Preoperative risk factors for successful extubation or not after lung transplantation
Introduction
Lung transplant (LTx) is the only effective therapeutic strategy for most end-stage lung diseases, such as chronic obstructive pulmonary disease (COPD), interstitial lung disease (ILD), and cystic fibrosis (CF). Up to now, there were more than 69,200 patients who have received LTx around the world (1).
Tracheal intubation and mechanical ventilation (MV) are the critical short-term life support techniques from scheduled surgical procedures to acute respiratory failure, which is the routine practice during LTxs. Some patients even needed ventilation support before surgery to wait for a matching donor.
Nowadays, increasing studies have proved early extubation, especially extubation in the operative room, was directly associated with good long-term survival for patients undergoing LTx (2,3). However, not all patients are suitable for early extubation. About 10–20% of patients might require emergency reintubation after successfully weaning from MV caused by post-extubation acute respiratory failure, or prolonged extubation (4,5). Unsuccessful extubation is associated with prolonged MV, a higher risk of ventilator-associated pneumonia, longer intensive care unit and hospital stays, and increased mortality (25–50%) (6,7).
Reintubation has been proved to be independent prognostic factors and increased mortality (86%) in LTX (8). However, confronted by alarmingly high mortality, there is a lack of relevant studies to conduct clinicians to prevent the risk of unsuccessful extubation or reintubation. In this study, we examined the associated preoperative risk factors of unsuccessful extubation or reintubation in LTx patients. We present the following article in accordance with the STROBE reporting checklist (available at http://dx.doi.org/10.21037/jtd-20-2546).
Methods
Patients
The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by Ethics Commission of the First Affiliated Hospital of Guangzhou Medical University (No. 2019-53) and informed consent was taken from all the patients.
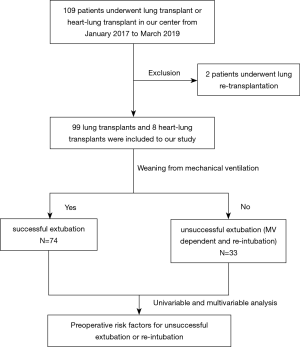
An observational retrospective case-control study was performed in all patients who underwent LTx or heart-LTxs in our center between January 2017 and March 2019, with a survival follow-up of 1 year. The first LTx was included for the next analysis, and the re-transplant was excluded in consideration of the complex preoperative status, the flow diagram as shown in Figure 1.
Postoperative MV management
The extubation criteria were: (I) successful spontaneous breathing trial (SBT) 120 minutes; (II) hemodynamic stability; (III) Glasgow coma scale score of 13 or larger; (IV) without upper airway resistance and controllable secretions; (V) ameliorative imaging of chest X-ray. As reported in the previous study in detail (9). The reintubation would be performed when the patients suffered from post-extubation respiratory failure or serve clinical events, such as respiratory or cardiac arrest, massive aspiration, serve hemodynamic instability, and so on. In our center, a tracheostomy was performed if a patient failed to wean from the ventilator and intubation would exceed postoperative 30 days, which was evaluated by intensive care physicians.
Definition of variables
The independent variables analyzed included the patient’s demographic characteristics (sex, age, and BMI), indication [idiopathic pulmonary fibrosis (IPF), COPD, silicosis, and others], general preoperative factors [extracorporeal membrane oxygenation (ECMO), independent sputum clearance, and partial pressure of oxygen/fraction of inspired oxygen (PaO2/FiO2)], and type of transplant. The ability of independent sputum clearance of patients was judged by the clinical physician based on whether the patients could clear sputum by spontaneous cough without medical assistance or not during being hospitalized for transplantation. The major dependent variable (primary outcomes) analyzed whether were successful extubation or not. The second dependent variables (secondary outcomes) was reintubation.
In this study, the age was stratified three subgroups, included age between 45 and 65 years, younger than 45 years, and older than 65 years. The BMI has also stratified three subgroups, less than 18.5 (underweight), 18.5 to 24.9 (normal), more than 24.9 (overweight). According to the preoperative arterial PaO2 and FiO2, the patients were divided into three subgroups, PaO2/FiO2 less than 150, PaO2/FiO2 between 150 to 250, and PaO2/FiO2 more than 250. And we defined successful extubation as the first successful extubation within 30 days after LTx and without reintubation. The unsuccessful extubation contained MV dependent or reintubation.
Statistical analysis
All statistical analysis was performed with SPSS 19.0. Univariable analysis was performed to assess statistically significant data by using the chi-square test. While the variables with P<0.20 were entered into the further multivariable analysis. Logistic regression models were applied for multivariable analysis using a forward stepwise selection procedure. The cutoff for variable removal was set at a significance level of 0.05. A probability value of P<0.05 was required for entry into the model and P>0.05 for elimination. Results were expressed as an odds ratio with a 95% confidence interval (CI). We used receiver operating characteristic (ROC) curves to calculate the area under the curve (AUC) values to assess the predictive ability of relevant preoperative factors for unsuccessful extubation or reintubation. In this study, a statistical significance was defined as P<0.05.
Results
Subject demographics
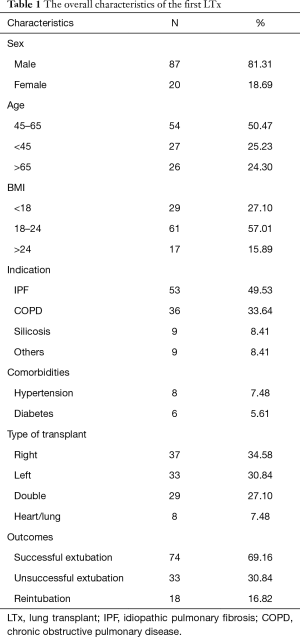
One hundred and nine LTX were performed: 2 re-transplant, 9 heart-lung, 33 left unilateral, and 37 right unilateral and 29 bilateral transplants in our center between January 2017 and March 2019. Among them, 2 patients who underwent re-transplant were excluded. A total of 107 patients undergoing first LTx were categorized into different groups according to weaning from MV or not, including successful extubation or unsuccessful extubation (including reintubation or MV dependent). As shown in Table 1, there were 74 (69.16%) patients who successfully liberated from MV, and 33 (30.84%) patients who were unsuccessful extubation, which included 18 patients (16.82%) who suffered from reintubation and 15 patients with MV dependent (14.02%), and 9 patients underwent a tracheostomy because MV exceeds 30 days. The main age of the sample was between 45 and 65 (50.47%), with 81.31% male patients. IPF occupied the main reasons from those LTx patients (49.53%), following by COPD (33.64%) and silicosis (8.41%). The postoperative severe infections were the main causes of unsuccessful extubation, occupied by 75.76%.
Full table
Relevant preoperative factors influencing unsuccessful extubation
Univariable analysis
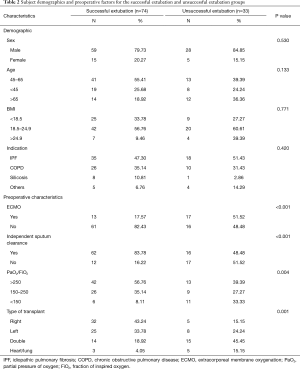
According to univariable analysis, ECMO, independent sputum clearance, hypoxia, and type of transplant were the impact factors for the prolonged extubation. There was a greater percentage of unsuccessful extubation patients who had received ECMO support bridge to LTx (51.52% vs. 17.57%, P<0.001) (Table 2). A greater proportion of patients in the successful extubation group had the preoperative ability of independent sputum clearance (83.78%) compared with the unsuccessful extubation group (48.48%) (P<0.001). The patients in unsuccessful extubation had more probably suffered PaO2/FiO2 <150 before LTx (33.33%) compared with successful extubation (8.11%) (P=0.004). A greater percentage of the unsuccessful extubation patients had undergone double-lung or heart-LTx compared with the successful group (45.45% vs. 18.92%, and 15.15% vs. 4.05%, respectively; P=0.001). The demographic characteristics, such as sex, age, BMI, and diagnosis, were not significantly associated with differential risk for unsuccessful extubation.
Full table
Multivariable analysis
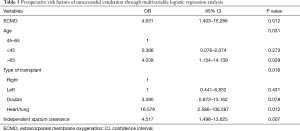
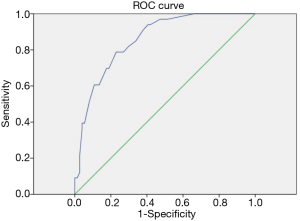
This study used multivariable logistic regression to investigate the preoperative risk factors of unsuccessful extubation for undergoing LTx patients. As shown in Table 3, associated preoperative risk factors for unsuccessful extubation following LTx included preoperative ECMO support (OR =4.631, 95% CI: 1.403–15.286, P=0.012), the preoperative ability of independent expectoration (OR =4.517, 95% CI: 1.498–13.625, P=0.007), the age older than 65-year-old (OR =4.039, 95% CI: 1.154–14.139, P=0.029), and receiving the double lung and heart-LTx (OR =3.390, 95% CI: 0.873–13.162, P=0.078; and OR =16.579, 95% CI: 2.586–106.287, P=0.012, respectively). The ROC curve was presented in Figure 2 for the preoperative predicted model of unsuccessful extubation in LTx, with C-statistic for the ROC AUC =0.857 (95% CI, 0.787–0.928).
Full table
Relevant preoperative factors influencing re-intubation
The demographic characteristics, patient-relevant preoperative factors, and surgical indications also were selected to investigate the preoperative risk of re-intubation after LTx.
Univariable analysis and multivariable analysis
The results for the univariable analysis of re-intubation are shown in Table 4. A greater proportion of patients in re-intubation group had received ECMO support and suffered double or heart-LTx compared with the successful group (50.00% vs. 17.57%, P=0.004; and double: 44.44% vs. 18.92%, heart-lung: 11.11% vs. 4.05%, P=0.044; respectively). Regarding the independent expectoration and hypoxia variables, although there was no significant difference between the successful extubation group and the re-intubation group, the rate of re-intubation for patients without independent expectoration was higher than the successful liberation from MV (33.33% vs. 16.22%), and the patient suffered severe hypoxia was more likely to confront the re-intubation risk (22.22% vs. 6.76%).

Full table
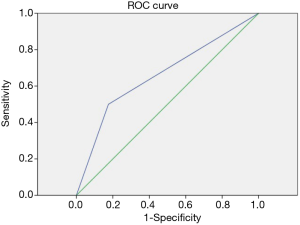
For multivariable analysis are presented in Table 5. Four relevant preoperative factors, including ECMO, independent expectoration, PaO2/FiO2, and type of transplant, were analyzed through multivariable logistic regression. Only the preoperative ECMO remained a significant predictor of re-intubation (OR =4.69, 95% CI: 1.56–15.286, P=0.012). The ROC curve was presented in Figure 3, with C-statistic for the ROC AUC =0.662 (95% CI: 0.511–0.813).

Full table
Long-term outcome
In this study, 1-year mortality for successful extubation was 12.12%. For the unsuccessful extubation or re-intubation, the 1-year mortality was 81.82% and 72.22%, respectively.
Discussion
According to the 2019 report from the International Thoracic Organ Transplant Registry, there were more than 69,200 adult and 4,128 adult heart-LTxs performed through June 30, 2018, around the world (1). Many studies have proved the early extubation was directly associated with good long-term survival for patients undergoing LTx (2,3). However, the difficulty for clinical work is to assess which patients are suitable for early extubation after undergoing LTx. Previous studies have reported nearly 20% of LTX patients might suffer the risk of reintubation after the first liberation from MV (8,10,11), In our center, the reintubation rate was 16.82% which is similar to those previous reports. In addition to the reintubation, 14.02% of patients developed MV dependent due to postoperative complications, such as primary graft dysfunction, respiratory infections, and chronic lung allograft dysfunction. In this study, we aimed at discriminating the high-risk patients of unsuccessful extubation by preoperative characteristics, and understanding the effect of preoperative factors on unsuccessful extubation presents an important opportunity for improving successful extubation.
We found preoperative ECMO support was an important factor for unsuccessful extubation (OR =4.631). Despite many reports have demonstrated the safety and success of ECMO as a bridge to transplant (12,13). However, the patients receiving preoperative ECMO support have worse perioperative outcomes than patients not requiring ECMO support for some low volume centers (14,15).
We found the ability of preoperative sputum clearance was associated with whether successful extubation or not. The patients without the independent sputum clearance ability had more risk than patients with the ability to unsuccessfully weaning from MV (OR =4.517). Patients undergoing LTx are subject to lifelong immunosuppression to manage allograft rejection (16), but meanwhile which increases the risk of graft lung infection (17). On the other hand, LTx altered recipients’ respiratory physiology such as diminish cough reflex, denervation, and impair mucociliary clearance (18,19), which caused the patients, especially the inability of independent sputum clearance, have more difficult to clear sputum. Sputum clearance is vital for the recovery after LTx through reducing infection and inflammation and improving lung function. Therefore, the independent sputum clearance impact whether weaning or not probably related to postoperative pulmonary infection. The rates of unsuccessful extubation may be decreased by strengthening the preoperative training of independent sputum clearance to waiting for LTx patients.
In our study, we found that type of transplant also could influence whether successful extubation or not. The right single LTx had the lowest risk for unsuccessful extubation, followed by left single LTx and double LTx. And the heart-LTx receptors suffered the highest fail risk for postoperative extubation (OR =16.579, vs. right single transplant). we found the right single LTx had less risk for extubation failure than the left single LTx (OR =1.735), although the difference was not significant in statistics (P=0.431). the more angle of the right main bronchus may be a potential cause leading to less extubation for right single LTx, which may decrease the postoperative infection risk of transplanted lung. Moreover, I Ben Nachum and associates reported that the left-sided bronchial anastomosis may be more vulnerable to complications (20). Therefore, we recommend patients undergoing single LTx, especially right single LTx, can consider early extubation. On the contrary, we should detailly assess before weaning from MV for double LTx or heart-LTx.
It is known that aging causes many physiological changes and syndromes that lead to increasing fragility, resulting in an increased risk of postoperative complications (21,22). Ehrsam has reported that older age serves as a marker for a complex constellation of factors that might be considered the relative or absolute contraindication to LTx (23). In this study, we found that patients older than 65 years have a higher risk of extubation failure than the age between 45- and 65-year-old (OR =4.039). The higher risk of unsuccessful extubation for the old patients may partly account for lower median survival compared with their younger counterparts.
Compared with those patients with MV dependent, there may are more chances to liberate from MV successfully for the patients suffering from reintubation. Therefore, we further investigate the preoperative predicted factors of reintubation. Although the four preoperative factors, such as ECMO, Independent sputum clearance, PaO2/FiO2, and type of transplant, were included in multivariable logistic regression analysis. Only preoperative ECMO remained a significant predictor of reintubation. The patients with pretransplant ECMO often continue to keep ECMO support in early post-transplant, which will increase the odds for some postoperative complications, such as postoperative ventilator support >48 hours, in-hospital stroke, in-hospital dialysis, in-hospital acute rejection episodes, etc. (10,24). Those complications may further cause re-intubation.
Limitations
This study has some limitations. this study is a retrospective, non-randomized, single-center study. The observational design means that there is a possibility of unmeasured factors that could be confounders of the relationships described. We have attempted to reduce those confounder factors by including as many variables as were available to us in our multivariable logistic regression. Moreover, we didn’t include the factors of the donor’s lung into this study, which need further study to investigate the predicted functions of postoperative extubation.
Conclusions
In conclusion, as we develop a more comprehensive understanding of the preoperative predicted factors behind postoperative unsuccessful extubation or reintubation, we will have more chances to prevent early and provide more precise and personalized airway management strategies for patients who have a high risk for unsuccessful extubation. In our study, we demonstrated that preoperative independent sputum clearance, preoperative ECMO, older than 65-year-old, and double lung or heart-LTx were four independent risk factors for unsuccessful extubation. Further, we found that preoperative ECMO was the only independent risk factor for reintubation. Unsuccessful extubation may be avoided by proper perioperative management for those high-risk patients, and for those low preoperative patients, we recommend to liberate from MV early.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at http://dx.doi.org/10.21037/jtd-20-2546
Data Sharing Statement: Available at http://dx.doi.org/10.21037/jtd-20-2546
Peer Review File: Available at http://dx.doi.org/10.21037/jtd-20-2546
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/jtd-20-2546). JH serves as the unpaid Executive Editor-in-Chief of Journal of Thoracic Disease. WL serves as an unpaid Editorial Board Member of Journal of Thoracic Disease from Apr 2018 to Apr 2021. The other authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by Ethics Commission of the First Affiliated Hospital of Guangzhou Medical University (No. 2019-53) and informed consent was taken from all the patients.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Chambers DC, Cherikh WS, Harhay MO, et al. The International Thoracic Organ Transplat Registry of the International Society for Heart and Lung Transplant: Thirty-sixth adult lung and heart-lung transplant Report-2019; Focus theme: Donor and recipient size match. J Heart Lung Transplant 2019;38:1042-55. [Crossref] [PubMed]
- Felten ML, Moyer JD, Dreyfus JF, et al. Immediate postoperative extubation in bilateral lung transplant: predictive factors and outcomes. Br J Anaesth 2016;116:847-54. [Crossref] [PubMed]
- Assenzo V, Assenzo C, Filippo R, et al. The feasibility of extubation in the operating room after bilateral lung transplant in adult emphysema patients: an observational retrospective study. Eur J Cardiothorac Surg 2018;54:1128-33. [Crossref] [PubMed]
- Boles JM, Bion J, Connors A, et al. Weaning from mechanical ventilation. Eur Respir J 2007;29:1033-56. [Crossref] [PubMed]
- Crotti S, Bottino N, Spinelli E. Spontaneous breathing during veno-venous extracorporeal membrane oxygenation. J Thorac Dis 2018;10:S661-9. [Crossref] [PubMed]
- Esteban A, Alía I, Gordo F, et al. Extubation outcome after spontaneous breathing trials with T-tube or pressure support ventilation. The Spanish Lung Failure Collaborative Group. Am J Respir Crit Care Med 1997;156:459-65. [Crossref] [PubMed]
- Boffini M, Simonato E, Ricci D, et al. Extracorporeal membrane oxygenation after lung transplantation: risk factors and outcomes analysis. Ann Cardiothorac Surg 2019;8:54-61. [Crossref] [PubMed]
- Machuca TN, Schio SM, Camargo SM, et al. Prognostic factors in lung transplantation: the Santa Casa de Porto Alegre experience. Transplantation 2011;91:1297-303. [Crossref] [PubMed]
- Hernández G, Vaquero C, González P, et al. Effect of postextubation high-flow nasal cannula vs conventional oxygen therapy on reintubation in low-risk patients: a randomized clinical trial. JAMA 2016;315:1354-61. [Crossref] [PubMed]
- Hayanga JWA, Hayanga HK, Fugett JH 2nd, et al. Contemporary look at extracorporeal membrane oxygenation as a bridge to reoperative lung transplantation in the United States - a retrospective study. Transpl Int 2020;33:895-901. [Crossref] [PubMed]
- Rocca GD, Coccia C, Costa GM, et al. Is very early extubation after lung transplant feasible? J Cardiothorac Vasc Anesth 2003;17:29-35. [Crossref] [PubMed]
- Hayanga AJ, Aboagye J, Esper S, et al. Extracorporeal membrane oxygenation as a bridge to lung transplant in the United States: an evolving strategy in the management of rapidly advancing pulmonary disease. J Thorac Cardiovasc Surg 2015;149:291-6. [Crossref] [PubMed]
- Hämmäinen P, Schersten H, Lemström K, et al. Usefulness of extracorporeal membrane oxygenation as a bridge to lung transplant: a descriptive study. J Heart Lung Transplant 2011;30:103-7. [Crossref] [PubMed]
- Halpern AL, Kohtz PD, Helmkamp L, et al. Improved mortality associated with the use of extracorporeal membrane oxygenation. Ann Thorac Surg 2019;108:350-7. [Crossref] [PubMed]
- Hayanga JW, Lira A, Aboagye JK, et al. Extracorporeal membrane oxygenation as a bridge to lung transplant: what lessons might we learn from volume and expertise? Interact Cardiovasc Thorac Surg 2016;22:406-10. [Crossref] [PubMed]
- Snell GI, Westall GP. Immunosuppression for lung transplant: evidence to date. Drugs 2007;67:1531-9. [Crossref] [PubMed]
- Munro PE, Button BM, Bailey M, et al. Should lung transplant recipients routinely perform airway clearance techniques? A randomized trial. Respirology 2008;13:1053-60. [PubMed]
- Veale D, Glasper PN, Gascoigne A, et al. Ciliary beat frequency in transplanted lungs. Thorax 1993;48:629-31. [Crossref] [PubMed]
- Duarte AG, Myers AC. Cough reflex in lung transplant recipients. Lung 2012;190:23-7. [Crossref] [PubMed]
- Ben Nachum I, Moreh O, Raviv Y, et al. Does side matter? Effect of single lung transplant laterality on outcomes. Thorac Cardiovasc Surg 2011;59:115-8. [Crossref] [PubMed]
- Hall MJ, DeFrances CJ, Williams SN, et al. National Hospital Discharge Survey: 2007 summary. Natl Health Stat Report 2010;29:1-20, 24. [PubMed]
- Turrentine FE, Wang H, Simpson VB, et al. Surgical risk factors, morbidity and mortality in elderly patients. J Am Coll Surg 2006;203:865-77. [Crossref] [PubMed]
- Ehrsam JP, Benden C, Seifert B, et al. Lung transplant in the elderly: Influence of age, comorbidities, underlying disease, and extended criteria donor lungs. J Thorac Cardiovasc Surg 2017;154:2135-41. [Crossref] [PubMed]
- Hayanga JWA, Hayanga HK, Holmes SD, et al. Mechanical ventilation and extracorporeal membrane oxygenation as a bridge to lung transplantation: Closing the gap. J Heart Lung Transplant 2019;38:1104-11. [Crossref] [PubMed]