospital & Institute.
Inputs from imaging specialist
This patient was diagnosed with PS following trauma. PS is a congenital malformation characterized by cystic, non-functioning embryonic lung tissue which lacks normal connection with the tracheobronchial tree and receives an abnormal blood supply originating from the descending thoracic or abdominal aorta. Venous usually drainage to pulmonary veins but occasionally to systemic veins (15). Two types of PS have been identified: extralobular sequestration and intralobular sequestration. Several reports suggested that intralobular sequestration is more common, accounting for 75–84% of all PSs (16-19).
Inputs from pathologists
Elderly patients complicated with high blood pressure, hyperlipidemia and diabetes, have a high risk of atherosclerotic vascular disease. Atheromatous vessels, always identified among systemic circulation arteries, are soft and fragile with little elasticity. In contrast, the pulmonary artery (PA) is rarely affected by atherosclerosis, even after systemic damage (20,21). Normally, Pulmonary artery pressure is lower than aortic pressure due to the lower pulmonary vascular resistance and this results in lower shear stress, therefore, less endothelial damage, which might not trigger atherogenesis (10,11). Unlike pulmonary arteries, aberrant arteries often originate from the aortic system, and easily progress atherosclerosis in its inner vascular wall.
Inputs from thoracic surgeons
Surgery is considered as an appropriate method for patients with PS especially for those who have permanent symptoms or cancer (9). In recent years, VATS has increasingly been accepted as an alternative procedure because of its minimal invasiveness (22,23). We need divide and cut nourishing vessels carefully to avoid the happening of catastrophic hemorrhage, especially under the uniport-VATS approach. However, few studies reported atherosclerosis existing in the aberrant arteries of intralobular sequestration, and none of them described the hemorrhage risks intraoperatively (24,25).
In endoscopic procedures, aberrant vessels can be ligature or clamped with Hemo-o-lock when the diameter is less than 1.6 cm. For those vessels which have exceeded the maximum clipping range of the device, it will damage the vascular and cause bleeding. Therefore, using an endo cutter fixed with a proper stapler may be a good choice in clamping and cutting vessels with good elasticity.
However, for those thick aberrant arteries with severe atherosclerosis, cutting them by using an endo cutter directly has a risk of bleeding due to unstable staple and squeeze the fragile vascular wall. After assessing the above risks, we clipped the vessel first and cut at 0.5 cm away from the blocking site without enlarging the surgical incision, and no bleeding occurred. When we dissected the aberrant artery on the specimen, we found a large atheromatous plaque attached to the vascular wall with some unstable nails next to it. If we hadn’t block the vessel before cutting it, a fatal hemorrhage would occurred inevitably.
In this case, there are several questions that should be further considered.
Question 1: For those vessels exceeded the maximum clipping range of the device, does endo cutter can be used for clamping and cutting vessels?
Expert opinion 1: Dr. Atsushi Ito
Congratulations. Dr. Liu et al. successfully performed uniportal VATS for such a challenging case which has some difficulties as below. The main difficulty during resection of a PS lesion is management of the aberrant artery because the vessel is easy rupturing and bleeding due to the anomalous fragile elastic layer and the local infection (16). Therefore, as the authors mentioned, clamping the proximal end of aberrant artery with a vascular closure device is suggested to prevent uncontrollable bleeding in case of endo cutter misprocessing. However, we should not hesitate to convert thoracotomy to treat such an enlarged aberrant artery with atherosclerosis under extracorporeal circulation. In the case of surgery of patent ductus arteriosus (PDA) in adults, it has been reported that the thoracic endograft and the balloon catheter for blocking blood flow are useful for management of the calcified PDA (17).
Expert opinion 2: Dr. Michel Gonzalez
Pulmonary sequestration is congenital malformation characterized by abnormal arterial blood supply to the pulmonary parenchyma. These “aberrant arteries” generally arrive from a branch or directly from the aorta. The location in a small confinement (the inferior pulmonary ligament), the variable diameter and the inflammatory aspect of these aberrant arteries all make it difficult to safely introduce an endostapler device and use it to transect. Most studies have demonstrated that pulmonary arteries of various diameters can be safely transected with staplers but, owing to the rarity of the condition, little is known about systemic arteries, apart from some scarce case reports or studies on small groups of patients. For small systemic arteries (<1 cm in diameter), clips or vascular staplers may be a good alternative to classical intra-operative suture. For larger vessels, an experimental model with pig aorta revealed that large systemic arteries can be safely transected after careful selection of the stapling cartridge size based on the diameter of the aberrant artery (18). In addition, fatal events after transection of systemic arteries have never been reported. Thus, I would recommend to use a blue cartridge (intermediate) for thick arteries and a white cartridge (small) for thin arteries, depending on their inflammatory aspect. In addition, I would recommend to use six rows of staples instead of four for safety reasons. Curved tips may also be helpful for introduction of the stapler around the vessel, particularly in small confinements.
Expert opinion 3: Dr. Kyoji Hirai
Generally, treatment for vessels with heterogeneous structures due to atherosclerosis should be careful done. According to several reports, end cutter is useful to treat aberrant artery of pulmonary sequestration. However, to be precise, there is no experimental evidence that end cutter can be safely used for transecting the aberrant artery. So that fatal hemorrhage won’t occur, vessel treatment should be done carefully. If endo cutter uses in transecting the aberrant artery with calcification or the diameter of vessel is more than 2 cm, reinforcement of cutting line or additional ligation treatment may be desirable to prevent of hemorrhage and aneurysm development.
Expert opinion 4: Dr. Mateusz Polaczek
Using endo cutter for the management of arterial vessels supplying pulmonary sequestration should be consider as effective method with some potential downsides. The increased risk of bleeding is mainly associated with atherosclerosis or an aneurysm of the aberrant artery and those are not so uncommon. Therefore some preparation steps to ensure precise cutting with endo cutter after endo stapling the artery can be conducted: good dissection of the proximal part of the artery and double clamping the proximal end. Endo cutter should not be used solely as clamping method for vessel over 2 cm.
Question 2: For ensuring the safety of cutting those aberrant arteries with a diameter of more than 2 cm and severe atherosclerosis with calcification, which procedures should be recommended?
Expert opinion 1: Dr. Atsushi Ito
It is generally accepted that identification of aberrant artery is exclusively important in thoracoscopic surgery of PS. Fatal bleeding during operation is caused by the confusion in the local anatomy as caused by inflammatory changes, previous unawareness of the existence of the aberrant artery. Therefore, as in this case, if the aberrant vessels are hard to be exposed, it is one of the methods which the lobectomy is performed first to create ideal space for management of the vessels. However, if the dissection of the pulmonary vein is preceded, the lung to be resected may swell due to the perfusion of blood supply from aberrant artery, resulting in narrow surgical space. Hence, it is preferable to dissect the aberrant artery first if possible.
Another point for ensuring the safety of cutting aberrant artery is that proximal end of the artery keep long enough for introduced endo stapler. Anatomization of the aberrant artery should be performed as long as possible to reserve a relative long proximal end for clamping it quickly if unexpected bleeding happens. On the other hand, long arterial stump may be associated with risk of embolism and aneurysm, and thus it requires long-term follow-up after surgery.
Expert opinion 2: Dr. Michel Gonzalez
As mentioned before, large vessels can be safely transected by using an endo-stapler. Generally, it is infrequent to have changes in the arterial wall such as atherosclerosis, aneurysm or calcification in cases of pulmonary sequestration. This unusual situation may increase surgical difficulty and expose the patients to catastrophic hemorrhage. Various techniques may be used to facilitate the transection. First, the use of a clamp proximally to the transection before the transection will decrease pressure on the stapler line during transection. This also allows the surgeon to control the situation in case of stapler misfiring and gives them time to convert to open thoracotomy if necessary, although this remains a rare occurrence. Alternatively, an aortic endo-prosthesis could be inserted before the VATS procedure to exclude the aberrant artery and safely transect it without pressure or massive hemorrhage. This technique should only be proposed when pulmonary resection is indicated.
Expert opinion 3: Dr. Kyoji Hirai
In this case, the structure of aberrant arterial wall is heterogenous and unstable. The efficacy of endo cutter to such as this case cannot be reliable and universal. Considering the patient’s age and characteristics of vessel wall, the stapling and double ligation treatment to proximal to descending aorta will be recommended to reduce of occurrence of aneurysm development. If ligation treatment is impossible anatomically, reinforcement of stapling line by monofilament nylon thread with pledget should be recommended. In direct suturing to descending aorta, it would be better to have reinforcement of stapling line assisted by a cardiothoracic surgeon.
Expert opinion 4: Dr. Mateusz Polaczek
Each arterial vessel supplying sequestration should be considered as potential cause of serious bleeding, although high blood pleasure makes the identification of this vessel easier. Most arteries to sequestration will run in pulmonary ligament which is extremely changed because of chronic inflammation and makes the dissection especially difficult. We do not recommend to dissect the whole length of the vessel but to only find the origin and dissect proximal portion of the artery, then using tourniquets to secure the origin as short trunk and later with endostapler to cut off the vessel.
Question 3: Are there non-surgical treatments can be applied for such patients?
Expert opinion 1: Dr. Atsushi Ito
Endovascular treatment with thoracic endograft has been reported as a safe alternative to surgery (19). This kind of treatment might be promising for occlusion of the enlarged aberrant vessels. However, there is a possible risk of symptoms recurrence or lesion enlarged. Long term follow-up was required to determine whether surgical resection was needed. Moreover, the risk of stent infection should be taken into account as the major concern about the thoracic endograft.
Expert opinion 2: Dr. Michel Gonzalez
Normally, pulmonary resection is performed in case of parenchyma anomaly or of local complications such an abscesses. When only an aberrant artery is present, without local complication in the parenchyma or hemoptysis, a non-surgical approach has shown promising short-term outcomes with complete exclusion of the aberrant artery. For small-diameter arteries, coils may be inserted by endovascular technique. The documented risks include embolization of the coils to the pulmonary arteries, vessel injury secondary to coil manipulation, transient limb ischemia or femoral artery thrombus at the puncture site. In case of large vessels, the additional use of an aortic thoracic stent graft to exclude the aberrant vessel addresses the potential complication of post-procedure recanalization as well as coil migration after embolization. In my opinion, such approaches should be reserved for non-operable symptomatic patients without pulmonary anomaly.
Expert opinion 3: Dr. Kyoji Hirai
Endovascular treatment such as coil and Amplatzer Vascular plug embolization to aberrant artery is a candidate for the treatments of patients with pulmonary sequestration. However, a 7.5cm mass in the right lower lobe is too large, after embolization there is a possibility of the abscess formation in this mass. In this case, surgical treatment is the best. If the abscess formation occurs in right lower lobe, right lower lobectomy will end up being performed.
Expert opinion 4: Dr. Mateusz Polaczek
Surgery should be considered as definitive treatment for all symptomatic patients and for most asymptomatic, although local experience and patients will should be taken under consideration (20,21). If thick and potentially hard to clamp arterial vessels are detected during presurgical workup some authors suggest the use of preoperative embolization of this arterial supply to minimize the bleeding risk (22).
Question 4: What should be noted before making an appropriate treatment strategy in such patients?
Expert opinion 1: Dr. Atsushi Ito
PS is known to receive a systemic artery supply from the descending aorta or the abdominal aorta or the celiac artery. Adequate preoperative imaging is therefore crucial for accurately defining the vascular anatomy and potentially embolizing the feeding vessels. Arterial angiography is thought to be the gold standard, however, in recent years, several studies reported that CT angiography and magnetic resonance angiography may be equally effective and safer alternatives. A multi-disciplinary discussion including cardiologists and radiologists etc. is crucial for the treatment of such patients. In case of unexpected catastrophic haemorrhage, it is also important to disinfect the inguinal lesion and keep it clean to introduce percutaneous cardiopulmonary support immediately.
Expert opinion 2: Dr. Michel Gonzalez
Several aspects should be addressed before decision making and surgical strategy design. The first aspect is the symptomatology of the patients. In case of incidental finding in an asymptomatic patient, or if the patient is not eligible for surgery, or in case of absence of parenchymal lesions, a non-surgical approach should be discussed. Otherwise surgery should be proposed for symptomatic patients and those with parenchymal lesions. The VATS approach (and its general set of advantages) has been reported to be safe and efficient to control aberrant systemic arteries, whether performed by uniport or multiport approach. The diameter of the aberrant artery, its exact origin and the aspect of the arterial wall should be clearly identified with a thin slice injected thoraco-abdominal CT-scan. The use of software with 3D reconstruction of arteries may help in such situations. During surgery, inflammatory changes of the sequestrated lung due to recurrent infections may hide the aberrant artery in scar tissue. Therefore, I would recommend that the identification of the aberrant artery or arteries should be done carefully at the beginning of the procedure. Then, endostapler may be used for transection even for larger arteries, as described above. In thoracoscopic surgery cases, the use of curved tips may facilitate the introduction of stapler around the vessel. Proximal control can be achieved by vascular clamp or suture to release pressure when transection is performed. The pre-operative insertion of aortic endo-prosthesis could be an alternative in case of aneurysmal or atherosclerotic aberrant arteries, but should be discussed individually by a multidisciplinary team.
Expert opinion 3: Dr. Kyoji Hirai
This case represents a 7.5 cm mass in right lower lobe feeding from aberrant artery branched to the descending aorta. A middle-aged man with atherosclerosis and calcification in aberrant artery have no inflammatory change before operation. A diameter of aberrant artery was more than 2 cm. Though the statement of descending aorta around the beginning of aberrant artery was not described, the evaluation of characteristics of vessels is essential. At least, the examination of 3D CT was necessary and the author should have evaluated the beginning of aberrant artery.
Poor treatment of aberrant artery may evoke fatal hemorrhage and aneurysm development intra- or postoperatively. In this case, careful follow-up for stapling line will be needed.
Expert opinion 4: Dr. Mateusz Polaczek
Detailed presurgical diagnosis should be carried out in each case of pulmonary sequestration before potential surgery. Anatomy of arterial vessels supplying the sequestration should be established in each case, but potential bleeding from the venous outflow should not be overlooked as well. What is essential, in each case bronchial lavage cultures for aerobic bacteria, tuberculosis and non-tuberculosis mycobacteria and funguses should be carried and antibiotic treatment conducted before surgery in cases with positive cultures. Aspergillus fumigatus may be the most common etiological factor of chronic infection in pulmonary sequestrations (21), which was also possible in present case based on pathological report.
Conclusions
It is crucial to evaluate the quality of thick aberrant vessels (over 2 cm in diameter) of PS before surgery, and appropriately treating those vessels is the key to avoid fatal hemorrhage intraoperatively
Acknowledgments
Funding: Technological Special Project of Liaoning Province of China (2019020176-JH1/103).
Footnote
Reporting Checklist: The authors have completed the CARE reporting checklist. Available at http://dx.doi.org/10.21037/jtd-20-2059
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/jtd-20-2059). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this case report and any accompanying images.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Sakai M, Ozawa Y, Konishi T, et al. Endostapling the aberrant artery filled with embolized coils for intralobar pulmonary sequestration: a report of two cases. J Thorac Dis 2018;10:E304-8. [Crossref] [PubMed]
- Savic B, Birtel FJ, Tholen W, et al. Lung sequestration: report of seven cases and review of 540 published cases. Thorax 1979;34:96-101. [Crossref] [PubMed]
- Sun X, Xiao Y. Pulmonary sequestration in adult patients: a retrospective study. Eur J Cardiothorac Surg 2015;48:279-82. [Crossref] [PubMed]
- Fu S, Wang H. Pulmonary sequestration associated with a synchronous elevation of carbohydrate antigen 50 and 19-9: a case report. Ann Transl Med 2018;6:212. [Crossref] [PubMed]
- Hwang HK, Tsai YS, Lin SM, et al. Occlusion of an aberrant artery to an intralobar pulmonary sequestration using an Amplatzer Vascular Plug. Pediatr Pulmonol 2008;43:933-5. [Crossref] [PubMed]
- Crushell E, Saidi A, al-Hassan A, et al. Occlusion of an aberrant artery to a pulmonary sequestration using a duct occluder. J Interv Cardiol 2002;15:415-6. [Crossref] [PubMed]
- Park ST, Yoon CH, Sung KB, et al. Pulmonary sequestration in a newborn infant: treatment with arterial embolization. J Vasc Interv Radiol 1998;9:648-50. [Crossref] [PubMed]
- Costa Junior Ada S, Perfeito JA, Forte V. Surgical treatment of 60 patients with pulmonary malformations: what have we learned? J Bras Pneumol 2008;34:661-6. [PubMed]
- Bratu I, Flageole H, Chen MF, et al. The multiple facets of pulmonary sequestration. J Pediatr Surg 2001;36:784-90. [Crossref] [PubMed]
- Zhang N, Zeng Q, Chen C, et al. Distribution, diagnosis, and treatment of pulmonary sequestration: Report of 208 cases. J Pediatr Surg 2019;54:1286-92. [Crossref] [PubMed]
- Wang S, Li Y, Wang J. Video-Assisted Thoracoscopic Surgery for Pulmonary Sequestrations: Series of 35 Consecutive Patients in a Single Center. Thorac Cardiovasc Surg 2019;67:73-8. [Crossref] [PubMed]
- Li XK, Luo J, Wu WJ, et al. Effect of different therapeutic strategies on the clinical outcome of asymptomatic intralobar pulmonary sequestration. Interact Cardiovasc Thorac Surg 2019;29:706-13. [Crossref] [PubMed]
- Traibi A, Seguin-Givelet A, Brian E, et al. Rev Mal Respir 2019;36:129-34. [Pulmonary intralobar sequestration in adults: Evolution of surgical treatment]. [Crossref] [PubMed]
- Lin ZW, Gu J, Xu ST, et al. Video-Assisted Thoracoscopic Surgery for Intralobar Pulmonary Sequestration: Wedge Resection Is Feasible in Limited Peripheral Lesions. Thorac Cardiovasc Surg 2016;64:456-60. [Crossref] [PubMed]
- Takahashi M, Ohno M, Milhara K, et al. Intralobar pulmonary sequestration; with special emphasis on bronchial communication. Radiology 1975;114:543-9. [Crossref] [PubMed]
- Wei Y, Li F. Pulmonary sequestration: a retrospective analysis of 2625 cases in China. Eur J Cardiothorac Surg 2011;40:e39-42. [Crossref] [PubMed]
- Herman TE, Siegel MJ. Congenital intralobar pulmonary sequestration with cystic adenomatoid malformation. J Perinatol 2009;29:175-7. [Crossref] [PubMed]
- Thilenius OG, Ruschhaupt DG, Replogle RL, et al. Spectrum of pulmonary sequestration: association with anomalous pulmonary venous drainage in infants. Pediatr Cardiol 1983;4:97-103. [Crossref] [PubMed]
- Gonzalez D, Garcia J, Fieira E, et al. Video-assisted thoracoscopic lobectomy in the treatment of intralobar pulmonary sequestration. Interact Cardiovasc Thorac Surg 2011;12:77-9. [Crossref] [PubMed]
- Cicconi M, Bonsignore A, Orcioni GF, et al. Primary pulmonary arteries atherosclerosis: discovering an unusual cause of death in forensic practice. Romanian Journal of Legal Medicine 2012;20:177-80. [Crossref]
- Esper RJ, Nordaby RA, Vilarino JO, et al. Endothelial dysfunction: a comprehensive appraisal. Cardiovascular Diabetology 2006;5:4. [Crossref] [PubMed]
- Macias L, Ojanguren A, Dahdah J, et al. Thoracoscopic anatomical resection of congenital lung malformations in adults. J Thorac Dis 2015;7:486-9. [PubMed]
- Wang LM, Cao JL, Hu J. Video-assisted thoracic surgery for pulmonary sequestration: a safe alternative procedure. J Thorac Dis 2016;8:31-6. [PubMed]
- Okamoto J, Kubokura H, Usuda J. Safe transection of aberrant arteries associated with pulmonary sequestrations. BMC Surg 2015;15:27. [Crossref] [PubMed]
- Hashimoto H, Yanagiya M, Kusakabe M, et al. Atherosclerosis of aberrant arteries from the left gastric artery into the right intralobar pulmonary sequestration complicated by mycobacterial epithelioid cell granuloma. Cardiovasc Pathol 2017;26:4-6. [Crossref] [PubMed]


