A video demonstration of the Li’s anastomosis—the key part of the “non-tube no fasting” fast track program for resectable esophageal carcinoma
Introduction
The fast track (FT) surgical patient pathway, which aims to improve the perioperative treatment of surgery for cancer patients, has been well studied in colorectal (1), gynecological (2), and gastric cancer (3) patients and has significantly reduced the surgical stress and costs (4,5). However, this program for esophagectomy patients is rarely used. The main concern of allowing early oral feeding postoperatively in patients with esophagectomy is the possible increase in the incidence of anastomotic leakage. Based on retrospective studies and surgical technical experience, Dr. Yin Li used the Li’s anastomosis to ensure first-day oral feeding at will after an esophagectomy (6), which made the early oral feeding fast track surgical program possible for esophageal cancer patients. More than two years have been passed since the Li’s anastomosis together with “non-tube no fasting” fast track program. Until May 2015, about 260 cases have started oral nutrition on postoperative day (POD) 1 at will without a nutrition tube and fasting, which represents the so-called “non-tube no fasting” fast track program.
Indications
This procedure is indicated in all operable esophageal carcinoma patients. We recommend to adopt the fast track surrey program “non-tube no fasting” followed by the Li’s anastomosis.
Results
This procedure together with “non-tube no fasting” fast track program has been successfully conducted for more than 2 years by our group. We started a randomized control trial in February 2014, “early oral feeding following thoracolaparoscopic oesophagectomy in patients with esophageal cancer”. In interim analyses, between February 2014 and September 2014, 148 continuous patients with thoracolaparoscopic esophagectomy were recruited. Seventy two patients were randomized in “non-tube no fasting” group and 76 patients in late oral feeding group. The anastomotic leakage rate was 2.8% for the “non-tube no feasting” group (6), which is significantly lower than that observed for mechanically stapled anastomosis and fasting for 7 days during the same period in other medical groups (n=92), (2.8% versus 10.9%, P=0.048). The post-operation hospital stay (7.6±2.2 versus 12.1±3.7, P<0.01) is quite short. In our cohort study, from June 2013 to August 2013 (n=30 in each group), the Health-related quality of life (HRQL) mean scores obtained 3 months post operation were significantly better, including those for reflux (14.07±14.86 versus 22.96±17.73, P=0.048) and dysphagia (15.56±15.33 versus 23.70±16.95, P=0.047) compared with the scores for conventional two-layer anastomosis and late oral feeding in other medical group. Additionally, the stricture rate is lower than that observed for conventional two-layer anastomosis at 6 months post operation (15.1±3.7 versus 13.2±3.4 mm, P=0.047). The simply summary of data for studies of Li’s anastomosis were shown in Table 1.
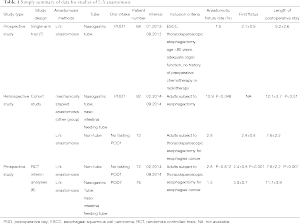
Full table
Conclusions
This safe and efficient anastomosis method significantly reduced the anastomotic leak, the number of post-operative days, reflux, dysphagia and stricture. Importantly, this method ensured at will oral feeding on first day after an esophagectomy. The “non-tube no fasting” fast track program for esophagectomy patients was thus conducted smoothly. A prospective randomized clinical trial (Clinical Trial Registration Number: NCT01998230) is ongoing in our cancer center, with a much larger sample size, to verify our findings and assess the additional potential benefits of early oral feeding after the Li’s anastomosis thoracolaparoscopic esophagectomy for esophageal cancer.
Procedure
The operation is performed under general anesthesia. The thoracolaparoscopic esophagectomy and a two-field lymph node dissection were adopted, with a left lateral decubitus position with 30° forerake. The thoracic esophagus was isolated, and the lymph nodes were harvested. Subsequently, the patient adopted a supine position. A 2-3 cm left cervical incision was made. The cervical esophagus was exposed and transected. Then, in the abdominal section, a 4-cm-wide gastric conduit was made by a linear cutting stapler (TLC, Ethicon, USA). The gastric conduit was pulled up to the neck. Finally, the Li’s anastomosis was conducted to sew the gastric conduit and the distal esophagus (Figure 1).
The Li’s anastomosis procedures included the following (Figure 2):
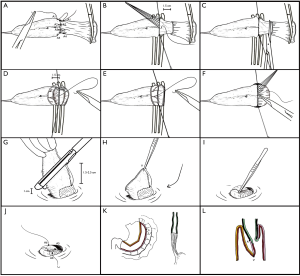
- We made a 2-3 cm skin incision on the left cervical. The muscle sparing method was utilized in the open tissue space. The distal esophagus and gastric conduit were explored.
- The lesser curvature of the gastric conduit was faced forward, and the greater curvature was faced backward. The posterior esophageal wall and posterior wall of the stomach were put together. A row of 4-0 Vicryl (Ethicon) interrupted horizontal mattress sutures were used to sew the two walls. The muscularis layer of the esophagus and the seromuscular layer of the stomach were sewn by four interrupted sutures, including two sutures at each peak and using mosquito forceps as hang lines to define the corners of the layers and obtain an optimal view (sutures were placed at the A1, A2, A3 and A4 positions). These spots were near to the greater curvature of stomach in order to get enough blood perfusion and named as anastomosis inicial spots, short for A, A1-A6. Shown in Figure 2A.
- A three-leaf clamp was used to fix the gastric conduit and esophageal stump to facilitate the suture procedure. Then, the muscularis layer of the esophagus was cut at the anastomotic side, and the seromuscular layer of the stomach was opened at the anastomotic side. The two layers were sewn with seven to eight stitches of interrupted 4-0 silk suture. Shown in Figure 2B.
- The other side of the muscularis layer of the esophagus was opened, the muscular and mucous layers of the esophagus were dissociated by approximately 1.5 cm and the redundant esophagus was removed. Shown in Figure 2C.
- The gastric mucosa layer was opened, and continuous sutures were used to carry out the mucosa anastomosis for the mucosal layers of esophagus and stomach using 4-0 Vicryl (Ethicon). Shown in Figure 2D,E.
- The three-leaf clamp was released, and the anterior muscular layer of the esophagus and the seromuscular layer of the stomach were sewn using 4-0 silk sutures. Shown in Figure 2F.
- A linear stapler was used to cut the redundant gastric conduit 1.5-2.5 cm above the anastomosis, shown in Figure 2G. Continuous 4-0 Vicryl (Ethicon) sutures were used to enhance the cutting edge. Then, the redundant gastric conduit was embedded into the gastric conduit cavity using forceps and fingers, shown in Figure 2H,I. This gastric folding was designed as a valve for anti-acid reflux. The valve was labeled in the Figure 2H,I as “V”. Finally, the gastric seromuscular layer and the anterior aspect of the esophageal muscle were sewn by intermittent 4-0 Vicryl (Ethicon) sutures together with fundoplication, shown in Figure 2J.
- The mediastinal drainage tube was placed near the anastomosis. The incision was closed with an absorbable suture.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Luglio G, De Palma GD, Tarquini R, et al. Laparoscopic colorectal surgery in learning curve: Role of implementation of a standardized technique and recovery protocol. A cohort study. Ann Med Surg (Lond) 2015;4:89-94. [PubMed]
- Philp S, Carter J, Barnett C, et al. Patients' perspectives of fast-track surgery and the role of the fast-track clinical nurse consultant in gynecological oncology. Holist Nurs Pract 2015;29:158-66. [PubMed]
- Jo DH, Jeong O, Sun JW, et al. Feasibility study of early oral intake after gastrectomy for gastric carcinoma. J Gastric Cancer 2011;11:101-8. [PubMed]
- Faucheron JL. Laparoscopy in combination with fast-track management is probably the best perioperative strategy in patients undergoing colonic resection for cancer. Ann Surg 2013;257:e5. [PubMed]
- Veenhof AA, Vlug MS, van der Pas MH, et al. Surgical stress response and postoperative immune function after laparoscopy or open surgery with fast track or standard perioperative care: a randomized trial. Ann Surg 2012;255:216-21. [PubMed]
- Li Y, Sun HB, Liu XB, et al. Poster 25: Early initiation of oral feeding following thoracolaparoscopic esophagectomy for cancer: interim results from a randomized controlled trial, 95th Annual Meeting of the American Association for Thoracic Surgery, April 25-29, 2015.
- Sun HB, Liu XB, Zhang RX, et al. Early oral feeding following thoracolaparoscopic oesophagectomy for oesophageal cancer. Eur J Cardiothorac Surg 2015;47:227-33. [PubMed]
- Zheng Y, Li Y, Wang Z, et al. A video demonstration of the Li’s anastomosis—the key part of the “non-tube no fasting” fast track program for resectable esophageal carcinoma. Asvide 2015;2:067. Available online: http://www.asvide.com/articles/611


