
Influence of operator volume on early outcomes of septal myectomy for isolated hypertrophic obstructive cardiomyopathy
Introduction
Hypertrophic cardiomyopathy (HCM) is a common genetic cardiovascular disease characterized by myocardial hypertrophy. A community epidemiological survey showed that the prevalence of HCM was 0.8% and that there are approximately 1 million patients with HCM in China (1).Approximately 70% of patients with HCM have left ventricular outflow tract (LVOT) obstruction, either at rest or with physiologic (exercise) provocation [defined as hypertrophic obstructive cardiomyopathy (HOCM)] (2), which significantly increases the risk for heart failure and death (3,4).
Surgical septal myectomy, when performed in experienced centres, is the first consideration for HOCM patients with severe drug-refractory symptoms (5). Through muscular resection and removal of the abnormal chordae or management of the mitral valve leaflet (6,7), septal myectomy can immediately ameliorate obstruction and relieve mitral regurgitation (8-11), leading to the restoration of diastolic function (12). The long-term survival after successful surgery has no difference from that of the general population of the same age and gender (13-15). However, HCM is a disease of substantial heterogeneity, and only a minority of patients (≤10%) would initially qualify for surgical septal myectomy (16), which is a technically challenging operation.
The American College of Cardiology Foundation (ACCF), the American Heart Association (AHA) and the European Society of Cardiology guidelines on the diagnosis and management of HCM recommend that septal reduction therapy only be performed by experienced operators (at least 20 septal myectomy procedures) in the context of a comprehensive HCM clinical programme (5,17). Nevertheless, data regarding the detailed impacts of operator volume on the results of HCM surgical treatment are limited. The purpose of this study is to address this issue.
We present the following article in accordance with the STROBE reporting checklist (available at http://dx.doi.org/10.21037/jtd-20-2070).
Methods
Study population
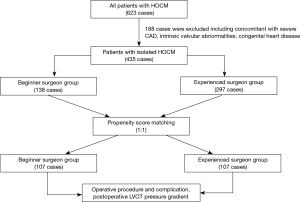
From January 2002 to December 2014, 623 consecutive patients with HOCM underwent surgical treatment in our hospital. A total of 435 patients were retrospectively enrolled, and 188 patients with coronary heart disease and/or intrinsic valvular abnormalities and/or congenital heart disease who needed concomitant surgical treatment were excluded. The reason we did not include patients receiving surgery in the last 5 years is that very few cases were recently assigned to unexperienced surgeons (or beginner surgeons). The diagnosis of HCM was established by the detection of septal hypertrophy on echocardiography or magnetic resonance imaging (MRI) when the maximal septal thickness was at least 13 mm in the absence of another cardiac or systemic disease that would be responsible for the degree of left ventricular (LV) hypertrophy identified (18).HOCM was diagnosed when HCM presented with an LVOT pressure gradient of 30 mmHg or greater. All patients who underwent septal myectomy had severe drug-refractory symptoms and a dynamic LVOT pressure gradient of 50 mmHg or greater at rest or a physiologic provocation condition associated with septal hypertrophy and systolic anterior motion (SAM) of the mitral valve. The study design and patient flow diagram are displayed in Figure 1. The study protocol was approved (No. 2016-790), and informed consent was waived by the Institutional Review Board of Fuwai Hospital, which was in accordance with the Helsinki Declaration (as revised in 2013).
Surgical technique
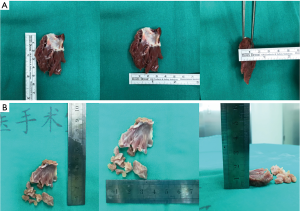
The standard surgical procedures were similar to those reported previously (19,20). In short, septal myectomy was performed through an oblique aortotomy to sufficiently expose the subaortic septum. The target size of the septal myectomy included the following: the length ranged from 3 to 5 mm below the aortic annulus to the level of the papillary muscle or apex. The width ranged from approximately 5 mm left of the membranous septum to the anterolateral free wall of the left ventricle near the anterior commissure of the mitral valve. The depth of the resection was 40% to 50% of the thickness at the site of myectomy. Abnormal chordal structure and anomalous fibrous or muscle attachments to the mitral valve or ventricular septum or free wall were excised. Detailed preoperative echocardiographic guidance of the procedure was provided by intraoperative transesophageal echocardiography. The representative myocardial specimens excised by an experienced and beginner operator are shown in Figure 2.
Propensity score matching
According to the 2011 ACCF/AHA guidelines for the diagnosis and treatment of HCM, an experienced surgeon (ES) was defined as an individual operator with a cumulative case volume of at least 20 septal myectomy procedures, and a beginner surgeon (BS) was defined as an individual operator with a cumulative case volume of ≤20 septal myectomy procedures (5). All beginner surgeons participated in many septal myectomies and had rich experience in other cardiac operations before they performed this procedure independently. We performed rigorous adjustments for baseline differences using a propensity score with 1:1 matching (21). To estimate the propensity score (PS), a logistic regression model predicting the patients undergoing operations by ES or BS was developed, with the covariates including the previously reported risk factors (22,23) of sex, interventricular septal thickness, LVOT pressure gradient, left atrial diameter, complete right bundle-branch blockage (RBBB), and mitral valve regurgitation. The PS score model demonstrated good calibration, as the P value was 0.185 for the Hosmer and Lemeshow goodness of fit test. The accuracy was moderately good, with an AUC of 0.712.
We created a matched sample by matching ES or BS on the logit of the propensity score using callipers of width equal to 0.2 of the standard deviation of the logit of the propensity score. An aggressive, nearest-neighbour matching algorithm was employed to form pairs. The absolute standardized differences were used to compare the balance in baseline covariates between groups, and imbalance was defined as an absolute value greater than 0.2. Finally, 214 matched patients (107:107) were included. The groups were defined as the ES group and BS group (Figure 1). In the BS group, 29 surgeons who had performed ≤20 cases were included. In the ES group, two operators who had completed more than 20 procedures were included.
Endpoints
The primary endpoint was the incidence of residual LVOT obstruction after the procedure. Residual LVOT obstruction was defined as a LVOT pressure gradient of 30 mmHg or greater by echocardiography. The secondary endpoints included a composite of postoperative maximal septal thickness, postoperative LVOT pressure gradient, incidence of concomitant mitral valve replacement, postoperative mitral regurgitation, and procedural complications (mortality, interventricular septal perforation, permanent pacemaker implantation). Operative death included all deaths within the same hospitalization after myectomy. The degree of mitral regurgitation was assessed on a scale of 0 to 4 (0, none; 1, mild; 2, moderate; 3, moderate to severe; and 4, severe) by using multiple different Doppler criteria.
Statistical analysis
Based on previous observations, we estimated that the incidence of residual LVOT obstruction in the ES group would be 5%; hence, the current sample size of 107 in both groups would provide 80% power. A 5% level of significance detected a 12% or more increase in the incidence of residual LVOT obstruction for the BS group.
Inpatient data were collected by trained clinical research staff and entered into a computer database by two independent investigators. Continuous variables were reported as the mean ± standard deviation (SD), and comparisons between groups were performed using Student’s t-test. Categorical variables were reported as percentages, and differences among groups were assessed using Fisher’s exact test or the chi-squared test. Missing values were imputed using multiple imputation.
All statistical testing was two-sided, at a significance level of P<0.05. We conducted all analyses using SAS software, version 9.4 (SAS Institute Inc., Cary, North Carolina).
Results
In 435 patients, there was a predominantly male population with a mean age of 43.0±13.4 years. Although 70 (16.1%) patients had a history of hypertension, imaging showed a predominantly asymmetric hypertrophy that could not be attributed to hypertension in these patients. Fifteen (3.4%) patients had previous alcohol septal ablation, and postoperative complete RBBB had occurred in 20% of patients. Only a very small number of patients (1.4%) had a family history of sudden death, while nearly 15.4% of patients had an interventricular septum thickness ≥30 mm; these two factors are the traditional HCM risk factors for sudden death. All patients had a significantly increased LVOT pressure gradient (≥50 mmHg) at rest or a physiologically provocative condition. Despite maximally tolerated medical treatment, nearly half of the patients (51.3%) had a significantly reduced New York Heart Association classification (NYHA III or IV). No patient had intrinsic abnormalities of the mitral valve on echocardiography. After matching, no statistically significant difference was found between the two groups.
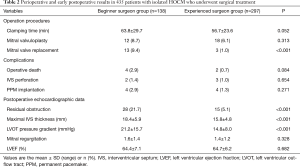
Baseline characteristic differences in age, NYHA classification, drug treatment history and left ventricular ejection fraction were found between the ES group and the BS group (Table 1). Operative death occurred in 6 patients (1.4%). There was a shorter clamp time (56.7±23.6 min in ES vs. 63.8±29.7 min in BS, P=0.052) and lower mortality (0.7% in ES vs. 2.9% in BS, P=0.084) in the ES group, although neither reached statistical significance. In both groups, less than 10% of patients underwent concomitant mitral valvuloplasty to relieve mitral valve regurgitation or LVOT obstruction, and the percentage was comparable. However, mitral valve replacement was performed more often to alleviate LVOT obstruction in the BS group (1% in ES vs. 9.4% in BS, P<0.001), although no significant intrinsic valvular abnormalities were shown during intraoperative transesophageal echocardiography. The major reasons for mitral valve replacement included inadequate myocardial resection and failed mitral valvuloplasty, and the latter was the primary reason for the ES group.

Full table
In the ES group, interventricular septal perforation occurred in 5 (1.1%) patients, and 8 (1.8%) patients received permanent pacemaker implantation due to complete atrioventricular blockage. Between the two groups, no significant difference was found in the incidence of these two common complications. On postoperative echocardiography, mitral valve regurgitation was less than moderate in 99.5% of patients, and no patients had significant (greater than mild) aortic valve regurgitation. However, in the BS group, the maximal interventricular septal thickness (18.4±5.9 mm in BS vs. 15.8±4.8 mm in ES, P<0.001), LVOT pressure gradient (21.2±15.7 mmHg in BS vs. 14.8±8.0 mmHg in ES, P<0.001), and incidence of residual LVOT obstruction (21.7% in BS vs. 5.1% in ES, P<0.001) were greater than those in the ES group (Table 2).
Full table
After propensity score matching, there were 107 pairs of BS vs. ES patients. Standardized differences in baseline covariates were below 0.2 (Table 1), indicating adequate control of possible confounding associated with the observed covariates.
There was no significant difference in the clamp time between the two groups, and the degree of postoperative mitral regurgitation was also comparable (0.6±0.5 in BS vs. 0.7±0.5 in ES, P=0.269). Nevertheless, concomitant mitral valvuloplasty (9.4% vs. 5.6%, P<0.001) and replacement (11.2% vs. 1.9%, P<0.001) were more common in the BS group. Furthermore, the incidence of permanent pacemaker implantation was lower in the ES group (1.9% vs. 3.7%, P<0.001), but no difference was found in the surgical mortality (1.9% vs. 1.9%) or the incidence of interventricular septal perforation between the two groups. In the BS group, compared to ES, a higher LVOT pressure gradient (20.73±15.10 vs. 14.32±7.37 mmHg, P<0.001), higher incidence of residual LVOT obstruction (18.7% vs. 0.9%, P<0.003), and thicker interventricular septum (18.78±5.99 vs. 15.91±5.27 mm, P<0.001) were found postoperatively (Table 3). Patients with residual obstruction did not undergo corrective surgery at discharge and were instead treated with oral drugs.
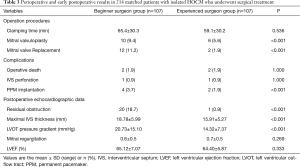
Full table
Discussion
This is a retrospective study on the surgical treatment for HOCM with a large sample size. In this study, we focused on the impact of operator volume on the outcome of septal myectomy for isolated HOCM. Our study showed that the operator volume is an important factor in achieving better results for septal myectomy procedures.
Several retrospective studies with large cohorts have reported excellent early and late results after surgical treatment for HOCM (8,13-15,22-25). In this study, we showed that myectomy could relieve LVOT obstruction and mitral regurgitation immediately after surgery, while the mortality and incidence of major complications were relatively low. In the original ES group, operators could achieve a mortality rate of <1% and a major complications rate of <3%, with documented success in both haemodynamic and functional benefits, which was comparable to other experienced centres (5).
Transaortic septal myectomy is currently considered the most effective method for treating HOCM. However, although HCM is relatively common in the general population, septal myectomy is infrequently performed in general clinical practice. The narrow surgical exposure field and the fear of interventricular septal perforation and complete heart blockage by excessive resection are the predominant challenges for most surgeons. A total of 435 consecutive patients were operated on by 29 surgeons within 13 years in this study. However, more and more septal myectomies were only performed by two experienced surgeons since the guidelines recommended that septal reduction therapy should be performed only by experienced operators in 2011 and 2014. Therefore, we enrolled operations performed by 29 surgeons before 2014 to ascertain the impact of operator volume on early myectomy results.
Panaich et al. reported that the operator volume was associated with a lower rate of complications and mortality, although without statistical significance (26). Our study demonstrated that, in the ES group, the alleviation of LVOT obstruction was more adequate, while a lower incidence of permanent pacemaker implantation and concomitant mitral valve replacement was found. The reason might be related to two important aspects of myectomy. The first is that the correct and extended range of myocardium resection is essential to eliminate LVOT obstruction, and it requires more practice and experience. The other important aspect is that proper management of the anomalous connection of the mitral valve is associated with operators’ individual experience. It was critical to release the anomalous connection of the subvalvular apparatus of the mitral valve, which could make the mitral valve coaptation closer to LVOT and contribute to the development of SAM. If the anomalous connection was not managed properly, there would be a risk of residual SAM and obstruction.
Kim et al. reported that a higher incidence of in-hospital death was associated with lower-volume centres, which indicated that operator experience is an important impact factor of early results after septal myectomy (27). In this study, there was no difference in operation death, with higher tendencies in the beginner surgeon group. The reasons may include limited sample size, patient selection, more conservative removal of the hypertrophic myocardium, and experience in cardiac surgery.
Our results might be frustrating for beginner surgeons, and it might be more difficult for them to gain experience, which is not the purpose of this study. We believe that for beginner surgeons who are dedicated to the surgical treatment of HOCM, it is essential to participate in myectomy procedures as an assistant as much as possible. When they eventually perform this procedure, perhaps suitable patient selection could lead to a better result, such as patients with a large aortic annulus and locally hypertrophied ventricular septum, rather than those with diffuse hypertrophy or severe mitral regurgitation.
There are several limitations to this study. First, the analysis is possibly biased, since this study is a single-centre retrospective study, and the results might not be extrapolated into general practice. Second, according to 2011 ACCF/AHA guidelines for the diagnosis and treatment of HCM, we defined a cut-off point of 20 in the operator volume for operator grouping, which was an empirical definition. Other factors, such as the frequency of procedures, might also evaluate the experience of the surgeons. However, an accurate cut-off point of surgical volumes or the frequency of procedures requires analysis with a larger sample size. Third, this study only illustrates the impact of operator volume on the early results. The impacts of operator volume on the long-term results require follow-up. In addition, because of the long period and many surgeons involved in this study, we did not evaluate the weight of the specimen excised in all patients, which might provide evidence to further understand the differences between ES and BS.
Conclusions
The operator volume is an important factor in achieving better obstruction obliteration after septal myectomy in patients with isolated HCM. The concrete impacts of operator volume on the long-term results need to be confirmed.
Acknowledgments
We appreciate all the operators and staff who have participated in the surgical treatment of HOCM in Fuwai Hospital.
Funding: None.
Footnote
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at http://dx.doi.org/10.21037/jtd-20-2070
Data Sharing Statement: Available at http://dx.doi.org/10.21037/jtd-20-2070
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/jtd-20-2070). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by the institutional ethics board of Fuwai Hospital (No. 2016-790) and informed consent was waived.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Maron BJ. The 2009 international hypertrophic cardiomyopathy summit. Am J Cardiol 2010;105:1164-8. [Crossref] [PubMed]
- Maron MS, Olivotto I, Zenovich AG, et al. Hypertrophic cardiomyopathy is predominantly a disease of left ventricular outflow tract obstruction. Circulation 2006;114:2232-9. [Crossref] [PubMed]
- Maron MS, Olivotto I, Betocchi S, et al. Effect of left ventricular outflow tract obstruction on clinical outcome in hypertrophic cardiomyopathy. N Engl J Med 2003;348:295-303. [Crossref] [PubMed]
- Elliott PM, Gimeno JR, Tome MT, et al. Left ventricular outflow tract obstruction and sudden death risk in patients with hypertrophic cardiomyopathy. Eur Heart J 2006;27:1933-41. [Crossref] [PubMed]
- Gersh BJ, Maron BJ, Bonow RO, et al. 2011 ACCF/AHA guideline for the diagnosis and treatment of hypertrophic cardiomyopathy: executive summary: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. Circulation 2011;124:2761-96. [Crossref] [PubMed]
- van der Lee C, Kofflard MJ, van Herwerden LA, et al. Sustained improvement after combined anterior mitral leaflet extension and myectomy in hypertrophic obstructive cardiomyopathy. Circulation 2003;108:2088-92. [Crossref] [PubMed]
- Balaram SK, Tyrie L, Sherrid MV, et al. Resection-plication-release for hypertrophic cardiomyopathy: clinical and echocardiographic follow-up. Ann Thorac Surg 2008;86:1539-44; discussion 1544-5. [Crossref] [PubMed]
- Smedira NG, Lytle BW, Lever HM, et al. Current effectiveness and risks of isolated septal myectomy for hypertrophic obstructive cardiomyopathy. Ann Thorac Surg 2008;85:127-33. [Crossref] [PubMed]
- Minakata K, Dearani JA, O'Leary PW, et al. Septal myectomy for obstructive hypertrophic cardiomyopathy in pediatric patients: early and late results. Ann Thorac Surg 2005;80:1424-9; discussion 1429-30. [Crossref] [PubMed]
- Deb SJ, Schaff HV, Dearani JA, et al. Septal myectomy results in regression of left ventricular hypertrophy in patients with hypertrophic obstructive cardiomyopathy. Ann Thorac Surg 2004;78:2118-22. [Crossref] [PubMed]
- Franke A, Schondube FA, Kuhl HP, et al. Quantitative assessment of the operative results after extended myectomy and surgical reconstruction of the subvalvular mitral apparatus in hypertrophic obstructive cardiomyopathy using dynamic three-dimensional transesophageal echocardiography. J Am Coll Cardiol 1998;31:1641-9. [Crossref] [PubMed]
- Monteiro PF, Ommen SR, Gersh BJ, et al. Effects of surgical septal myectomy on left ventricular wall thickness and diastolic filling. Am J Cardiol 2007;100:1776-8. [Crossref] [PubMed]
- Ommen SR, Maron BJ, Olivotto I, et al. Long-term effects of surgical septal myectomy on survival in patients with obstructive hypertrophic cardiomyopathy. J Am Coll Cardiol 2005;46:470-6. [Crossref] [PubMed]
- Vriesendorp PA, Schinkel AF, Soliman OI, et al. Long-term benefit of myectomy and anterior mitral leaflet extension in obstructive hypertrophic cardiomyopathy. Am J Cardiol 2015;115:670-5. [Crossref] [PubMed]
- Balaram SK, Ross RE, Sherrid MV, et al. Role of mitral valve plication in the surgical management of hypertrophic cardiomyopathy. Ann Thorac Surg 2012;94:1990-7; discussion 1997-8. [Crossref] [PubMed]
- Olivotto I, Ommen SR, Maron MS, et al. Surgical myectomy versus alcohol septal ablation for obstructive hypertrophic cardiomyopathy. Will there ever be a randomized trial? J Am Coll Cardiol 2007;50:831-4. [Crossref] [PubMed]
- Borger MA, Elliott PM, Anastasakis A, et al. 2014 ESC Guidelines on diagnosis and management of hypertrophic cardiomyopathy: the Task Force for the Diagnosis and Management of Hypertrophic Cardiomyopathy of the European Society of Cardiology (ESC). Eur Heart J 2014;35:2733-79. [Crossref] [PubMed]
- Maron BJ, McKenna WJ, Danielson GK, et al. American College of Cardiology/European Society of Cardiology clinical expert consensus document on hypertrophic cardiomyopathy. A report of the American College of Cardiology Foundation Task Force on Clinical Expert Consensus Documents and the European Society of Cardiology Committee for Practice Guidelines. J Am Coll Cardiol 2003;42:1687-713. [Crossref] [PubMed]
- Wang S, Cui H, Yu Q, et al. Excision of anomalous muscle bundles as an important addition to extended septal myectomy for treatment of left ventricular outflow tract obstruction. J Thorac Cardiovasc Surg 2016;152:461-8. [Crossref] [PubMed]
- Liu Y, Song Y, Gao G, et al. Outcomes of an extended Morrow procedure without a concomitant mitral valve procedure for hypertrophic obstructive cardiomyopathy. Sci Rep 2016;6:29031. [Crossref] [PubMed]
- Li F, Zaslavsky AM, Landrum MB. Propensity score weighting with multilevel data. Stat Med 2013;32:3373-87. [Crossref] [PubMed]
- Woo A, Williams WG, Choi R, et al. Clinical and echocardiographic determinants of long-term survival after surgical myectomy in obstructive hypertrophic cardiomyopathy. Circulation 2005;111:2033-41. [Crossref] [PubMed]
- Desai MY, Bhonsale A, Smedira NG, et al. Predictors of long-term outcomes in symptomatic hypertrophic obstructive cardiomyopathy patients undergoing surgical relief of left ventricular outflow tract obstruction. Circulation 2013;128:209-16. [Crossref] [PubMed]
- Delmo Walter EM, Javier MF, Hetzer R. Long-term outcome of simultaneous septal myectomy and anterior mitral leaflet retention plasty in hypertrophic obstructive cardiomyopathy: the Berlin experience. Ann Cardiothorac Surg 2017;6:343-52. [Crossref] [PubMed]
- Iacovoni A, Spirito P, Simon C, et al. A contemporary European experience with surgical septal myectomy in hypertrophic cardiomyopathy. Eur Heart J 2012;33:2080-7. [Crossref] [PubMed]
- Panaich SS, Badheka AO, Chothani A, et al. Results of ventricular septal myectomy and hypertrophic cardiomyopathy (from Nationwide Inpatient Sample [1998-2010]). Am J Cardiol 2014;114:1390-5. [Crossref] [PubMed]
- Kim LK, Swaminathan RV, Looser P, et al. Hospital volume outcomes after septal myectomy and alcohol septal ablation for treatment of obstructive hypertrophic cardiomyopathy: US nationwide inpatient database, 2003-2011. JAMA Cardiol 2016;1:324-32. [Crossref] [PubMed]


