Full or hypocaloric nutritional support for the critically ill patient: is less really more?
In critically ill patients we typically observe a catabolic response and changes in metabolic demands varying from increased energy expenditure during the initial inflammatory response to decreased energy expenditure in later phases of critical illness. In addition, sedation and immobilization may reduce exercise-induced energy expenditure in all stages of intensive care unit (ICU) stay. Therefore, it is recommended to estimate energy expenditure based on indirect calorimetry. However, the availability of such devices in ICUs is low. As a consequence most healthcare providers still use formulae to calculate the estimated energy expenditure, although these estimates have been shown to be unreliable (1).
Catabolism is more rule than exception in ICU patients and is characterized by increased protein breakdown, a negative nitrogen balance and loss of lean body mass (LBM). This potentially destructive metabolic response may also be seen as adaptive to severe injury or stress in an attempt to secure or promote optimal supply of amino acids to organs to serve as substrates for gluconeogenesis and for the synthesis of various proteins such as acute phase proteins and proteins necessary for immune defense and wound repair. Furthermore, it may provide energy substrate for fast replicating cells such as immune cells and enterocytes (2).
The severity of protein degradation may lead to extensive muscle wasting, recently quantified during the first 10 days after ICU admission up to 15-20% of the muscle mass, negatively affecting outcome. The loss of muscle mass is more pronounced in patients suffering from multiple organ dysfunction syndrome than in patients with single organ failure (3).
Hypocaloric and hypercaloric feeding in critically ill patients
In an observational study in ICU patients Villet frequently encountered a negative cumulative energy balance of >10,000 kcal/week and was able to show an association with complications, mainly infections (4). This observation lead to a widespread assumption that energy deficit should be prevented and still it is called the cumulative energy deficit hypothesis. In most critically ill patients, due to the severity of illness and critical care therapy normal oral nutritional intake is inadequate, impractical or impossible. Therefore, enteral or parenteral provision of calories, proteins, electrolytes, vitamins, minerals, trace elements, and fluids is necessary.
Hypercaloric feeding or overfeeding defined as providing too many calories (>110% of the calculated or measured energy target), has been proven to confer deleterious effects on outcome. Consequences of overfeeding are insulin resistance and hyperglycemia, hepatic steatosis, prolonged organ support such as mechanical ventilation and even increased mortality (5).
For decades the optimal dose of nutritional support for critically ill patient is heavily debated. Some recommend full nutritional support others advocate the use of so-called trophic or trickle feeding to prevent negative effects of starvation to the gut, such as mucosal atrophy, reduced absorption of nutrients and (bacterial) translocation (6).
The terminology is divergent and confusing: permissive underfeeding, trophic feeding, trickle feeding, and hypocaloric feeding are frequently used to describe specific nutritional strategies. Permissive underfeeding suggests that lower total nutritional intake (calories, proteins and micronutrients) is acceptable. Hypocaloric feeding implies that only energy intake is lower. However, hypocaloric intake can be realized by reducing carbohydrate, protein or fat macronutrients. Trophic feeding and trickle feeding have no clear definition, however it is generally accepted that according to this nutritional strategy an intake of 10-20 mL enteral feeding per hour or a maximum of 500-1,000 kcal per day is meant. To make matters more complex, some use supplemental parenteral nutrition (SPN) to meet the total daily energy and protein targets. In case SPN is added total energy and protein deficit will no longer be present. In this case effects of limiting enteral intake only are studied and not effects of hypocaloric or permissive underfeeding.
The nutritional risk of ICU patients can vary on ICU admission. A new instrument [Nutrition Risk in the Critically Ill (NUTRIC) score] to assess the nutritional status of critically ill patients has recently been developed. From validation data of the NUTRIC score we learned that nutritional interventions do not confer similar effects in patients with different baseline risks, in other words benefits of nutritional support can only be detected in patients with high nutritional risk and advantages or disadvantages of such interventions may go undetected in patients with low nutritional risk. Conversely, effects of hypocaloric feeding may not be less beneficial than full nutritional support in patients with low nutritional risk (NUTRIC score <5) (7).
Consequently, it is important to carefully review recently published large observational and randomized studies to evaluate these aspects to better understand their implications for daily practice.
Observational studies on caloric intake: contradictory results
Early enteral nutrition is advocated for critically ill patients and preferred over parenteral nutrition (8). In addition, several observational studies on enteral nutrition have demonstrated that prescribed caloric goals are rarely achieved. Furthermore, based on some older observational studies it was concluded that patients that received the lowest intake of calories showed the best outcomes, possibly due to better metabolic consequences of lower intake (9).
In contrast, Alberda reported data on 2,772 mechanically ventilated patients who only received an average of 1,034 kcal/day and 47 g protein/day. In their analysis an increase of 1,000 kcal/day was associated with reduced mortality (OR 60-day mortality 0.76) and an increase in ventilator free days. Strikingly, they showed an association of increased calories and lower mortality observed in patients with a BMI <25 and >35 with no benefit for patients with a BMI 25-35. Similar effects on mortality were observed when comparing increasing protein intake (10).
How can these contradictory observations be explained?
Heyland reported data from a prospective, multinational audit involving 7,872 mechanically ventilated, critically ill patients that may help to understand these contradictory results. In an initial unadjusted analysis, a significant association between increased caloric intake and increased mortality (OR 1.28, 95% CI: 1.12-1.48 for patients receiving >2/3 of their caloric prescription versus those receiving <1/3) was noted (11). These data would confirm the hypocaloric feeding concept. However, during the first days after ICU admission a step-up approach of increasing delivery of (enteral) nutrition (i.e., steps of 20 mL/h·day−1 increase) is common. Therefore, ICU patients that stay for shorter periods will have received less nutritional support. Thus, the association of short length of stay (LOS) and beneficial effects of hypocaloric feeding may due to a better prognosis in patients with a short LOS. In addition, on days near the full progression to oral intake, nutritional support will be tapered suggesting benefits of lower intake. In order to circumvent these aspects Heyland reanalyzed the database excluding data from the first and last days, and showed that patients that received >2/3 of their caloric prescription were much less likely to die (OR 0.67, 95% CI: 0.56-0.79) (11).
The importance of energy and protein
Both energy and protein intake are important for critically ill patients. In a small mechanistic study Berg showed that hypocaloric feeding (50% of target) was associated with a more negative protein balance, due to reduced protein synthesis, without affecting the amino acid oxidation and breakdown, suggesting that hypocaloric feeding could aggravate loss of muscle mass (12).
Weijs in an observational study clearly demonstrated that higher protein intake is associated with better survival. Meeting only caloric targets without meeting the protein demands does not confer the same mortality reduction as when also protein targets are reached (13). The caloric target with the lowest mortality is around 85% of target (11).
Randomized trials on trophic and full nutritional support
Until now five relevant randomized trials have been published (see Table 1). In the first Arabi trial permissive underfeeding was studied in a 2×2 factorial, randomized, controlled design with the cointervention intensive insulin therapy resulting in a reduction of in-hospital mortality (14). Rice studied trophic feeding in 1,000 ventilated patients with acute lung injury without significant effects on infections, mortality or LOS (15). Petros compared the impact of normocaloric (100% of measured energy expenditure) vs. hypocaloric feeding (50%) in critically ill patients during the first 7 ICU days (16). ICU and hospital mortality were non-significant, however significant more infections in the hypocaloric group were encountered. Charles studied hypocaloric feeding in surgical critically ill patients and found no differences on major endpoints (17).
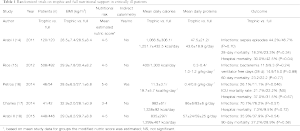
Full table
Recently the permit trial (Arabi-II) was published, assigning 894 critically ill adults with a medical, surgical, or trauma admission category to permissive underfeeding (40% to 60% of calculated caloric requirements) or standard enteral feeding (70% to 100%) for up to 14 days while maintaining a similar protein intake in the two groups. The primary outcome was 90-day mortality (18). Lower protein intake in the permissive underfeeding group was compensated by provision of enteral protein supplements. Protein intake was similar in the two groups (57±24 and 59±25 g per day, respectively; P=0.29). Enteral feeding to deliver a moderate amount of nonprotein calories to critically ill adults was not associated with lower mortality than that associated with planned delivery of a full amount of nonprotein calories.
Interpretation of study data
In most studies addressing hypocaloric feeding no indirect calorimetry was used, limiting the validity of results. The importance of optimizing energy and protein delivery by repeated indirect calorimetry measurements was recently demonstrated by Singer and coworkers in a prospective pilot clinical trial in 130 mechanically ventilated patients randomized to receive enteral nutrition with an energy target determined by indirect calorimetry or 25 kcal/kg/day. Enteral nutrition (EN) was supplemented with parenteral nutrition (PN) when required. The indirect calorimetry group had a higher mean energy (2,086±460 vs. 1,480±356 kcal/day) and protein intake (76±16 vs. 53±16 g/day) and there was a trend towards improved hospital mortality. However, duration of ventilation and ICU stay was increased (19).
Heyland suggested that increasing caloric and protein intake only is associated with improved clinical outcome among patients with higher nutritional risk profiles (7). In most studies both the intervention and full support groups received lower than recommended caloric intakes, and in fact both represent hypocaloric groups. In the Arabi I trial the caloric intake difference was only 200 kcal and thus non-discriminatory. In addition, some studies do not have isonitrogenous arms (marked differences in protein intake). As protein intake is relevant for outcome this may potentially confound effects of hypocaloric feeding.
Most importantly, most studies have included relatively young, well-nourished (high BMI) patients with low nutritional risk (NUTRIC score 5 or lower). For example the caloric intake in the Arabi II trial (mean 10 vs. 16 kcal/kg·day−1, respectively) and protein intake achieved (mean 0.7 g/kg·day−1 in both groups) was far below the recommended intake. Similar to the rice trial no differences were observed as most patients were young (mean age 51 years) and well-nourished (mean BMI 29.3). In the only trial with higher nutritional risk and measured energy expenditure hypocaloric feeding was associated with increased infectious morbidity (16). Furthermore, functional outcomes in all studies were not investigated, although long-term outcomes have been shown to be associated with feeding adequacy (20).
Conclusions and future directions
Most randomized studies addressing the concept of trophic, trickle or hypocaloric feeding or permissive underfeeding, have shown no major impact on outcome. This could suggest that hypocaloric feeding is as good as full nutritional support. This may be true for the specific patient groups studied. However, it is important to notice that in some studies additional protein supplements have been used to meet protein requirements during hypocaloric feeding. Still in most studies both arms did not meet recommended caloric and protein requirements. Furthermore, long-term effects were not studied. As in general patients studied were younger and had lower nutritional risk the external validity is limited for many ICUs as many ICU patients have high-nutritional risk scores.
Therefore, extrapolation of the hypocaloric feeding concept to high-risk patients cannot be recommended. Studies on hypocaloric feeding in ICU patients with high nutritional risk are warranted. Until results of these studies are available I suggest aiming for primary full enteral support, probably leading to an optimal caloric intake of 85% of target (as enteral support rarely achieves the 100% target). This may potentially positively influence long-term outcome and does not seem to increase risk.
Full or hypocaloric nutritional support for the critically ill patient: is less really more? No, not more in few, potentially less in many. Keep optimally feeding your critically ill patients.
Acknowledgements
None.
Footnote
Provenance: This is a Guest Editorial commissioned by the Section Editor Ming, Zhong (Department of Critical Care Medicine, Zhongshan Hospital, Fudan University, Shanghai, China).
Conflicts of Interest: Dr. Arthur R.H. van Zanten reported that he has received honoraria for advisory board meetings, lectures, and travel expenses from Abbott, Baxter, BBraun, Danone, Fresenius Kabi, Nestle, Novartis, and Nutricia. Inclusion fees for patients included in clinical trials were paid to the local ICU research foundation.
References
- Tatucu-Babet OA, Ridley EJ, Tierney AC. The Prevalence of Underprescription or Overprescription of Energy Needs in Critically Ill Mechanically Ventilated Adults as Determined by Indirect Calorimetry: A Systematic Literature Review. JPEN J Parenter Enteral Nutr 2015. [Epub ahead of print]. [PubMed]
- Puthucheary Z, Montgomery H, Moxham J, et al. Structure to function: muscle failure in critically ill patients. J Physiol 2010;588:4641-8. [PubMed]
- Puthucheary ZA, Rawal J, McPhail M, et al. Acute skeletal muscle wasting in critical illness. JAMA 2013;310:1591-600. [PubMed]
- Villet S, Chiolero RL, Bollmann MD, et al. Negative impact of hypocaloric feeding and energy balance on clinical outcome in ICU patients. Clin Nutr 2005;24:502-9. [PubMed]
- Klein CJ, Stanek GS, Wiles CE 3rd. Overfeeding macronutrients to critically ill adults: metabolic complications. J Am Diet Assoc 1998;98:795-806. [PubMed]
- Preiser JC, van Zanten AR, Berger MM, et al. Metabolic and nutritional support of critically ill patients: consensus and controversies. Crit Care 2015;19:35. [PubMed]
- Heyland DK, Dhaliwal R, Jiang X, et al. Identifying critically ill patients who benefit the most from nutrition therapy: the development and initial validation of a novel risk assessment tool. Crit Care 2011;15:R268. [PubMed]
- McClave SA, Martindale RG, Vanek VW, et al. Guidelines for the Provision and Assessment of Nutrition Support Therapy in the Adult Critically Ill Patient: Society of Critical Care Medicine (SCCM) and American Society for Parenteral and Enteral Nutrition (A.S.P.E.N.). JPEN J Parenter Enteral Nutr 2009;33:277-316. [PubMed]
- Boitano M. Hypocaloric feeding of the critically ill. Nutr Clin Pract 2006;21:617-22. [PubMed]
- Alberda C, Gramlich L, Jones N, et al. The relationship between nutritional intake and clinical outcomes in critically ill patients: results of an international multicenter observational study. Intensive Care Med 2009;35:1728-37. [PubMed]
- Heyland DK, Cahill N, Day AG. Optimal amount of calories for critically ill patients: depends on how you slice the cake! Crit Care Med 2011;39:2619-26. [PubMed]
- Berg A, Rooyackers O, Bellander BM, et al. Whole body protein kinetics during hypocaloric and normocaloric feeding in critically ill patients. Crit Care 2013;17:R158. [PubMed]
- Weijs PJ, Stapel SN, de Groot SD, et al. Optimal protein and energy nutrition decreases mortality in mechanically ventilated, critically ill patients: a prospective observational cohort study. JPEN J Parenter Enteral Nutr 2012;36:60-8. [PubMed]
- Arabi YM, Tamim HM, Dhar GS, et al. Permissive underfeeding and intensive insulin therapy in critically ill patients: a randomized controlled trial. Am J Clin Nutr 2011;93:569-77. [PubMed]
- National Heart, Lung, and Blood Institute Acute Respiratory Distress Syndrome (ARDS) Clinical Trials Network, Rice TW, Wheeler AP, et al. Initial trophic vs full enteral feeding in patients with acute lung injury: the EDEN randomized trial. JAMA 2012;307:795-803.
- Petros S, Horbach M, Seidel F, et al. Hypocaloric vs Normocaloric Nutrition in Critically Ill Patients: A Prospective Randomized Pilot Trial. JPEN J Parenter Enteral Nutr 2014. [Epub ahead of print]. [PubMed]
- Charles EJ, Petroze RT, Metzger R, et al. Hypocaloric compared with eucaloric nutritional support and its effect on infection rates in a surgical intensive care unit: a randomized controlled trial. Am J Clin Nutr 2014;100:1337-43. [PubMed]
- Arabi YM, Aldawood AS, Haddad SH, et al. Permissive Underfeeding or Standard Enteral Feeding in Critically Ill Adults. N Engl J Med 2015;372:2398-408. [PubMed]
- Singer P, Anbar R, Cohen J, et al. The tight calorie control study (TICACOS): a prospective, randomized, controlled pilot study of nutritional support in critically ill patients. Intensive Care Med 2011;37:601-9. [PubMed]
- Wei X, Day AG, Ouellette-Kuntz H, et al. The Association Between Nutritional Adequacy and Long-Term Outcomes in Critically Ill Patients Requiring Prolonged Mechanical Ventilation: A Multicenter Cohort Study. Crit Care Med 2015;43:1569-79. [PubMed]


