Respiratory management of the obese patient undergoing surgery
Introduction
Obesity, as defined by a body mass index (BMI) of ≥30 kg/m2 (1), has almost doubled since 1980 to affect an estimated 671 million individuals worldwide (2). Furthermore, morbid obesity, defined as a BMI above 40 kg/m2, is rising (3). In the United States, China and United Kingdom (UK), obesity has a current prevalence of 32%, 4% and 25%, respectively in adult males and 34%, 5% and 25% respectively in adult females (2). The direct cost to the NHS in England for treating obesity, and its related morbidity, is estimated to be above £4 billion (4). The UK reported a 30-fold increase in the number of bariatric surgical procedures over ten years, a ten-fold increase in the number of hospital episodes primarily related to obesity over a decade (5) and it has been estimated that 25% of all UK patients admitted to intensive care units (ICU) are obese with 7% morbidly obese (6). It is therefore not surprising that the respiratory management of obese subjects, in particular in the pre- and peri-operative stage, represents a growing challenge to surgeons, pulmonologists, anesthetists and intensivists (7,8). This review will detail the physiological effects of obesity on the respiratory system and report the evidence-based strategies to manage the pre- and peri-operative phase.
Obesity-related changes in respiratory physiology
Effects of obesity on the respiratory system
Obesity is associated with increased work of breathing as a consequence of increased airways resistance and reduced respiratory system compliance (9-12) Lung volume falls as a function of obesity (13) as a result of the increased abdominal volume and visceral fat (14,15). Respiratory system compliance in the obese can be reduced by up to 35% (12) due to (I) the restrictive effect of mass loading on the chest wall (15,16); (II) a tendency to breathe at low lung volumes (17,18); and (III) the effect of fat distribution that contributes to high pleural pressures and leads to low end-expiratory volumes with expiratory flow limitation when supine (19). The decrease in overall compliance, however, is principally driven by a decrease in lung compliance, in turn, being the result of an increased pulmonary blood volume (20). Breathing at low volumes increases airway resistance (12) with expiratory flow limitation and gas trapping due to early airway closure and subsequent generation of intrinsic positive end-expiratory pressure (PEEPi) (20) and ventilation-perfusion mismatching, especially when supine and asleep (21). These phenomena serve to further increase work of breathing (14).
These physiological changes are heightened during sleep in the supine position due to the negative impact on the pulmonary mechanics of diaphragm impedance by the abdomen with a change in lung volume (15,22-24). This impairs the capacity of obese patients to tolerate apneic episodes with early onset oxygen desaturation (25). All these changes in pulmonary mechanics result in the obese patient having a lower functional residual capacity (FRC) and expiratory reserve volume (ERV) compared with normal weight subjects (26) with forced vital capacity (FVC), forced expired volume in one second (FEV1) and forced mid-expiratory flow reduced in the morbidly obese (27).
Sleep disordered breathing
Sleep-disordered breathing, including obstructive sleep apnoea (OSA) and obesity-related respiratory failure (ORRF), is common in obese patients (28). Studies estimate the prevalence of OSA as 2-24% of the population (29,30) with half of all patients with a BMI above 40 kg/m2 demonstrating OSA (31). Of major clinical importance, a recent meta-analysis reported that OSA is associated with a higher incidence of postoperative acute respiratory failure, cardiac events and ICU admission (32). ORRF encompasses three distinct clinical phenotypes.
Severe OSA
Chronic respiratory failure in these patients has been shown to be a consequence of a reduced hypercapnic ventilatory response at the end of an apnoeic episode (33). Patients with this clinical phenotype have insufficient post apnea hyperpnea to clear the carbon dioxide load that accumulates during the apnoea (34). Therefore, each apnea is associated with an increase in carbon dioxide load that is buffered by renal retention of bicarbonate, subsequently blunting the hypercapnic ventilator response.
Lone obesity hypoventilation syndrome (OHS)
OHS is defined as obesity (BMI ≥30 kg/m2) with daytime hypercapnia (PaCO2 >6 kPa or 45 mmHg) and sleep disordered breathing in the absence of other causes of hypoventilation (35). Recent update of the definition has extended this to include the presence of an elevated base excess or bicarbonate level which may facilitate early screening for these patients (36). The mechanism underlying OHS is not fully understood and although an imbalance between the neural respiratory drive, respiratory muscle load and respiratory muscle capacity results in alveolar hypoventilation and hypercapnia, the contribution of each has yet to be determined. In simple obesity, subjects breathe more rapidly at a lower tidal volume to reduce the respiratory muscle load and avoid hypoventilation. However, this response is absent in patients with OHS, resulting in hypoventilation. Both hypercapnic and hypoxic ventilatory challenges are blunted in OHS patients compared with simple obese patients, such that there is less ventilation for a given level of oxygen and carbon dioxide (37,38). The subsequent hypercapnia and hypoxia cause sleep fragmentation that further blunts the hypercapnic and hypoxic ventilatory response (39). The impairment of the hypercapnic ventilatory response, in particular, has been shown to correlate with the severity of nocturnal hypoventilation and improves following treatment with non-invasive ventilation (NIV) (40,41).
Combination of OSA and OHS
Up to 30% of patients with OSA have OHS (42). The mechanism of chronic respiratory failure in these patients is presumed to be a combination of a blunted hypercapnic ventilatory response at the end of an apneic episode and an imbalance between increased respiratory muscle load and reduced respiratory muscle capacity, resulting in alveolar hypoventilation.
Pre-operative assessment
Risk stratification
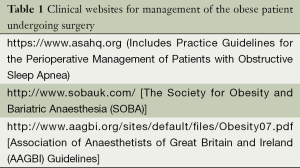
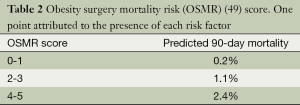
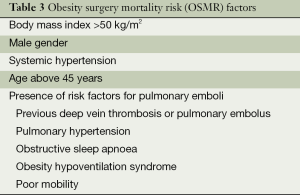
A number of recommendations are available to guide the clinician in the management of the obese patient undergoing surgery (43,44) along with a number of useful websites (see Table 1). The Association of Anaesthetists of Great Britain and Ireland guidance advises that a supine oxygen saturation of less than 96% requires consideration of a referral to a specialist respiratory physician. It has become common clinical practice to screen obese patients with a simple questionnaire that has high negative predictive value in excluding sleep disordered breathing (45). Screening for symptoms of OSA with instruments such as STOP-BANG and subsequent treatment of sleep disordered breathing has been shown to reduce the need for intensive care when managing obese patients (46). As part of the screening programme, further investigation such as clinic oxygen saturations, spirometry and overnight oximetry are considered useful. Indeed, in obese patients with oximetry proven sleep disordered breathing, defined as a 4% oxygen desaturation index above ten events per hour, the combination of reduced daytime clinic oxygen saturations (SpO2) and FVC indicates high risk of obesity related respiratory failure (47). Specifically, an FVC of less than 3.5 L in men and 2.3 L in women or a clinic SpO2 less than 95% in men and 93% in women predicts a PaCO2 of above 6.0 kPa. As part of this pre-operative assessment, review of any problems encountered during previous anesthesia is undertaken with a focus on important co-morbidities, such as ischemic heart disease and chronic heart failure and a comprehensive assessment of the upper airway to estimate the risk of a difficult intubation. Surgical risk assessment tools are available for example to help predict those at highest risk of post-operative respiratory complications (48) and a mortality risk score specifically designed for the obese patient undergoing surgery is shown in Tables 2,3 (49).
Full table
Full table
Full table
General physical condition
Cardio-pulmonary exercise testing (CPET) can identify high-risk patients and the data gained from CPET is associated with surgical outcome in non-cardiopulmonary surgery (50). McCulloch and colleagues (51) observed that in patients undergoing bariatric surgery, post-operative complications were significantly higher in the cohort with a peak oxygen consumption (O2) levels less than 15.8 mL·kg-1·min-1. In a similar study group, Hennis and colleagues found that a low anaerobic threshold (AT) was associated with postoperative morbidity and increased length of stay (52). With this in mind, and with a focus on optimizing the physical condition of the patient, the clinician may consider pre-operative training to reduce the incidence of post-operative pulmonary complications albeit the evidence for this is limited (53).
Airway assessment
Reduced neck extension and flexion combined with limited mouth opening account for the majority of the difficult airway cases encountered in obese subjects (54). Other risk factors such as morbid obesity, large neck circumference (above 43 cm) and a Mallampati score of ≥3 should alert the clinician to a difficult intubation (55,56). In addition, the reduced FRC and ERV (28) of the obese in the upright posture are further decreased by placing the patient in the supine position with the potential for rapid oxygen desaturation (57). Adequate pre-oxygenation is therefore essential (58) and if performed whilst sitting, this extends the time before oxygen desaturation (59). By optimizing the position of the patient, with head and trunk elevation, severe oxygen desaturations can be avoided. It has been reported that 75% of morbidly obese patients are grade 1 Cormack-Lehane view on direct laryngoscopy (57) with the ramped position improving oxygenation and visualization of the glottis with support provided under the head and trunk (60).
Intra-operative strategies
In morbidly obese patients, FRC decreases after induction of anesthesia by up to 50% due to atelectasis and blood shifting from abdomen to thorax (20,61,62). Increased intra-abdominal pressure transmitted in a cephalid direction towards the most dependent lung regions is coupled with decreased movement of the dependent part of the diaphragm to increase the likelihood of atelectasis (15). Indeed, atelectasis frequently persists through the postoperative period (63,64) and this contributes to the decrease in lung compliance of the respiratory system, which is more important than the fall in chest wall compliance (20).
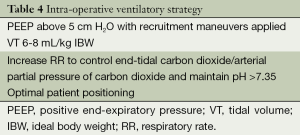
A number of techniques have been suggested to optimize ventilation intra-operatively and reduce postoperative complications and these are summarized in Table 4.
Full table
Application of extrinsic positive end expiratory pressure (PEEP)
Katz and coworkers showed that the increase in lung volume caused by application PEEP is greater than that predicted from the pressure-volume relationship at lower PEEP (65). Indeed, PEEP defends against the fall in FRC associated with administration of general anesthesia and thereby prevents or, at least, reduces lung atelectasis (66-68) with evidence that the addition of PEEP improves intra-operative respiratory function (69-71). Pelosi et al. showed that applying 10 cm H2O of PEEP resulted in improved oxygenation in morbidly obese patients, but not in normal weight subjects (72) and Azab and colleagues demonstrated PEEP reduced lung atelectasis with a reduction in post-operative pulmonary complications (73).
Extrinsic PEEP combined with recruitment maneuvers (RM)
Small airway opening can be achieved by applying intermittent hyperinflation of the lung, so called recruitment maneuvers (RM) (62). Although the clinician should avoid the associated negative haemodynamic effects, a number of recent studies suggest that the addition of PEEP in combination with RM improves oxygenation and lung compliance by reducing lung atelectasis (64,74-80). Talab and colleagues found that this intraoperative combination reduced post-operative pulmonary complications (81). Two recent large multi-centre RCTs found conflicting results for protective ventilation. The IMPROVE study (82) included 400 patients at risk of postoperative pulmonary complications undergoing major abdominal surgery demonstrated that lung protective ventilation using low tidal volumes ventilation with a PEEP of 6 to 8 cm H2O combined with RM reduced post-operative complications and shortened hospital length of stay. A recent large French multi-centre observational study of 2,960 patients found that BMI was an independent factor for the use of tidal volume of above 10 mL/kg ideal body weight (IBW) (83). Interestingly, only 25% of patients with a BMI greater than 30 kg/m2 and 35% with a BMI greater than 35 kg/m2 received additional PEEP and only 18% of the obese patients receiving RMs. A tidal volume of 6-10 mL/kg IBW and a respiratory rate to maintain normocapnia has been recommended (84,85). Finally, a recent meta-analysis (86) of three randomized studies of ventilation in obese patients, comparing pressure with volume ventilation found no difference between ventilation modes in terms of intraoperative oxygenation, tidal volume, mean airway pressure, mean arterial pressure and heart rate.
Positioning of the patient
A number of different patient positions have been reported. Valenza and colleagues showed that PEEP in combination with the ‘beach chair position’ improved oxygenation and pulmonary elastance (87) whilst the reverse Trendelenburg position mitigates against increased intra-abdominal pressure improving oxygenation and lung compliance (88,89). Lateral decubitus position, by shifting the abdominal pannus away from the diaphragm, can also decrease the intra-abdominal pressure and increase chest excursions (57).
Post-operative stage
Pulmonary complications
Obese patients are more likely to develop post-operative acute respiratory failure (90) and have higher rates of pneumonia, prolonged mechanical ventilation and weaning difficulty (58,91-95). Guidelines recommend extubating patients with existing ORRF in an awake state and to avoid the supine position (46). Indeed, the post-operative pulmonary complications are associated with increased rates of short-term and long-term mortality (96). Both upper abdominal and thoracic surgery can result in a restriction of pulmonary function that can persist for several days as a direct cause due to the reduced ability of the patient to clear secretions (64). Furthermore, the immediate post-operative period can pose an increased risk for respiratory complications in obese patients with OSA and OHS as opiate sensitivity contributes to the severity of nocturnal hypoxia (97,98). In addition, obesity increases the post-operative work of breathing (15,20) as lung atelectasis causes the patient to breath at lower lung volumes with associated early airways closure and expiratory flow limitation resulting in development of intrinsic PEEP (22,99). This is worsened further when supine (14).
Non-invasive ventilator support (CPAP and NIV)
Continuous positive airway pressure (CPAP) and NIV have been used to prevent and treat acute respiratory failure after surgery or to treat acute respiratory failure (100,101). In an ICU telephone survey in France, 69% of physicians reported to use CPAP and NIV as first line treatment in patients with post-operative acute respiratory failure (102). This is supported by a systematic review of the use of post-operative NIV and CPAP (103), of which 19 of 29 studies observed improved gas exchange, 11 reported a reduced re-intubation rate and one study showed NIV improved clinical outcome (104). CPAP provides ventilatory support to restore and maintain the lung volumes by recruiting atelectatic lung which, in turn, improves oxygenation and reduces work of breathing. Animal studies have shown that minimizing lung atelectasis decreases bacterial growth and translocation of organisms to the bloodstream by reducing the permeability of the epithelial-endothelial barrier (105,106). A meta-analysis (107) has shown that post-operative CPAP following abdominal surgery significantly reduced post pulmonary complications, atelectasis and pneumonia which is in contrast with a more recent Cochrane review concluding that the evidence to support the use of CPAP to reduces pneumonia and re-intubation is of low quality (108). However in this Cochrane review, only one study included obese patients and the review excluded use of intra-operative PEEP (109). This can be balanced against the results of a randomized controlled trial that showed applying CPAP to morbidly obese patients immediately following extubation led to improved spirometry at 24 hours compared to delaying the initiation of external CPAP to the recovery room (110).
The feasibility and safety of NIV use in the recovery room after various types of surgery has been demonstrated (106,108,111,112). One study showed a 16% absolute risk reduction in post-extubation acute respiratory failure with a reduced length of ICU stay by application of 48 hours of NIV in the immediate post-operative stage for patients with a BMI above 35 kg/m2 (113). A limitation of the study was the use of a historically matched control group (114). Although there are no clinical trials that have shown the effectiveness of NIV in the post-operative setting for the management of patients with established chronic respiratory failure it is considered the standard of care (113,115-117).
Post-operative ventilation strategy
If a patient requires extended ventilation, the clinician should give careful consideration in their decision for the most appropriate tidal volume and this should be based on ideal and not actual body weight to avoid high peak and plateau airway pressures and barotrauma. As a consequence of the effect of general anesthesia and surgery, the obese patient demonstrates lung atelectasis with a fall in lung volumes and increased airway resistance. Because of the reduced chest wall compliance of respiratory system in obesity, inflation pressures should be interpreted with caution with the initial target tidal volume calculated from the IBW and then adjusted according gas exchange (118). Pelosi and colleagues demonstrated that the addition of PEEP at 10 cm H2O in morbidly obese patients increased elastance and improved oxygenation compared with non-obese subjects (62). Of clinical relevance is that the use of a low tidal volume and a high fraction of inspired oxygen in the obese population can lead to progressive formation of atelectasis, with secondary hypoxemia and hypercapnia (119). The goal for mechanical ventilation in this patient population should focus on the use of peak inspiratory pressures high enough to open collapsed lung regions and the use of PEEP to keep the alveoli open at the end of expiration (120). ‘Safe’ peak plateau pressures in the obese patient differ from the non-obese patient as these obese patients, due to a reduced chest wall compliance, have increased pleural pressures resulting in a lower transpulmonary pressure and less lung distension. Thus, indirect measurements of transpulmonary pressures using oesophageal pressure monitoring can be useful to assist the clinician in the delivery of the ventilator strategy in the physiologically complex patients based on transpulmonary pressure measurement (121).
Respiratory physiotherapy and early mobilization
Incentive spirometry, respiratory physiotherapy, and targeted pulmonary toileting should be instituted in the immediate post-operative stage (122). Early mobilization, albeit a complex task involving a large team with an associated risk, is suggested (87). This approach is supported by a study in obese patients following major abdominal surgery, which showed that respiratory and rehabilitation physiotherapy, including coughing, deep breathing and early mobilization, reduced post-operative complications (123).
Conclusions
The respiratory management of the obese surgical patient provides a number of peri-operative challenges. There is a growing evidence base in a number of key areas, in particular, around optimal ventilation strategies to minimize the risk of immediate post-operative pulmonary complications (Table 5). The elective clinical pathway for such complex patients must be carefully considered taking into account pre-operative assessment and planning as well as peri- and post-operative management.
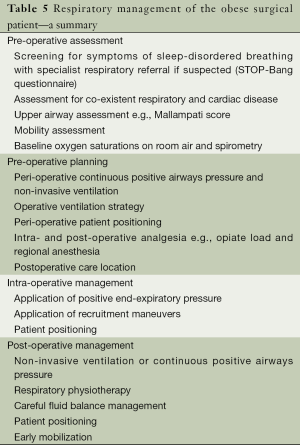
Full table
Acknowledgements
Dr. Hart has received funding from Philips, Philips-Respironics, Resmed, Fisher-Paykel, B&D Electromedical and GSK for lecture fees and research grants. Dr. Murphy has received funding from B&D Electromedical and GSK for research grants and conference attendance.
Disclosure: The authors declare no conflict of interest.
References
- Obesity and overweight. Available online: http://www.who.int/mediacentre/factsheets/fs311/en/. Accessed on 20 November 2014.
- Ng M, Fleming T, Robinson M, et al. Global, regional, and national prevalence of overweight and obesity in children and adults during 1980-2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet 2014;384:766-81. [PubMed]
- Sturm R. Increases in morbid obesity in the USA: 2000-2005. Public Health 2007;121:492-6. [PubMed]
- Butland B, Jebb S, Kopelman P, et al. editors. Tackling Obesities: Future Choices—Project report. 2nd ed. London: Foresight Programme of the Government Office for Science, 2007.
- Statistics on obesity, physical activity and diet. England: The NHS Information Centre, 2012. Available online: http://www.hscic.gov.uk/catalogue/PUB05131/obes-phys-acti-diet-eng-2012-rep.pdf
- Akinnusi ME, Pineda LA, El Solh AA. Effect of obesity on intensive care morbidity and mortality: a meta-analysis. Crit Care Med 2008;36:151-8. [PubMed]
- Friedman N, Fanning EL. Overweight and obesity: an overview of prevalence, clinical impact, and economic impact. Dis Manag 2004;7 Suppl 1:S1-6. [PubMed]
- Lewandowski K, Lewandowski M. Intensive care in the obese. Best Pract Res Clin Anaesthesiol 2011;25:95-108. [PubMed]
- Sharp JT, Henry JP, Sweany SK, et al. The total work of breathing in normal and obese men. J Clin Invest 1964;43:728-39. [PubMed]
- Zerah F, Harf A, Perlemuter L, et al. Effects of obesity on respiratory resistance. Chest 1993;103:1470-6. [PubMed]
- Kress JP, Pohlman AS, Alverdy J, et al. The impact of morbid obesity on oxygen cost of breathing (VO(2RESP)) at rest. Am J Respir Crit Care Med 1999;160:883-6. [PubMed]
- Steier J, Jolley CJ, Seymour J, et al. Neural respiratory drive in obesity. Thorax 2009;64:719-25. [PubMed]
- Pelosi P, Croci M, Ravagnan I, et al. The effects of body mass on lung volumes, respiratory mechanics, and gas exchange during general anesthesia. Anesth Analg 1998;87:654-60. [PubMed]
- Hackney JD. Syndrome of extreme obesity and hypoventilation: studies of etiology. Ann Intern Med 1959;51:541-52. [PubMed]
- Salome CM, Munoz PA, Berend N, et al. Effect of obesity on breathlessness and airway responsiveness to methacholine in non-asthmatic subjects. Int J Obes (Lond) 2008;32:502-9. [PubMed]
- Eriksen J, Andersen J, Rasmussen JP, et al. Effects of ventilation with large tidal volumes or positive end-expiratory pressure on cardiorespiratory function in anesthetized obese patients. Acta Anaesthesiol Scand 1978;22:241-8. [PubMed]
- Behazin N, Jones SB, Cohen RI, et al. Respiratory restriction and elevated pleural and esophageal pressures in morbid obesity. J Appl Physiol (1985) 2010;108:212-8. [PubMed]
- Pelosi P, Croci M, Ravagnan I, et al. Total respiratory system, lung, and chest wall mechanics in sedated-paralyzed postoperative morbidly obese patients. Chest 1996;109:144-51. [PubMed]
- Ferretti A, Giampiccolo P, Cavalli A, et al. Expiratory flow limitation and orthopnea in massively obese subjects. Chest 2001;119:1401-8. [PubMed]
- Pankow W, Podszus T, Gutheil T, et al. Expiratory flow limitation and intrinsic positive end-expiratory pressure in obesity. J Appl Physiol (1985) 1998;85:1236-43. [PubMed]
- Holley HS, Milic-Emili J, Becklake MR, et al. Regional distribution of pulmonary ventilation and perfusion in obesity. J Clin Invest 1967;46:475-81. [PubMed]
- King GG, Brown NJ, Diba C, et al. The effects of body weight on airway calibre. Eur Respir J 2005;25:896-901. [PubMed]
- Malhotra A, Hillman D. Obesity and the lung: 3. Obesity, respiration and intensive care. Thorax 2008;63:925-31. [PubMed]
- Steier J, Lunt A, Hart N, et al. Observational study of the effect of obesity on lung volumes. Thorax 2014;69:752-9. [PubMed]
- Damia G, Mascheroni D, Croci M, et al. Perioperative changes in functional residual capacity in morbidly obese patients. Br J Anaesth 1988;60:574-8. [PubMed]
- Rubinstein I, Zamel N, DuBarry L, et al. Airflow limitation in morbidly obese, nonsmoking men. Ann Intern Med 1990;112:828-32. [PubMed]
- Littleton SW. Impact of obesity on respiratory function. Respirology 2012;17:43-9. [PubMed]
- Mandal S, Hart N. Respiratory complications of obesity. Clin Med 2012;12:75-8. [PubMed]
- Young T, Palta M, Dempsey J, et al. The occurrence of sleep-disordered breathing among middle-aged adults. N Engl J Med 1993;328:1230-5. [PubMed]
- Young T, Peppard PE, Taheri S. Excess weight and sleep-disordered breathing. J Appl Physiol (1985) 2005;99:1592-9. [PubMed]
- Resta O, Foschino-Barbaro MP, Legari G, et al. Sleep-related breathing disorders, loud snoring and excessive daytime sleepiness in obese subjects. Int J Obes Relat Metab Disord 2001;25:669-75. [PubMed]
- Kaw R, Chung F, Pasupuleti V, et al. Meta-analysis of the association between obstructive sleep apnoea and postoperative outcome. Br J Anaesth 2012;109:897-906. [PubMed]
- Garay SM, Rapoport D, Sorkin B, et al. Regulation of ventilation in the obstructive sleep apnea syndrome. Am Rev Respir Dis 1981;124:451-7. [PubMed]
- Berger KI, Goldring RM, Rapoport DM. Obesity hypoventilation syndrome. Semin Respir Crit Care Med 2009;30:253-61. [PubMed]
- Piper AJ, Grunstein RR. Obesity hypoventilation syndrome: mechanisms and management. Am J Respir Crit Care Med 2011;183:292-8. [PubMed]
- Hart N, Mandal S, Manuel A, et al. Obesity hypoventilation syndrome: does the current definition need revisiting? Thorax 2014;69:83-4. [PubMed]
- Sampson MG, Grassino K. Neuromechanical properties in obese patients during carbon dioxide rebreathing. Am J Med 1983;75:81-90. [PubMed]
- Jokic R, Zintel T, Sridhar G, et al. Ventilatory responses to hypercapnia and hypoxia in relatives of patients with the obesity hypoventilation syndrome. Thorax 2000;55:940-5. [PubMed]
- White DP, Douglas NJ, Pickett CK, et al. Sleep deprivation and the control of ventilation. Am Rev Respir Dis 1983;128:984-6. [PubMed]
- Chouri-Pontarollo N, Borel JC, Tamisier R, et al. Impaired objective daytime vigilance in obesity-hypoventilation syndrome: impact of noninvasive ventilation. Chest 2007;131:148-55. [PubMed]
- de Lucas-Ramos P, de Miguel-Díez J, Santacruz-Siminiani A, et al. Benefits at 1 year of nocturnal intermittent positive pressure ventilation in patients with obesity-hypoventi lation syndrome. Respir Med 2004;98:961-7. [PubMed]
- Mokhlesi B, Tulaimat A, Faibussowitsch I, et al. Obesity hypoventilation syndrome: prevalence and predictors in patients with obstructive sleep apnea. Sleep Breath 2007;11:117-24. [PubMed]
- Chambers WA, Beckwith P, Bellamy M, et al. editors. Peri-operative management of the morbidly obese patient. London: The Association of Anaesthetists of Great Britain and Ireland, 2007.
- Practice guidelines for the perioperative management of patients with obstructive sleep apnea: an updated report by the American Society of Anesthesiologists Task Force on Perioperative Management of patients with obstructive sleep apnea. Anesthesiology 2014;120:268-86. [PubMed]
- Chung F, Yegneswaran B, Liao P, et al. STOP questionnaire: a tool to screen patients for obstructive sleep apnea. Anesthesiology 2008;108:812-21. [PubMed]
- Hallowell PT, Stellato TA, Petrozzi MC, et al. Eliminating respiratory intensive care unit stay after gastric bypass surgery. Surgery 2007;142:608-12; discussion 612.e1.
- Mandal S, Suh ES, Boleat E, et al. A cohort study to identify simple clinical tests for chronic respiratory failure in obese patients with sleep-disordered breathing. BMJ Open Respir Res 2014;1:e000022. [PubMed]
- Canet J, Gallart L, Gomar C, et al. Prediction of postoperative pulmonary complications in a population-based surgical cohort. Anesthesiology 2010;113:1338-50. [PubMed]
- DeMaria EJ, Murr M, Byrne TK, et al. Validation of the obesity surgery mortality risk score in a multicenter study proves it stratifies mortality risk in patients undergoing gastric bypass for morbid obesity. Ann Surg 2007;246:578-82; discussion 583-4. [PubMed]
- Hennis PJ, Meale PM, Grocott MP. Cardiopulmonary exercise testing for the evaluation of perioperative risk in non-cardiopulmonary surgery. Postgrad Med J 2011;87:550-7. [PubMed]
- McCullough PA, Gallagher MJ, Dejong AT, et al. Cardiorespiratory fitness and short-term complications after bariatric surgery. Chest 2006;130:517-25. [PubMed]
- Hennis PJ, Meale PM, Hurst RA, et al. Cardiopulmonary exercise testing predicts postoperative outcome in patients undergoing gastric bypass surgery. Br J Anaesth 2012;109:566-71. [PubMed]
- Hulzebos EH, Smit Y, Helders PP, et al. Preoperative physical therapy for elective cardiac surgery patients. Cochrane Database Syst Rev 2012;11:CD010118. [PubMed]
- Williamson JA, Webb RK, Szekely S, et al. The Australian Incident Monitoring Study. Difficult intubation: an analysis of 2000 incident reports. Anaesth Intensive Care 1993;21:602-7. [PubMed]
- Brodsky JB, Lemmens HJ, Brock-Utne JG, et al. Morbid obesity and tracheal intubation. Anesth Analg 2002;94:732-6. [PubMed]
- Lundstrøm LH, Møller AM, Rosenstock C, et al. High body mass index is a weak predictor for difficult and failed tracheal intubation: a cohort study of 91,332 consecutive patients scheduled for direct laryngoscopy registered in the Danish Anesthesia Database. Anesthesiology 2009;110:266-74. [PubMed]
- El-Solh AA. Clinical approach to the critically ill, morbidly obese patient. Am J Respir Crit Care Med 2004;169:557-61. [PubMed]
- Rao SL, Kunselman AR, Schuler HG, et al. Laryngoscopy and tracheal intubation in the head-elevated position in obese patients: a randomized, controlled, equivalence trial. Anesth Analg 2008;107:1912-8. [PubMed]
- Altermatt FR, Muñoz HR, Delfino AE, et al. Pre-oxygenation in the obese patient: effects of position on tolerance to apnoea. Br J Anaesth 2005;95:706-9. [PubMed]
- Kristensen MS. Airway management and morbid obesity. Eur J Anaesthesiol 2010;27:923-7. [PubMed]
- Smetana GW. Preoperative pulmonary evaluation. N Engl J Med 1999;340:937-44. [PubMed]
- Reinius H, Jonsson L, Gustafsson S, et al. Prevention of atelectasis in morbidly obese patients during general anesthesia and paralysis: a computerized tomography study. Anesthesiology 2009;111:979-87. [PubMed]
- Lindberg P, Gunnarsson L, Tokics L, et al. Atelectasis and lung function in the postoperative period. Acta Anaesthesiol Scand 1992;36:546-53. [PubMed]
- Eichenberger A, Proietti S, Wicky S, et al. Morbid obesity and postoperative pulmonary atelectasis: an underestimated problem. Anesth Analg 2002;95:1788-92. [PubMed]
- Katz JA, Ozanne GM, Zinn SE, et al. Time course and mechanisms of lung-volume increase with PEEP in acute pulmonary failure. Anesthesiology 1981;54:9-16. [PubMed]
- Brismar B, Hedenstierna G, Lundquist H, et al. Pulmonary densities during anesthesia with muscular relaxation--a proposal of atelectasis. Anesthesiology 1985;62:422-8. [PubMed]
- Neumann P, Rothen HU, Berglund JE, et al. Positive end-expiratory pressure prevents atelectasis during general anaesthesia even in the presence of a high inspired oxygen concentration. Acta Anaesthesiol Scand 1999;43:295-301. [PubMed]
- Tokics L, Hedenstierna G, Strandberg A, et al. Lung collapse and gas exchange during general anesthesia: effects of spontaneous breathing, muscle paralysis, and positive end-expiratory pressure. Anesthesiology 1987;66:157-67. [PubMed]
- Clarke JP, Schuitemaker MN, Sleigh JW. The effect of intraoperative ventilation strategies on perioperative atelectasis. Anaesth Intensive Care 1998;26:262-6. [PubMed]
- Maracajá-Neto LF, Verçosa N, Roncally AC, et al. Beneficial effects of high positive end-expiratory pressure in lung respiratory mechanics during laparoscopic surgery. Acta Anaesthesiol Scand 2009;53:210-7. [PubMed]
- Meininger D, Byhahn C, Mierdl S, et al. Positive end-expiratory pressure improves arterial oxygenation during prolonged pneumoperitoneum. Acta Anaesthesiol Scand 2005;49:778-83. [PubMed]
- Pelosi P, Ravagnan I, Giurati G, et al. Positive end-expiratory pressure improves respiratory function in obese but not in normal subjects during anesthesia and paralysis. Anesthesiology 1999;91:1221-31. [PubMed]
- Azab T, El-Masry A, Salah M, et al. Effects of intraoperative use of positive end expiratory pressure on lung atelectasis during laparoscopic cholecystectomy. Egyptian J Anaesthesia 2005;21:219-25.
- Dyhr T, Nygård E, Laursen N, et al. Both lung recruitment maneuver and PEEP are needed to increase oxygenation and lung volume after cardiac surgery. Acta Anaesthesiol Scand 2004;48:187-97. [PubMed]
- Tusman G, Böhm SH, Suarez-Sipmann F, et al. Alveolar recruitment improves ventilatory efficiency of the lungs during anesthesia. Can J Anaesth 2004;51:723-7. [PubMed]
- Maisch S, Reissmann H, Fuellekrug B, et al. Compliance and dead space fraction indicate an optimal level of positive end-expiratory pressure after recruitment in anesthetized patients. Anesth Analg 2008;106:175-81. [PubMed]
- de Souza AP, Buschpigel M, Mathias LA, et al. Analysis of the effects of the alveolar recruitment maneuver on blood oxygenation during bariatric surgery. Rev Bras Anestesiol 2009;59:177-86. [PubMed]
- Tafer N, Nouette-Gaulain K, Richebé P, et al. Effectiveness of a recruitment manoeuvre and positive end-expiratory pressure on respiratory mechanics during laparoscopic bariatric surgery. Ann Fr Anesth Reanim 2009;28:130-4. [PubMed]
- Futier E, Constantin JM, Pelosi P, et al. Intraoperative recruitment maneuver reverses detrimental pneumoperitoneum-induced respiratory effects in healthy weight and obese patients undergoing laparoscopy. Anesthesiology 2010;113:1310-9. [PubMed]
- Futier E, Constantin JM, Pelosi P, et al. Noninvasive ventilation and alveolar recruitment maneuver improve respiratory function during and after intubation of morbidly obese patients: a randomized controlled study. Anesthesiology 2011;114:1354-63. [PubMed]
- Talab HF, Zabani IA, Abdelrahman HS, et al. Intraoperative ventilatory strategies for prevention of pulmonary atelectasis in obese patients undergoing laparoscopic bariatric surgery. Anesth Analg 2009;109:1511-6. [PubMed]
- Futier E, Constantin JM, Paugam-Burtz C, et al. A trial of intraoperative low-tidal-volume ventilation in abdominal surgery. N Engl J Med 2013;369:428-37. [PubMed]
- Jaber S, Coisel Y, Chanques G, et al. A multicentre observational study of intra-operative ventilatory management during general anaesthesia: tidal volumes and relation to body weight. Anaesthesia 2012;67:999-1008. [PubMed]
- Schultz MJ, Haitsma JJ, Slutsky AS, et al. What tidal volumes should be used in patients without acute lung injury? Anesthesiology 2007;106:1226-31. [PubMed]
- Pelosi P, Gregoretti C. Perioperative management of obese patients. Best Pract Res Clin Anaesthesiol 2010;24:211-25. [PubMed]
- Aldenkortt M, Lysakowski C, Elia N, et al. Ventilation strategies in obese patients undergoing surgery: a quantitative systematic review and meta-analysis. Br J Anaesth 2012;109:493-502. [PubMed]
- Valenza F, Vagginelli F, Tiby A, et al. Effects of the beach chair position, positive end-expiratory pressure, and pneumoperitoneum on respiratory function in morbidly obese patients during anesthesia and paralysis. Anesthesiology 2007;107:725-32. [PubMed]
- Perilli V, Sollazzi L, Bozza P, et al. The effects of the reverse trendelenburg position on respiratory mechanics and blood gases in morbidly obese patients during bariatric surgery. Anesth Analg 2000;91:1520-5. [PubMed]
- Perilli V, Sollazzi L, Modesti C, et al. Comparison of positive end-expiratory pressure with reverse Trendelenburg position in morbidly obese patients undergoing bariatric surgery: effects on hemodynamics and pulmonary gas exchange. Obes Surg 2003;13:605-9. [PubMed]
- Newell MA, Bard MR, Goettler CE, et al. Body mass index and outcomes in critically injured blunt trauma patients: weighing the impact. J Am Coll Surg 2007;204:1056-61; discussion 1062-4. [PubMed]
- El-Solh A, Sikka P, Bozkanat E, et al. Morbid obesity in the medical ICU. Chest 2001;120:1989-97. [PubMed]
- Sakr Y, Madl C, Filipescu D, et al. Obesity is associated with increased morbidity but not mortality in critically ill patients. Intensive Care Med 2008;34:1999-2009. [PubMed]
- Frat JP, Gissot V, Ragot S, et al. Impact of obesity in mechanically ventilated patients: a prospective study. Intensive Care Med 2008;34:1991-8. [PubMed]
- Bamgbade OA, Rutter TW, Nafiu OO, et al. Postoperative complications in obese and nonobese patients. World J Surg 2007;31:556-60; discussion 561. [PubMed]
- Martino JL, Stapleton RD, Wang M, et al. Extreme obesity and outcomes in critically ill patients. Chest 2011;140:1198-206. [PubMed]
- Khuri SF, Henderson WG, DePalma RG, et al. Determinants of long-term survival after major surgery and the adverse effect of postoperative complications. Ann Surg 2005;242:326-41; discussion 341-3. [PubMed]
- Taylor S, Kirton OC, Staff I, et al. Postoperative day one: a high risk period for respiratory events. Am J Surg 2005;190:752-6. [PubMed]
- Doufas AG, Tian L, Padrez KA, et al. Experimental pain and opioid analgesia in volunteers at high risk for obstructive sleep apnea. PLoS One 2013;8:e54807. [PubMed]
- Koutsoukou A, Koulouris N, Bekos B, et al. Expiratory flow limitation in morbidly obese postoperative mechanically ventilated patients. Acta Anaesthesiol Scand 2004;48:1080-8. [PubMed]
- Ferreyra G, Long Y, Ranieri VM. Respiratory complications after major surgery. Curr Opin Crit Care 2009;15:342-8. [PubMed]
- Jaber S, Chanques G, Jung B. Postoperative noninvasive ventilation. Anesthesiology 2010;112:453-61. [PubMed]
- Chanques G, Jaber S, Delay JM, et al. Phoning study about postoperative practice and application of non-invasive ventilation. Ann Fr Anesth Reanim 2003;22:879-85. [PubMed]
- Chiumello D, Chevallard G, Gregoretti C. Non-invasive ventilation in postoperative patients: a systematic review. Intensive Care Med 2011;37:918-29. [PubMed]
- Auriant I, Jallot A, Hervé P, et al. Noninvasive ventilation reduces mortality in acute respiratory failure following lung resection. Am J Respir Crit Care Med 2001;164:1231-5. [PubMed]
- Duggan M, McCaul CL, McNamara PJ, et al. Atelectasis causes vascular leak and lethal right ventricular failure in uninjured rat lungs. Am J Respir Crit Care Med 2003;167:1633-40. [PubMed]
- van Kaam AH, Lachmann RA, Herting E, et al. Reducing atelectasis attenuates bacterial growth and translocation in experimental pneumonia. Am J Respir Crit Care Med 2004;169:1046-53. [PubMed]
- Ferreyra GP, Baussano I, Squadrone V, et al. Continuous positive airway pressure for treatment of respiratory complications after abdominal surgery: a systematic review and meta-analysis. Ann Surg 2008;247:617-26. [PubMed]
- Battisti A, Michotte JB, Tassaux D, et al. Non-invasive ventilation in the recovery room for postoperative respiratory failure: a feasibility study. Swiss Med Wkly 2005;135:339-43. [PubMed]
- Ireland CJ, Chapman TM, Mathew SF, et al. Continuous positive airway pressure (CPAP) during the postoperative period for prevention of postoperative morbidity and mortality following major abdominal surgery. Cochrane Database Syst Rev 2014;8:CD008930. [PubMed]
- Neligan PJ, Malhotra G, Fraser M, et al. Continuous positive airway pressure via the Boussignac system immediately after extubation improves lung function in morbidly obese patients with obstructive sleep apnea undergoing laparoscopic bariatric surgery. Anesthesiology 2009;110:878-84. [PubMed]
- Joris JL, Sottiaux TM, Chiche JD, et al. Effect of bi-level positive airway pressure (BiPAP) nasal ventilation on the postoperative pulmonary restrictive syndrome in obese patients undergoing gastroplasty. Chest 1997;111:665-70. [PubMed]
- Jaber S, Delay JM, Chanques G, et al. Outcomes of patients with acute respiratory failure after abdominal surgery treated with noninvasive positive pressure ventilation. Chest 2005;128:2688-95. [PubMed]
- Pérez de Llano LA, Golpe R, Ortiz Piquer M, et al. Short-term and long-term effects of nasal intermittent positive pressure ventilation in patients with obesity-hypoventilation syndrome. Chest 2005;128:587-94. [PubMed]
- El-Solh AA, Aquilina A, Pineda L, et al. Noninvasive ventilation for prevention of post-extubation respiratory failure in obese patients. Eur Respir J 2006;28:588-95. [PubMed]
- Carrillo A, Ferrer M, Gonzalez-Diaz G, et al. Noninvasive ventilation in acute hypercapnic respiratory failure caused by obesity hypoventilation syndrome and chronic obstructive pulmonary disease. Am J Respir Crit Care Med 2012;186:1279-85. [PubMed]
- Priou P, Hamel JF, Person C, et al. Long-term outcome of noninvasive positive pressure ventilation for obesity hypoventilation syndrome. Chest 2010;138:84-90. [PubMed]
- Masa JF, Celli BR, Riesco JA, et al. The obesity hypoventilation syndrome can be treated with noninvasive mechanical ventilation. Chest 2001;119:1102-7. [PubMed]
- Marik P, Varon J. The obese patient in the ICU. Chest 1998;113:492-8. [PubMed]
- Rothen HU, Sporre B, Engberg G, et al. Influence of gas composition on recurrence of atelectasis after a reexpansion maneuver during general anesthesia. Anesthesiology 1995;82:832-42. [PubMed]
- Pelosi P, Luecke T, Caironi P. Respiratory Management in Obese Patients. In: Gullo A. editors. Anaesthesia, Pain, Intensive Care and Emergency Medicine—A.P.I.C.E. Milan: Springer Milan, 2005:379-94.
- Akoumianaki E, Maggiore SM, Valenza F, et al. The application of esophageal pressure measurement in patients with respiratory failure. Am J Respir Crit Care Med 2014;189:520-31. [PubMed]
- Torrington KG, Sorenson DE, Sherwood LM. Postoperative chest percussion with postural drainage in obese patients following gastric stapling. Chest 1984;86:891-5. [PubMed]
- Fagevik Olsén M, Hahn I, Nordgren S, et al. Randomized controlled trial of prophylactic chest physiotherapy in major abdominal surgery. Br J Surg 1997;84:1535-8. [PubMed]


