Effect of genotype-guided strategy in East Asian vs. Caucasian patients after percutaneous coronary intervention: insight from the TAILOR-PCI trial
In patients undergoing percutaneous coronary intervention (PCI), dual antiplatelet therapy (DAPT) with aspirin and P2Y12 receptor inhibitor is the standard treatment to prevent occurrence of atherothrombotic event. Clinical application of different P2Y12 receptor inhibitors (clopidogrel, prasugrel or ticagrelor) with varying levels of antiplatelet potency has enabled physicians to consider individualized treatment strategies, which may include escalation or de-escalation of P2Y12 receptor inhibitor (1). A tailored DAPT approach may be possibly guided by platelet function testing (PFT) or genetic testing (2). The data of the TAILOR-PCI (Tailored Antiplatelet Therapy Following PCI) trial evaluated clinical efficacy and safety of genotype-guided strategy (potent P2Y12 receptor inhibitor in cases with CYP2C19 loss-of-function allele) vs. conventional treatment with clopidogrel (3), which could be another important evidence showing inter-racial differences of clinical benefit according to the selected treatment method (including 38.3% of East Asians and 49.1% of the Whites). During antithrombotic treatment, East Asians vs. Caucasian patients have shown a reduced benefit for ischemic events, an increased hazard for bleeding events, and race-specific response for the antithrombotic drugs, which has been a well-described and clinically important phenomenon termed the “East Asian Paradox” (4-7).
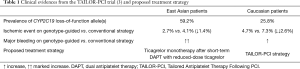
To mention at the first place, there are different frequencies of gene polymorphisms contributing to effects of antithrombotic agents across races (8) (Table 1). In the TAILOR-PCI trial, East Asian cohort showed a higher frequency of the CYP2C19 loss-of-function allele carriage compared with the Caucasian cohort (59.2% vs. 25.8%, P<0.001) (3), which may indicate decreased effect of clopidogrel in East Asian population. Second, there have been different risks of ischemic event and unique clinical benefit achieved by an antiplatelet treatment according to race (9,10). In the TAILOR-PCI trial, despite the same treatment with clopidogrel in patients carrying the CYP2C19 loss-of-function allele, Caucasian patients showed increased risk of ischemic event by about 1.8-fold than Asian patients (7.3% vs. 4.1%) (3). In addition, the genotype-guided strategy vs. conventional treatment reduced the risk of 1-year ischemic event after index PCI by 1.4% (2.7% vs. 4.1%) and 2.6% (4.7% vs. 7.3%) in the Asians and Caucasians, respectively (3). Finally, response to antithrombotic agents and prevalence of adverse side effects related with these agents can be different between races (1-4,11-13). The exposures of ticagrelor and its major active metabolite (AR-C124910XX) are approximately 40% higher in East Asian individuals than in White individuals (4-7), which correlates with the level of platelet inhibition. During standard-dose ticagrelor treatment, East Asian patients have shown increased risks of clinically serious bleeding (about 2-fold risk of clinically serious bleeding vs. clopidogrel) (11,12) and discontinuation (e.g., 1-year discontinuation rate of ticagrelor and clopidogrel: 51.5% and 9.0% in the Korean National Health Insurance Service data) (13). In the TAILOR-PCI trial (3), 1-year discontinuation rate was higher during ticagrelor vs. clopidogrel treatment (32% vs. 11%, P<0.001), which might affect clinical efficacy and safety of the genotype-guided therapy.
Taken together, the relatively high participation rate of East Asian patients in the TAILOR-PCI trial may influence the results of the study, and the delicate comparative analysis may give a deep insight into inter-racial difference in clinical benefit of the genotype-guided strategy. Furthermore, further large-scale clinical trials examining race-based clinical outcomes for a specific antithrombotic strategy are warranted for reliably assessing clinical implications and possible advantages of a tailored treatment based on patient’s race. Recent evidences suggest that ticagrelor monotherapy after short-term DAPT [from TICO (Ticagrelor Monotherapy After 3 Months in the Patients Treated With New Generation Sirolimus Stent for Acute Coronary Syndrome) trial] (14) or a reduced-dose ticagrelor treatment (from expert consensus) (7,15) would be a better choice in East Asian population with acute coronary syndrome (Table 1).
Acknowledgments
Funding: This study was supported by research grants from the Basic Science Research Program through the National Research Foundation (NRF) of Korea funded by the Ministry of Science, ICT and Future Planning (NRF-2015R1A5A2008833).
Footnote
Provenance and Peer Review: This article was a free submission to the journal. The article did not undergo external peer review.
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/jtd-20-3066). Dr. YHJ reports personal fees from AstraZeneca, personal fees from Sanofi-Aventis, personal fees from Daiichi Sankyo, grants and personal fees from Han-mi Pharmaceuticals, grants and personal fees from Yuhan Pharmaceuticals, grants from U&I Corporation, non-financial support from Haemonetics, during the conduct of the study. The other authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Angiolillo DJ, Rollini F, Storey RF, et al. International Expert Consensus on Switching Platelet P2Y12 Receptor-Inhibiting Therapies. Circulation 2017;136:1955-75. [PubMed]
- Sibbing D, Aradi D, Alexopoulos D, et al. Updated Expert Consensus Statement on Platelet Function and Genetic Testing for Guiding P2Y12 Receptor Inhibitor Treatment in Percutaneous Coronary Intervention. JACC Cardiovasc Interv 2019;12:1521-37. [PubMed]
- Pereira NL, Farkouh ME, So D, et al. Effect of Genotype-Guided Oral P2Y12 Inhibitor Selection vs Conventional Clopidogrel Therapy on Ischemic Outcomes After Percutaneous Coronary Intervention: The TAILOR-PCI Randomized Clinical Trial. JAMA 2020;324:761-71. [PubMed]
- Kim HK, Tantry US, Smith SC Jr, et al. The East Asian Paradox: An Updated Position Statement on the Challenges to the Current Antithrombotic Strategy in Patients with Cardiovascular Disease. Thromb Haemost 2020. Epub ahead of print. [Crossref] [PubMed]
- Levine GN, Jeong YH, Goto S, et al. Expert consensus document: World Heart Federation expert consensus statement on antiplatelet therapy in East Asian patients with ACS or undergoing PCI. Nat Rev Cardiol 2014;11:597-606. [PubMed]
- Bae JS, Ahn JH, Tantry US, et al. Should Antithrombotic Treatment Strategies in East Asians Differ from Caucasians? Curr Vasc Pharmacol 2018;16:459-76. [PubMed]
- Huo Y, Jeong YH, Gong Y, et al. 2018 update of expert consensus statement on antiplatelet therapy in East Asian patients with ACS or undergoing PCI. Science Bulletin 2019;64:166-79.
- Scott SA, Sangkuhl K, Stein CM, et al. Clinical pharmacogenetics implementation consortium guidelines for CYP2C19 genotype and clopidogrel therapy: 2013 update. Clin Pharmacol Ther 2013;94:317-23. [PubMed]
- Kang J, Park KW, Palmerini T, et al. Racial Differences in Ischaemia/Bleeding Risk Trade-Off during Anti-Platelet Therapy: Individual Patient Level Landmark Meta-Analysis from Seven RCTs. Thromb Haemost 2019;119:149-62. [PubMed]
- Golomb M, Redfors B, Crowley A, et al. Prognostic Impact of Race in Patients Undergoing PCI: Analysis From 10 Randomized Coronary Stent Trials. JACC Cardiovasc Interv 2020;13:1586-95. [PubMed]
- Kang J, Han JK, Ahn Y, et al. Third-Generation P2Y12 Inhibitors in East Asian Acute Myocardial Infarction Patients: A Nationwide Prospective Multicentre Study. Thromb Haemost 2018;118:591-600. [PubMed]
- Park DW, Kwon O, Jang JS, et al. Clinically Significant Bleeding With Ticagrelor Versus Clopidogrel in Korean Patients With Acute Coronary Syndromes Intended for Invasive Management: A Randomized Clinical Trial. Circulation 2019;140:1865-77. [PubMed]
- Yun JE, Kim YJ, Park JJ, et al. Safety and Effectiveness of Contemporary P2Y12 Inhibitors in an East Asian Population With Acute Coronary Syndrome: A Nationwide Population-Based Cohort Study. J Am Heart Assoc 2019;8:e012078. [PubMed]
- Kim BK, Hong SJ, Cho YH, et al. Effect of Ticagrelor Monotherapy vs Ticagrelor With Aspirin on Major Bleeding and Cardiovascular Events in Patients With Acute Coronary Syndrome: The TICO Randomized Clinical Trial. JAMA 2020;323:2407-16. [PubMed]
- Kim HK, Ahn Y, Chang K, et al. 2020 Korean Society of Myocardial Infarction Expert Consensus Document on Pharmacotherapy for Acute Myocardial Infarction. Korean Circ J 2020;50:845-66. [PubMed]