
Factors associated with discrepancy between fresh frozen and permanent biopsy from medical thoracoscopy: single center analysis of 172 medical flexible thoracoscopy cases
Introduction
Cases of malignancy are often accompanied by pleural effusion, and the use of medical thoracoscopy (MT) by respiratory physicians has been increasingly allowing more accurate evaluation (1-3). This diagnostic modality has the strength of acquiring pathological samples from the pleural cavity under direct visualization by the operator (2-6). Pathological confirmation of pleural malignancy to identify cases that require and are appropriate for pleural intervention is an important focus of MT (7,8). Until now, no consensus has been made on the pathological confirmation of pleural malignancy during MT (2,7-9). Frozen sectioning is often used by thoracic surgeons to more rapidly confirm a pleural malignancy during the procedure, but few medical thoracoscopists utilize this approach. The sensitivity of malignancy by frozen sectioning in patients with a pleural disease has been evaluated in two studies (10,11). Fielding et al. found that frozen sectioning performed during MT assisted in decision-making before pleurodesis (11), and Karpathiou et al. reported that frozen sectioning has a highly precise diagnostic ability in pleural pathology (10). Despite the usefulness of frozen sections, some cases have involved contradictory results between fresh frozen sections and the final pathological findings. The previous studies have commented that the limitation in sampling of pathologic samples may have been associated with pathological disagreement between frozen sections and final pathological diagnosis using MT. However, we believe that more detailed analysis accounting other important parameters is necessary.
MT has traditionally been performed using a conventional rigid thoracoscope, but more recently flex-rigid MT has been used as a diagnostic modality, with increased ease of use (12). The ability of flex-rigid MT to aid in the diagnosis of pleural disease has been compared with rigid-thoracoscopy (12). In the study by Rahman et al., the diagnostic yield of rigid thoracoscopy is 92.7% (2). In comparison with flex-rigid thoracoscopy, the diagnostic yield for rigid thoracoscopy was noted to be superior in the study by Yap et al. (12). However, more clinical data are necessary (3). More specifically, no data have been reported on the usefulness of frozen sectioning performed during flex-rigid MT.
The present study evaluated the sensitivity of the diagnosis using frozen sectioning during flex-rigid MT, and further evaluated the clinical parameters associated with discrepancy between frozen sections and permanent paraffin sections. We present the following article in accordance with the STARD reporting checklist (available at http://dx.doi.org/10.21037/jtd-20-1809).
Methods
Patient selection
In this retrospective study, we screened 212 patients who underwent MT between February 2017 and November 2019 at Incheon Saint Mary’s Hospital, the Catholic University of Korea. All cases were performed with flex-rigid MT, and we included 172 patients who underwent frozen biopsy (Figure 1). We excluded 40 patients who did not undergo frozen biopsy, as they were already diagnosed with malignant pleural effusion before the procedure.
Procedure
Flex-rigid MT (LTF-240; Olympus, Tokyo, Japan) was performed under conscious sedation using midazolam and fentanyl. The detailed information of forcep used during MT is as follows: FB-221D; Olympus, Tokyo, Japan, size 1.9 mm. The day before MT, a pleural catheter was inserted to determine whether the lung would expand after pleural effusion was sufficiently drained. Four respiratory physicians performed MT following the assigned procedure schedules. After a preliminary inspection of the pleura, biopsies were performed from the sites of interest under direct visualization by the operators using flexible biopsy forceps. The samples were sent for frozen sectioning (at least 5 samples were collected). While waiting for the results, more specimens were acquired from multiple sites. After reviewing the frozen sections, the pathologist confirmed whether the lesion was malignant or benign. If the frozen section was proven to be malignant, pleurodesis was performed by insufflating talc before placing a chest tube in the pleural cavity. When the frozen section result was inconclusive and required permanent sections for a definitive diagnosis or did not favor malignancy, we categorized these cases as favoring benign disease and did not perform talc pleurodesis. Chest X-rays were taken immediately after the procedure and the following morning to decide whether to remove the chest tube.
Pathological confirmation
Frozen sectioning
Each sample was embedded in a Cryometrix and frozen at −25 °C using the Leica-CM 1950 (Leica Biosystems, Heidelberg, Germany) cryostat. Samples were cut into 5-µm-thick sections, treated with 95% alcohol, and stained with hematoxylin and eosin. A pathologist read the frozen sections, and in a few cases, a second opinion was queried before notifying the operators of the result. After the frozen section diagnosis (FSD), the specimens were immersed in 10% neutral formalin to prepare the permanent paraffin section. All paraffin-embedded permanent sections were examined to evaluate the accuracy of the FSD.
Paraffin sectioning
Additional tissues were analyzed by routine hematoxylin and eosin staining. A pathologist read the paraffin section, and in a few cases, a second opinion was queried to a peer pathologist before submitting the final pathological report. The original frozen sections were analyzed and compared to conventional formalin-fixed paraffin-embedded tissue sections. If frozen sections and paraffin tissue sections disagreed, a pulmonologist and a pathologist (ES.P.) reviewed the sections.
Clinical data
Patients’ data including age, sex, underlying disease, and radiologic findings were acquired from the electronic medical records.
Definitions of the thoracoscopic findings
Evaluation of the clinical characteristics and thoracoscopic results yielded the following findings with regard to the pleural cavity. A pleural nodule was defined as a small round or irregularly shaped pleural lesion <3 cm in the longest diameter. If the longest diameter was >3 cm, the lesion was categorized as a pleural mass. Pleural thickening refers to a smooth, uninterrupted diffusely thickened fibrotic pleura, which prevents visualization of the pleural fat and muscle below. Fibrotic pleura tissue was difficult to tear apart from other tissue layers. Plaque-like lesions were localized, flat, and well-circumscribed areas of thin pleural thickening. A diffuse infiltration was defined as a diffuse and active permeation of the pleura by a tumor or inflammation without forming a nodule or mass.
An adhesion was defined as an abnormal union between visceral and parietal pleura with newly developed fibrous tissue. Adhesion grades were determined according to the following categories: Grade 0) no adhesions, the whole pleural cavity can be visually confirmed; Grade 1) approximately 80% of the pleural cavity can be visualized after adhesiolysis; Grade 2), 50% of the pleural space can be visualized after adhesiolysis; and Grade 3), <50% of the pleural space can be thoracoscopically observed even after attempting adhesiolysis.
Statistical analysis
All statistical analyses were performed using the SPSS software (ver. 20.0; SPSS Inc., Chicago, IL, USA). Continuous data are presented as means with ranges. The chi-square test was used to analyze the categorical parameters. Continuous variables were analyzed using Student’s t-test or the Mann-Whitney test, depending on the normality of the data distribution. A logistic regression analysis was used to evaluate the association with a false-negative FSD (later confirmed as malignant from paraffin sections). Age, sex, and factors significant in the univariate analysis were entered into multivariate analysis. A P value <0.05 was considered significant.
Ethics statement
The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). Because this was a retrospective study, no consent was needed from the patients. The Institutional Review Board of the Catholic University of Korea approved the study protocol in December 2019 (OC19RISI0180).
Results
Patient clinical characteristics
In total, 172 patients were evaluated in this study. Table 1 lists their clinical characteristics. The mean age was 69.1 years, and 108 (62.8%) patients were male; 94 (54.7%) patients were smokers, 32 (18.6%) had a history of previous malignancy, and 16 (9.3%) had a history of prior pulmonary tuberculosis. In terms of pre-procedural diagnosis, lung cancer comprised 38.4% of all cases, but the proportion of lung cancer increased to 45.9% after pathological confirmation. In addition, 80 (46.5%) patients underwent the talc pleurodesis during thoracoscopy.
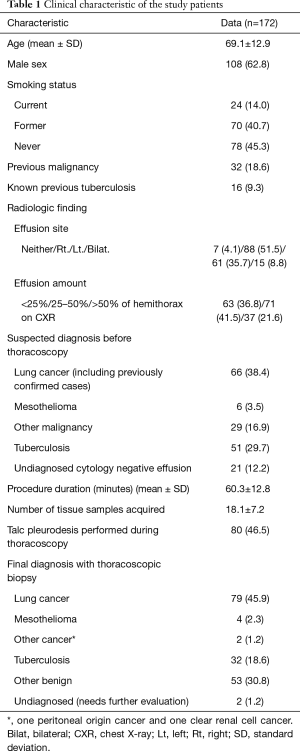
Full table
The mean duration of the procedure was 60.3 min, and the mean number of tissue samples acquired during a single MT was 18.1.
Patients with a final diagnosis of malignancy
Table 2 lists the clinical characteristics along with the initial radiological findings and thoracoscopic findings of 85 patients with a final diagnosis of malignancy. Patients were categorized into two groups depending on whether the frozen section had malignant tissues. Among the 85 patients, 75 were malignant on frozen sections, while 10 patients showed otherwise. No significant differences were observed between the two groups in terms of age, sex, history of malignancy or tuberculosis, or initial radiological findings. The group with non-malignant frozen sections had a significantly higher mean number of tissues sampled (P<0.001), and tended to have a longer procedural time (P=0.050). Regarding the proportion of patients who underwent talc pleurodesis during the procedure, it was significantly higher in the frozen malignant group compared to the frozen section negative group (93.3% vs. 30.0%, P<0.001).
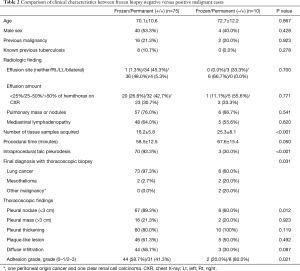
Full table
The frozen section negative group included six cases of lung cancer, two of mesothelioma, and two non-lung originating malignancy cases. The proportion of lung cancer was significantly lower in the frozen section negative group than in the frozen section malignant group (60.0% vs. 97.3%, P=0.031).
Clinically significant thoracoscopic findings were compared between the groups. The frozen section negative group had a significantly lower proportion of pleural nodules (<3 cm) and a higher proportion of high-grade adhesions (grade 2–3) compared to the frozen section malignant cases (60.0% vs. 89.3%, P=0.012 and 80.0% vs. 41.3%, P=0.021, respectively). Other findings, such as pleural mass, pleural thickening, plaque-like lesions, and diffuse infiltration, did not differ significantly between the groups.
Sensitivity of the frozen sections
When compared to permanent paraffin sections, an accurate diagnosis by a fresh frozen section was feasible in 94.2% of cases. The sensitivity of the method was 88.2%, and specificity was 100.0%. The positive predictive value was 100.0%, and the negative predictive value was 89.7%.
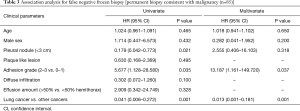
Association with a non-malignant result from frozen sections in patients with a final diagnosis of malignancy
The clinical parameters were evaluated in the 85 patients with a final diagnosis of malignancy to investigate the association with non-malignant frozen section results (Table 3). Age, sex, volume of effusion, thoracoscopic findings such as pleural nodules, plaque-like lesions, adhesion grade, and diffuse infiltration of pleura, as well as the final pathological diagnosis (lung vs. non-lung origin) were included in the univariate analysis. Absence of pleural nodules, adhesion grade, and final pathology were all significant in the univariate analysis and entered in the multivariate analysis along with age and sex. Multivariate analysis revealed that high adhesion grade, and malignancy other than lung cancer, were significant factors associated with frozen section negative cases [hazard ratio (HR) 13.187, 95% CI, 1.161–149.720, P=0.037; HR 0.013, 95% CI 0.001–0.181, P=0.001, respectively].
Full table
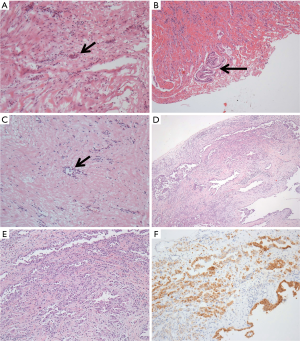
Cases of non-malignant fresh frozen biopsy results
Table 4 and Figure 1 present the non-malignant fresh frozen biopsy results later confirmed as pleural malignancy by the paraffin sections. The disagreement between frozen section and final paraffin section diagnoses was due to a sampling error in eight cases and an interpretation error in three cases. One case involved both a sampling and an interpretation error. Most of the sampling errors were due to severe fibrosis and low cellularity in the tissue samples. Three cases involving an interpretation error yielded the following findings from the frozen section diagnosis: one case with severe fibrosis, one case with both severe fibrosis and atypical mesothelial cells, and one case with findings suggestive of small cell lung cancer. The frozen sections of the malignant mesothelioma cases revealed only mesothelial hyperplasia, which was insufficient for a diagnosis of malignancy. However, the final paraffin sections revealed proliferating mesothelial cells invading surrounding tissues, which were confirmed as malignant mesothelioma after calretinin staining.

Full table
Discussion
The present study evaluated the sensitivity of frozen sectioning performed during flex-rigid MT, and further assessed the clinical factors associated with discrepancy between frozen and permanent paraffin sections. The findings provide useful information for MT operators with regard to acquiring a better pathological sample and performing later pleurodesis.
Medical thoracoscopists generally rely on macroscopic appearance for pathological diagnosis; few use frozen sectioning for this purpose (9). However, fresh frozen sections can assist with the final pathological diagnosis by enabling confirmation of malignancy and the decision to undergo further intervention via thoracoscopy during the procedure. This may shorten the time necessary for the pathological confirmation and reduce the necessity for a second pleural intervention, while also reducing the length of hospital stay.
Some previous studies have evaluated the usefulness of taking a fresh frozen section during thoracoscopy (10,11). Fielding et al. found that taking frozen sections during MT contributes to easier decision-making before pleurodesis (11), but their study population was relatively small. Karpathiou et al. also reported that frozen sections are a highly precise diagnostic modality in pleural pathology, based on an analysis of 156 frozen sections evaluated during MT and video-assisted thoracoscopic surgery (10). Our study included 172 MT cases that used only a flex-rigid thoracoscope and flexible forceps, so it has strengths in terms of both the number and homogeneous features of the study population. Furthermore, we have shown that among the malignant cases, frozen section results assisted the decision to perform talc pleurodesis during thoracoscopy, with significantly higher proportion of performance in the frozen malignant cases than in the frozen negative cases (93.3% vs. 30.0%).
Our results yielded some novel findings regarding flex-rigid thoracoscopes and fresh frozen sectioning during MT. First, we found that the flex-rigid thoracoscope is a reliable tool for diagnosing pleural disease. Yap et al. reported that the flex-rigid thoracoscope may have limitations in terms of acquiring a large amount of tissue from fibrotic pleura despite diagnostic yields comparable to rigid thoracoscopy (12). In the present study, many of the included cases were accompanied by significant fibrotic lesions, such as pleural thickening and adhesions in the pleural cavity, but only two cases required surgical exploration for further pathological confirmation. If the pre-procedural findings suggested a high possibility of malignancy and the frozen section results were non-malignant, we tried to acquire as many tissue samples as possible from multiple sites at various tissues levels for the paraffin histological diagnosis. Therefore, the limitation of the flex-rigid thoracoscope due to fibrotic pleura can be overcome by acquiring many tissue samples from multiple sites in the pleural cavity.
Second, we identified which clinical parameters were associated with the pathological discrepancy. The 10 cases diagnosed as non-malignant from frozen sections but later confirmed to be malignant were more likely to be accompanied by complex adhesions in the pleural cavity and were less likely to be lung cancer. Moderate-to-severe adhesions may have limited the visual field in the pleural cavity, thus making it more difficult to discover pleural nodules or pleural thickening, which would have suggested a pleural malignancy (10).
It is unknown why malignancy other than lung cancer was more likely to be frozen section negative. Of the 10 cases, two were mesothelioma. The diagnosis of mesothelioma often requires a large number of pathological samples involving different layers of pleural tissue, because microscopic confirmation of tumor cells invading fat tissue, muscle tissue, or lung parenchyma is necessary (13,14). This discrepancy was also observed in the study conducted by Fielding et al. in which incorrect identification as benign in the malignant group was due to sampling from superficial benign tissues overlying malignant deposits (11). We believe that deeper frozen section biopsies should be performed when mesothelioma is suspected. In addition, the calretinin stain not performed in the frozen section could have contributed to the discrepancy in diagnosis of malignant mesothelioma. The immune staining helped diagnose malignant mesothelioma in the permanent paraffin section, which supports its necessity in a more accurate pathologic diagnosis.
The other two cases were metastatic lesions from primary peritoneal cancer and clear cell renal cell carcinoma. These two diseases were difficult to diagnose using only frozen sections; pathological assessment using a small number of samples is difficult, so surgical biopsy is usually preferred (15,16). If the pre-thoracoscopy diagnosis is likely to be a malignancy other than lung cancer, more emphasis should be put on the permanent final paraffin histological diagnosis using a large number of tissue samples.
This study had some limitations. First, it had a retrospective design. However, the study patients underwent MT following the same preplanned protocol, and the cases were consecutively enrolled for evaluation. Second, this was a single-center study and the demographic features of our study patients may differ from other centers.
In conclusion, fresh frozen sectioning during MT using flex-rigid bronchoscopy was a useful diagnostic modality with reliable sensitivity for malignancy. However, if the pre-procedural diagnosis is likely to be a malignancy other than lung cancer, and severe adhesions are present in the pleural cavity, the final pathological confirmation should be decided based on permanent paraffin sections, not only on fresh frozen sections.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the STARD reporting checklist. Available at http://dx.doi.org/10.21037/jtd-20-1809
Data Sharing Statement: Available at http://dx.doi.org/10.21037/jtd-20-1809
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/jtd-20-1809). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The Institutional Review Board of the Catholic University of Korea approved the study protocol in December 2019 (OC19RISI0180). Because this was a retrospective study, no consent was needed from the patients.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Porcel JM, Light RW. Pleural effusions. Dis Mon 2013;59:29-57. [Crossref] [PubMed]
- Rahman NM, Ali NJ, Brown G, et al. Local anaesthetic thoracoscopy: British Thoracic Society Pleural Disease Guideline 2010. Thorax 2010;65 Suppl 2:ii54-60. [Crossref] [PubMed]
- Skalski JH, Astoul PJ, Maldonado F. Medical thoracoscopy. Semin Respir Crit Care Med 2014;35:732-43. [Crossref] [PubMed]
- Lee P, Hsu A, Lo C, et al. Prospective evaluation of flex-rigid pleuroscopy for indeterminate pleural effusion: accuracy, safety and outcome. Respirology 2007;12:881-6. [Crossref] [PubMed]
- Froudarakis ME. New challenges in medical thoracoscopy. Respiration 2011;82:197-200. [Crossref] [PubMed]
- Hooper C, Lee YC, Maskell N, et al. Investigation of a unilateral pleural effusion in adults: British Thoracic Society Pleural Disease Guideline 2010. Thorax 2010;65 Suppl 2:ii4-17. [Crossref] [PubMed]
- Feller-Kopman DJ, Reddy CB, DeCamp MM, et al. Management of Malignant Pleural Effusions. An Official ATS/STS/STR Clinical Practice Guideline. Am J Respir Crit Care Med 2018;198:839-49. [Crossref] [PubMed]
- Roberts ME, Neville E, Berrisford RG, et al. Management of a malignant pleural effusion: British Thoracic Society Pleural Disease Guideline 2010. Thorax 2010;65 Suppl 2:ii32-40. [Crossref] [PubMed]
- Hallifax RJ, Corcoran JP, Psallidas I, et al. Medical thoracoscopy: Survey of current practice-How successful are medical thoracoscopists at predicting malignancy? Respirology 2016;21:958-60. [Crossref] [PubMed]
- Karpathiou G, Froudarakis M, Forest F, et al. Frozen Sections in Pleural Pathology: A Valuable Tool. Respiration 2017;94:45-51. [Crossref] [PubMed]
- Fielding D, Hopkins P, Serisier D. Frozen section of pleural biopsies at medical thoracoscopy assists in correctly identifying benign disease. Respirology 2005;10:636-42. [Crossref] [PubMed]
- Yap KH, Phillips MJ, Lee YC. Medical thoracoscopy: rigid thoracoscopy or flexi-rigid pleuroscopy? Curr Opin Pulm Med 2014;20:358-65. [Crossref] [PubMed]
- Husain AN, Colby TV, Ordonez NG, et al. Guidelines for Pathologic Diagnosis of Malignant Mesothelioma 2017 Update of the Consensus Statement From the International Mesothelioma Interest Group. Arch Pathol Lab Med 2018;142:89-108. [Crossref] [PubMed]
- Akyildiz EU. Intraoperative pathology consultation for pulmonary lesions: errors and deferrals. Int J Clin Exp Pathol 2015;8:7961-6. [PubMed]
- Abel EJ, Carrasco A, Culp SH, et al. Limitations of preoperative biopsy in patients with metastatic renal cell carcinoma: comparison to surgical pathology in 405 cases. BJU Int 2012;110:1742-6. [Crossref] [PubMed]
- Wilkinson N, Vroobel K, McCluggage W. Dataset for histopathological reporting of carcinomas and borderline tumours of the ovaries, fallopian tubes and peritoneum. 2019.


