Restrictive pulmonary deficit is associated with inflammation in sub-optimally controlled obese diabetics
Introduction
A growing body of evidence links low-grade systemic inflammation with the metabolic syndrome, diabetes mellitus and reduced pulmonary function. Among the multiple factors that appear to be associated with diabetes mellitus, studies suggest abnormal lung function is present in individuals with diabetes (1,2). A three year follow-up of The Atherosclerosis Risk in Communities (ARIC) Study (3), demonstrated that the reduction in forced vital capacity (FVC) was swifter in diabetic adults than in their non-diabetic counterparts. The rate of decline was related to the severity of diabetes, lending sound support to the hypothesis that the lung is a target organ for injury from diabetic disease.
The NHANES Study revealed the prevalence of diabetes mellitus and the metabolic syndrome significantly increased as the predicted FVC decreased and every 10% reduction in FVC was associated with 77% higher mortality in people with the metabolic syndrome (4). Systemic inflammation in these patients, estimated by C-reactive protein (CRP) was inversely related to FVC (5). In another report (6) on 9,500 apparently healthy non-smoking Korean males, those in the lowest FVC or FEV1 quartile had the highest hs-CRP (high sensitivity-CRP) levels. The metabolic syndrome, insulin resistance and systemic inflammation were important risk factors for reduced lung function in this study. Dahl et al. (7) measured serum CRP in subjects with airway obstruction and found that hospitalization or death due to chronic obstructive pulmonary disease (COPD) were both increased in subjects with increased baseline serum CRP levels. In patients with declining FEV1 and airways obstruction, serum CRP was also a stronger and independent predictor of COPD mortality than of COPD hospitalization. Collectively, these studies suggest CRP is a surrogate marker of lung injury in the chronic diseases studied. Such relationships have not been explored in the West Indian populace, which is afflicted with high prevalence and morbidity of diabetes. In our earlier studies we found that forced expiratory volume (FEV1) (8) was reduced in in-patients with vascular disease, an important outcome measure in diabetics, and observed a similar relationship for FVC in outpatients attending chronic disease clinics in Trinidad (9).
In countries of the Caribbean Community Market (CARICOM) the age adjusted death rate for diabetes in 2000 was >100 per 100,000, compared with less than 20 per 100,000 from Canada and the USA. Across the Caribbean, the overall prevalence of diabetes mellitus is estimated at about 9% (10) and in Trinidad and Tobago, it is 12.7% (11). Trinidad and Tobago, where life style and socio-economic changes have transformed the health profile of the population, portrays a model of the climbing health threat, prevalence and societal burden of NIDDM for the Caribbean (12,13). The interrelationship between pulmonary involvement and low grade inflammation studied elsewhere (14,15), has not been examined in the Caribbean where diabetes presents a significant health burden. We cross-sectionally examined the relationship between systemic inflammation, evaluated by hs-CRP, lung function and type 2 diabetes in Trinidad.
Methods and subjects
The Ethics Committee of The University of The West Indies (St. Augustine) approved the study, and participants gave written, informed consent.
This was a cross sectional study in 109 known adult diabetics attending two endocrinology clinics in north-central Trinidad. These clinics receive patient referrals from all over the island and even from Tobago, the sister isle, for specialist attention to control diabetes or arrest its complications. Patients were recruited as they presented to the clinics.
Adult (>17 years) type 2 diabetic patients of both genders were invited to participate. A diabetic patient was defined as one whose fasting plasma glucose was >126 mg/dL, attending a Diabetic Clinic and receiving prescribed treatment for the condition. Patients were evaluated for the presence of the Metabolic Syndrome using criteria of the International Diabetes Federation (16). Patients who were receiving exogenous corticosteroids, including inhaled steroids or those in whom spirometry could not be performed using ATS criteria (17) were excluded.
On Encounter 1, subjects were interviewed to document demography, family and smoking history, and examined for anthropometric measurements using a stadiometer and calibrated weights, waist circumference (midway between the lower rib margin and iliac crest), BMI and blood pressure. Blood was collected for estimation of hs-CRP, lipid profile, HbA1c, and uric acid. All biochemical tests (including crp) were conducted with the Vitros 250 Clinical Chemistry Analyzer (Johnson & Johnson Vitros 250, Ortho-Clinical Diagnostics Inc., Rochester NY 14626, USA), with the appropriate quality controls. Analysis of CRP was done using dry chemistry kits with a detection limit of 0.70 mg/dL. Subjects were examined for acanthosis nigricans, a surrogate marker of hyper-insulinemia, which was graded for severity on the neck using the scale described by Burke et al. (18).
On Encounter 2, one week later, lung function was assessed 20 minutes after inhaling 200 µgm salbutamol, following the ATS criteria for methodology and equipment (17). Responses from at least three technically satisfactory curves from three acceptable blows were considered. A post-bronchodilator FEV1/FVC <0.7 informed on the diagnosis of obstructive lung disease and less than 80% predicted FVC was indicative of a restrictive ventilatory defect. Post-bronchodilator spirometric indices were assessed according to the guidelines of the American Thoracic Society by open-circuit testing. Data included in the analysis satisfied the parameters of acceptability and reproducibility (17) and predicted values were calculated using Hankinson equations (19).
Using the method described by Brown et al. (20), steroid sensitivity of the skin was assayed on this occasion with beclomethasone dipropionate dissolved in 95% ethanol (1,000 μgm/mL); 95% ethanol was the control. Test or control (10 μL) solutions were randomly applied to two test sites on the flexor aspect of the middle third of the forearm, in 2 cm diameter markings cut on double-sided adhesive tape. After complete drying, the site was occluded with ‘Saran’ wrap for sixteen hours. Two trained ‘blinded’ observers examined both sites for blanching under fluorescent light and the average reading was considered. Gradation of blanching was scored on a 5 point scale from 0-4, for normal skin/no blanching, faint, obvious, intense, and intense blanching beyond the circumscribed test area respectively. The absence of a blanching response after steroid application indicates an inflammatory state is present, obliterating the topical pharmacodynamic steroid effect, resulting in cutaneous steroid insensitivity.
Stastical analysis
Data was analysed using SPSS version 12. Data for continuous variables were expressed as means [standard deviation (SD); Standard Error (SE) or 95% Confidence Interval (95% CI)] and discrete data were summarized as number (%). Associations were considered statistically significant at the 5% level. For purposes of analysis acanthosis nigricans was binary coded as 0 or one vs. two to four. Skin vasoconstrictor assay was binary coded to no response vs. any response.
Residual pulmonary function was determined by subtracting the predicted from the measured value; negative values thus reflect pulmonary function less than expected as suggested in the Framingham Study (2). Univariate relationships with residual lung function measures were examined by Pearson’s correlation.
A generalized univariate linear model was constructed with hsCRP as outcome variable. All variables having significant univariate relationship with hsCRP were included in the model. Though gender was related to some of the baseline variables it was not related to hs-CRP and its inclusion in the multivariate model with hs-CRP as outcome variables did not change the outcome and so we show the data without inclusion of gender in the model. Acanthosis nigricans and skin vasoconstrictor response were included in the model as fixed factors, all other independent variables were included as covariates. The model test of significance was P=0.002.
Results
Sample description
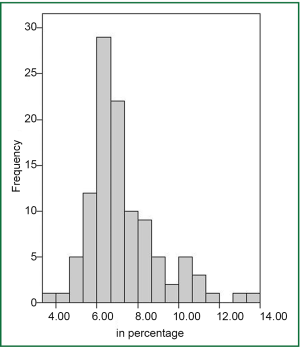
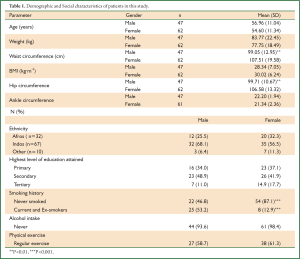
Two of the 109 subjects who gave written consent for the study, could not do the skin vasoconstrictor assay, thus analyses for this assay are for 107 patients. The majority (61.5%) of subjects were of African descent. The mean (SD) age of the population was 55.6 (11.2) years and comprised 56.88% women (Table 1).About one third (33%) of subjects were ex- or current smokers. The mean BMI (29.29 kilogram/m2) and waist circumference (103.86 cm) were high in the sample studied. The mean systolic and diastolic blood pressures were within the normal range as were mean lipid and mean uric acid levels (Table 2). Based on the IDF criteria (16) of HbA1c ≤6.5, glucose control was sub-optimal in 63.9% of subjects (Figure 1); HbA1c was greater than 8% in 25 percent of patients. In 25% of subjects the hs-CRP was greater than 5 mg/L.
Full Table

Full Table
Using the IDF Criteria 104 (95.4%) patients had central obesity, 61 (55.96%) had hypertension, 28 (25.4%) had high serum triglyceride levels and 61 (56%) had low HDL and 83.5% of subjects (n=91) suffered with the metabolic syndrome. Half the sample (50.05%) exhibited grade two-four acanthosis nigricans and 55% of subjects failed to respond to the skin vasoconstrictor assay (Table 2).
Social factors
Only 16.5% of the sample had tertiary education and only 13.7% had an annual income exceeding 10, 000 TT dollars (about $1587 USD). Most patients were non-smokers and denied alcohol consumption. A fairly large subset (39.4%) did not exercise daily or did so irregularly. Patients with a lower annual income were more likely to be smokers (P=0.023). Smokers were more likely to be male and have a lower level of education and lower hip circumference (P<0.05 in all cases). Patients who exercised daily were less likely to report alcohol drinking (P=0.012) and have a family history of cancer (P=0.018).
Lung function
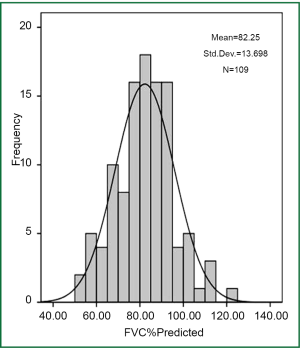
The mean post bronchodilator FVC was 2.56L and mean (SD) FEV1/FVC % was 85.13 (5.10). In 41.3% of subjects the post bronchodilator FVC was less than 80% predicted, and in 6.4% of subjects the FVC was less than 60% (Figure 2).
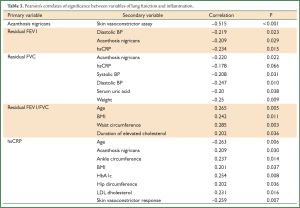
Lung function and inflammation
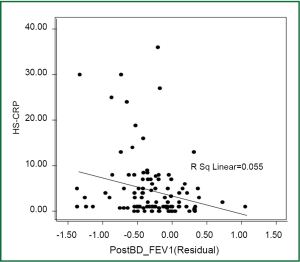
Table 3 shows the correlates of lung function and acanthosis with inflammation and variables of the metabolic syndrome. Diastolic blood pressure and hs-CRP were both inversely related to residual FEV1. Though acanthosis nigricans was related to both residual FEV1 and residual FVC, a generalized multivariate linear modeling with residual FEV1 and residual FVC as outcome variables did not elicit a statistically significant relationship with acanthosis nigricans or the skin vasoconstrictor assay. Higher levels of residual FVC were related to lower hs-CRP, and also to lower systolic and diastolic BP, lower serum uric acid and weight. The residual FEV1 value showed a similar relationship to lower hs-CRP and lower diastolic blood pressure. The FEV1/FVC ratio was higher with older age, greater BMI, greater waist circumference and longer history of hypercholesterolaemia.
Full Table
The inverse relationship of hs-CRP with post-bronchodilator residual bronchodilator FEV1 in Figure 3 draws attention to poor lung function in the presence of systemic inflammation. The high hs-CRP was associated with low residual FEV1 (Figure 3) and a tendency toward a lower residual FVC. Reduced lung function consequent to inflammation in diabetic patients was also demonstrated by the inverse association between acanthosis nigricans and residual post bronchodilator FVC (P=0.048). The systemic inflammation in patients evidenced by an absent vasoconstrictor response to topical steroid correlated negatively with acanthosis nigricans (rho=–0.515, P<0.001).
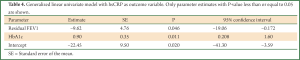
In Table 4 the generalized linear univariate model with hs-CRP as outcome variable shows that hs-CRP was significantly related to residual FEV1 and HbA1C. The adjusted grand mean hs-CRP for the patients in this study was 4.19 (95% CI: 2.72 to 5.67) mg/L. Based on these data, high HbA1C and low residual FEV1 are predictors of elevated hs-CRP in diabetic patients. Only those variables which had a significant univariate relationship to hs-CRP were included in the multivariate analysis.
Full Table
Discussion
In this cross sectional study in 109 Type 2 diabetic adults with central obesity, the first West Indian report that looks at pulmonary function in diabetics, we found that 83.5% of subjects had the metabolic syndrome. The Caribbean countries are populated by an integration of peoples drawn from the Indian subcontinent, West Africa, and China, and this populace mix is now seen in diasporas internationally. Despite the high prevalence of diabetes in the Caribbean community, to our knowledge its association with pulmonary function has not been studied in this region.
A restrictive ventilatory defect was observed in 41.3% of subjects in whom postbronchodilator FVC was <80% predicted. Residual FVC was negatively related to hs-CRP, systolic and diastolic BP, and weight and residual FEV1 showed a similar relationship to hs-CRP and diastolic blood pressure. Residual FEV1 and HbA1C were significantly related to hs-CRP and acanthosis nigricans was negatively correlated with skin vasoconstriction. The findings suggest that obese diabetic patients in Trinidad have low-grade systemic inflammation which is associated with restrictive pulmonary disease.
Lifestyle changes, sedentary work patterns, coincident increases in dietary, alcohol, and tobacco indiscretions influence the onset of the metabolic syndrome, which is demonstrated by the combined associated presence of hyperinsulinemia, obesity and hypertension. Lower income and educational level in the subjects under study was more likely to be associated with smokers, a pattern observed in a world health survey of social determinants of smoking in 48 low-income and middle-income countries (21). The population in this study was treatment responsive for dysplipidemia, hyperuricemia and hypertension, but exhibited high BMI, an excess visceral adipose tissue compartment (increased waist circumference is the clinical correlate) and dysglycemia, all of which encourage insulin resistance and fuels an underlying state of systemic inflammation (22). Guided by earlier reports (23,24) of an absent or markedly diminished response of skin vasoconstriction to a topical glucocorticosteroid we used a failed skin vasoconstriction response as a surrogate non-invasive marker of systemic inflammation secondary to insulin resistance. Our earlier findings in West Indian diabetics established that inflammation (demonstrated by hs-CRP) was associated with high grade acanthosis nigricans (25). This report also showed that high grade acanthosis nigricans was inversely related to a low grade skin vasoconstrictor response supporting the current findings of insensitive steroid induced cutaneous vasoconstriction. The failure of skin blanching presents evidence of an underlying inflammatory state associated with glucocorticoid resistance which could have either provoked it or been derived from it. The high waist circumference and BMI (representative of body fat) is indicative of insulin resistance (26), and points to the co-existent glucocorticoid and insulin resistance as concurrent metabolic co-morbidities.
Diabetics in our study were obese with sub-optimal glucose control and had low predictive FVC which was inversely related to acanthosis nigricans, the surrogate marker of insulin resistance From the inverse relationship of post bronchodilator residual FEV1 with hs-CRP, systemic inflammation is associated with abnormal pulmonary function in obese diabetic patients. Assays of hs-CRP establish it is a robust marker demonstrating the temporal relation between lung function decline and systemic inflammation (15,27). Dennis et al. (28) showed mean residual FEV1 and FVC values were lower, FEV1/FVC ratios were higher and inflammatory markers were significantly increased in diabetics without adequate control when compared with those who were well controlled. This report together with the data of Ford and Mannino (1) and the report by Yeh et al. (3), strengthens our findings that poorly controlled diabetics have a restrictive lung disorder. The mean FEV1/FVC% and mean FVC% were well below the predicted values and consistent with a restrictive ventilatory defect. In a prospective study by Wannamethee and colleagues (29) of 4,434 British men, lung function was significantly and inversely associated with C-reactive protein and interleukin-6. These authors reported an association between restrictive impaired lung function with incident type 2 diabetes, and partially attributed these findings to metabolic risk factors and inflammation. Chronic hyperglycemia promotes the formation of oxygen radicals which impair pulmonary microvasculature, alveolar epithelial basal lamina and capillary membranes (30). These inflammatory mediators potentially provoke ensuing systemic inflammation in diabetic patients who are in an altered metabolic state (31). We propose that low-grade systemic inflammation evidenced by high hs-CRP links restrictive lung function and obesity in diabetic patients who do not have optimal disease control.
Low FVC and FEV1 measures have been reported in adult diabetics (32) and in comparison with their non-diabetic counterparts (8). However we did not study non-diabetics. Further study of lung function in well controlled diabetics and those with inefficient glycemic control may inform on the role of hyperglycemia accelerating inflammation and declining lung function, a hypothesis which is supported by our results.
Spirometric impairment of lung function is more common in the general US population after the age of 55 (19). In our study, diabetic patients with impaired FEV1 and FVC had a mean age of 55 years, suggesting abnormal spirometry was present in this population for some time prior to the age of 55 years. Yeh et al. demonstrated the decline in FVC is accelerated in diabetes (3) and the rate of annual decline is directly proportional to the severity of glycemia. Restriction of vital capacity is clinically significant when gaseous exchange is impaired (32) and spirometry addresses only partly the ventilatory restriction, without probing into cardiopulmonary dynamics such as alveolar gas exchange. It is therefore necessary to examine components of vital capacity and chest wall–lung mechanics in the diabetic patient without and particularly with obesity. We recommend obese diabetic patients, be evaluated annually for abnormalities of pulmonary function, with the same focused attention as for dyslipidemia, hypertension, hyperuricemia and renal function. Based on the findings we suggest that diabetic patients with restrictive pulmonary function undergo annual radiological evaluation to detect or exclude an underlying pulmonary parenchymal pathology, an assessment which is planned for our future studies. When cohorts of diabetic and non-diabetic men were examined in a longitudinal study, Litonjua et al. (33) found that those predisposed to develop diabetes had reduced lung function several years before diagnosis as compared to men who did not develop diabetes, and the decline in lung function persisted after diabetes developed. This finding taken together with those from the Atherosclerosis Risk in Communities (ARIC) Study (34) demonstrates diminished lung function is an independent predictor of incident type 2 diabetes, pointing to the lung as a target organ of diabetes-induced injury.
In the present study blinded skin vasoconstrictor testing was done in duplicate, a trained researcher did the spirometry evaluation and in the analysis we adjusted for waist circumference and BMI considering the strong relationship between type 2 diabetes and central adiposity. Limitations however are present. This was an open study in a conveniently sampled population and its sensitivity could have been enhanced by a case controlled design between sub-optimally and well controlled diabetics. Only one measurement of HbA1C was done to ascertain glycemic control restricting its usefulness in labeling disease control.
In summary lung function is impaired and associated with inflammation in obese West Indian adult diabetics with inefficient glycaemic control. Physicians should be alerted to evaluating pulmonary function in diabetic patients, and particularly monitor the obese diabetic. These findings are of significant clinical import, for the Caribbean peoples and West Indian migrations globally.
Acknowledgements
The study was supported by a research award from The Government of the Republic of Trinidad and Tobago. Data collection and spirometric evaluation was done by Nurse Desert Francis.
Disclosure: The authors declare no conflict of interest.
References
- Ford ES, Mannino DM, National Health and Nutrition Examination Survey Epidemiologic Follow-up Study. Prospective association between lung function and the incidence of diabetes: findings from the National Health and Nutrition Examination Survey Epidemiologic Follow-up Study. Diabetes Care 2004;27:2966-70. [PubMed]
- Walter RE, Beiser A, Givelber RJ, et al. Association between glycemic state and lung function: the Framingham Heart Study. Am J Respir Crit Care Med 2003;167:911-6. [PubMed]
- Yeh HC, Punjabi NM, Wang NY, et al. Cross-sectional and prospective study of lung function in adults with type 2 diabetes: the Atherosclerosis Risk in Communities (ARIC) study. Diabetes Care 2008;31:741-6. [PubMed]
- Lee HM, Chung SJ, Lopez VA, et al. Association of FVC and total mortality in US adults with metabolic syndrome and diabetes. Chest 2009;136:171-6. [PubMed]
- Lee HM, Le TV, Lopez VA, et al. Association of C-reactive protein with reduced forced vital capacity in a nonsmoking U.S. population with metabolic syndrome and diabetes. Diabetes Care 2008;31:2000-2. [PubMed]
- Lim SY, Rhee EJ, Sung KC. Metabolic syndrome, insulin resistance and systemic inflammation as risk factors for reduced lung function in Korean nonsmoking males. J Korean Med Sci 2010;25:1480-6. [PubMed]
- Dahl M, Vestbo J, Lange P, et al. C-reactive protein as a predictor of prognosis in chronic obstructive pulmonary disease. Am J Respir Crit Care Med 2007;175:250-5. [PubMed]
- Thorington P, Avila G, Haynes C, et al. FEV1 is inversely related to frequency of chest infections in chronic disease patients in Trinidad and Tobago. West Indian Med J 2007;43:0-40.
- Thorington P, Rios M, Avila G, et al. Prevalence of chronic obstructive pulmonary disease among stable chronic disease subjects in primary care in Trinidad, West Indies. J Thorac Dis 2011;3:177-82. [PubMed]
- Ferguson TS, Tulloch-Reid MK, Wilks RJ. The epidemiology of diabetes mellitus in Jamaica and the Caribbean: a historical review. West Indian Med J 2010;59:259-64. [PubMed]
- Healthy Caribbean Coalition - Background paper and fact sheet for the Healthy Caribbean -2008-first Caribbean Chronic Disease Conference-No1. Accessed 2011. Available online: www.healthycaribbean.org/hcc/fact_sheet_1.html
- Cooper RS, Rotimi CN, Kaufman JS, et al. Prevalence of NIDDM among populations of the African diaspora. Diabetes Care 1997;20:343-8. [PubMed]
- Gulliford MC, Mahabir D, Rocke B. Diabetes-related inequalities in health status and financial barriers to health care access in a population-based study. Diabet Med 2004;21:45-51. [PubMed]
- Gläser S, Ittermann T, Koch B, et al. Airflow limitation, lung volumes and systemic inflammation in a general population. Eur Respir J 2012;39:29-37. [PubMed]
- Rasmussen F, Mikkelsen D, Hancox RJ, et al. High-sensitive C-reactive protein is associated with reduced lung function in young adults. Eur Respir J 2009;33:382-8. [PubMed]
- Available online: http://www.idf.org/webdata/docs/MetS_def_update2006.pdf
- Miller MR, Crapo R, Hankinson J, et al. General considerations for lung function testing. Eur Respir J 2005;26:153-61. [PubMed]
- Burke JP, Hale DE, Hazuda HP, et al. A quantitative scale of acanthosis nigricans. Diabetes Care 1999;22:1655-9. [PubMed]
- Hankinson JL, Odencrantz JR, Fedan KB. Spirometric reference values from a sample of the general U.S. population. Am J Respir Crit Care Med 1999;159:179-87. [PubMed]
- Brown PH, Teelucksingh S, Matusiewicz SP, et al. Cutaneous vasoconstrictor response to glucocorticoids in asthma. Lancet 1991;337:576-80. [PubMed]
- Hosseinpoor AR, Parker LA, Tursan d'Espaignet E, et al. Social determinants of smoking in low- and middle-income countries: results from the World Health Survey. PLoS One 2011;6:e20331. [PubMed]
- Shah A, Mehta N, Reilly MP. Adipose inflammation, insulin resistance, and cardiovascular disease. JPEN J Parenter Enteral Nutr 2008;32:638-44. [PubMed]
- Pinto Pereira LM, Seemungal TA, Teelucksingh S, et al. Markers of lung function and inflammation in West Indian diabetics. Eur Respir J 2010;1:18-22.
- Seemungal T, Pinto Pereira LM, Teelucksingh S, et al. Inflammation in diabetes Is related directly to glycaemic control and inversely to FEV1. Am J Respir Crit Care Med 2011;183:A1326.
- Teelucksingh S, Jaimungal S, Pinto Pereira L, et al. Does insulin resistance co-exist with glucocorticoid resistance in the metabolic syndrome? Studies comparing skin sensitivity to glucocorticoids in individuals with and without acanthosis nigricans. Cardiovasc Diabetol 2012;11:31. [PubMed]
- Ruiz JR, Rizzo NS, Ortega FB, et al. Markers of insulin resistance are associated with fatness and fitness in school-aged children: the European Youth Heart Study. Diabetologia 2007;50:1401-8. [PubMed]
- Gan WQ, Man SF, Senthilselvan A, et al. Association between chronic obstructive pulmonary disease and systemic inflammation: a systematic review and a meta-analysis. Thorax 2004;59:574-80. [PubMed]
- Dennis RJ, Maldonado D, Rojas MX, et al. Inadequate glucose control in type 2 diabetes is associated with impaired lung function and systemic inflammation: a cross-sectional study. BMC Pulm Med 2010;10:38. [PubMed]
- Wannamethee SG, Shaper AG, Rumley A, et al. Lung function and risk of type 2 diabetes and fatal and nonfatal major coronary heart disease events: possible associations with inflammation. Diabetes Care 2010;33:1990-6. [PubMed]
- Chance WW, Rhee C, Yilmaz C, et al. Diminished alveolar microvascular reserves in type 2 diabetes reflect systemic microangiopathy. Diabetes Care 2008;31:1596-601. [PubMed]
- Hsia CC, Raskin P. Lung involvement in diabetes: does it matter? Diabetes Care 2008;31:828-9. [PubMed]
- Lawlor DA, Ebrahim S, Smith GD. Associations of measures of lung function with insulin resistance and Type 2 diabetes: findings from the British Women's Heart and Health Study. Diabetologia 2004;47:195-203. [PubMed]
- Litonjua AA, Lazarus R, Sparrow D. Lung function in type 2 diabetes: the Normative Aging Study. Respir Med 2005;99:1583-90. [PubMed]
- Yeh HC, Punjabi NM, Wang NY, et al. Vital capacity as a predictor of incident type 2 diabetes: the Atherosclerosis Risk in Communities study. Diabetes Care 2005;28:1472-9. [PubMed]