
Development of the fundamentals of thoracic robotic surgery curriculum
Introduction
A great technological revolution in surgery occurred with the introduction of laparoscopic and other minimally invasive procedures, with enormous patient benefits. Many randomized trials have demonstrated the benefits of minimally invasive surgery over traditional open surgery (1-4). The use of minimally invasive techniques has now penetrated many specialties, such as general surgery, gynecology, urology, colorectal surgery, thoracic surgery, and others.
Robotic-assisted surgery (RAS) is a form of minimally invasive surgery that is able to overcome some of the limitations of laparoscopic techniques. Some of its benefits of RAS include (5):
- High-definition three-dimensional imaging of the endoscope view that increases depth perception and precision.
- Adjustments of the surgeon’s console that provide comfortable ergonomically advantageous positions.
- Elimination of motion reversal seen in laparoscopy.
- Increasing degrees of freedom (DOF) in instrument motion with the addition of a wrist-like joint at the end of the end-effector to better facilitate suturing and instrument tying.
- Favorable motion scaling by amplifying data or information to increase (or decrease) the distance the tip of an instrument moves relative to the distance the hand controller moves.
- Stable camera platform without tremor, rotation, or migration.
Until recently, there were few standardized curricula for RAS. The Fundamentals of Robotic Surgery (FRS) is a multi-specialty, proficiency-based curriculum of basic cognitive, psychomotor (technical), and team training and communication skills that was developed to train and assess surgeons to safely and efficiently perform robotic-assisted surgery (6,7). To establish this curriculum, a full-cycle development process was utilized to ensure the final curriculum and assessment methods would meet the rigorous requirements of determining proficiency, meeting standards, and possibly even fulfilling certification criteria.
To accomplish this goal, the FRS committee convened almost 80 robotic surgery experts, behavioral psychologists, medical educators, statisticians, and psychometricians. Represented in the clinical subject matter experts (SME) were all of the major surgical specialties in the United States that currently perform robotic-assisted surgical procedures, as well as the Department of Defense, and the VA. These leaders in robotic surgery participated in four consensus conferences that are briefly described below (6).
- Outcomes Measures: A prioritized matrix of 25 basic robotic surgery skills, outcome measures and metrics was produced, which served as the core material for development and design of the FRS curriculum.
- Curriculum Planning: A previously published expert consensus-driven surgical curriculum template was critically reviewed and adopted for the development of the FRS curriculum (8). An outline for subsequent curriculum development was developed.
- Curriculum Development: The FRS curriculum was broken down into 4 parts, including Introduction to Robotic Surgery, Didactic Instructions, Psychomotor Skills, and Team Training and Communication Skills. Online modules were developed for each of these areas. In addition, physical models and virtual reality simulation models were developed to train and test psychomotor skills involving seven basic RAS tasks.
- Validation Study Design: The study design was formulated to conduct a formal validation of the didactic online FRS curriculum, psychomotor (technical) skills, and team training and communication skills components. Based on this study design, an international multi-institutional, noninferiority blinded, randomized control trial was conducted that demonstrated effectiveness of the FRS curriculum by demonstrating better performance of those trained using FRS compared with controls.
The Institute for Surgical Excellence (ISE), a 501(c) (3) public non-profit organization dedicated to improving surgical care and patient outcomes, conducted the FRS validation study. ISE also coordinated, facilitated and managed a subsequent Fundamentals of Thoracic Robotic Surgery Consensus Conference that will be described below.
Expert consensus conference
Based on the groundwork set by the original four FRS consensus conferences, all elements of outcome measures and metrics, curriculum design and early development, simulation design, and team training and communication were all accomplished during a single Fundamentals of Thoracic Robotic Surgery (FTRS) Consensus Conference from February 9–11, 2017.
The goals for the meeting were to:
- Discuss best practices in curriculum development.
- Build upon the accomplishments of FRS and incorporate the experiences of thoracic societies and academic institutions to establish a standardized Thoracic Surgery robotic curriculum for the development and maintenance of specialty-specific robotic surgical skills.
- Develop a detailed outline for the FTRS training curriculum.
- Design thoracic surgery specific robotic psychomotor skills for the bedside assistant and console surgeon.
- Determine the most appropriate validation process for the curriculum.
During the meeting descriptions from existing thoracic robotic surgery curricula developed by individual institutions including Emory Healthcare, University of Michigan Health System, University of North Carolina and University of Pittsburgh Medical Center were presented. An update was also provided regarding a European thoracic surgery committee that was tasked with development of a robotic curriculum. Commonalities and differences between the various curricula were recorded and discussed.
Next, a task deconstruction was completed for the thoracic ‘signature’ procedure, the lobectomy, which included:
- Takedown of inferior pulmonary ligament, division of pleura.
- Dissect subcarinal posterior/paratracheal/hilar nodes.
- Dissect/divide superior vein.
- Dissect superior hilar/peribronchial nodes.
- Dissect/divide pulmonary arteries.
- Dissect/divide bronchus.
- Complete posterior/horizontal fissure.
- Management of PA Injury.
For each of these steps, training items and potential errors were identified and are provided in the Table 1.
Table 1
| Procedural step | Training items | Potential errors |
|---|---|---|
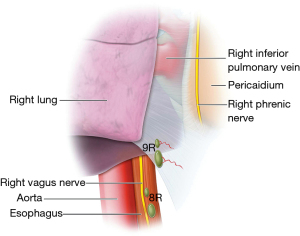
| Takedown of inferior pulmonary ligament, division of pleura | Identification of station 8/9 lymph nodes, energy device use, hemostasis, lung retraction | Injury to esophagus, Inferior vein, vagus, lung, bronchus intermedius, no-touch tumor |
| Dissect subcarinal posterior/paratracheal/hilar nodes | Correct identification of mediastinal nodal stations, en bloc dissection, avoidance of grabbing node (fracture), energy device use, hemostasis, lung retraction | Injury to vagus, R recurrent laryngeal nerves, lung, esophagus, airway, azygos, pulmonary artery, SVC, aorta |
| Dissect/divide superior vein | Vascular dissection (grabbing vein allowed), energy, stapler use | RML vein, phrenic, PA |
| Dissect superior hilar/peribronchial nodes | Node grabbing technique, en bloc dissection, energy, retraction (on vessels, bronchus) | Pulmonary artery, bronchus |
| Dissect/divide pulmonary arteries | Multiple vessels, vascular dissection (no-grab), energy, stapler use, clip use, energy division of artery and appropriate selection | Pulmonary artery, azygos |
| Dissect/divide bronchus | Energy, retraction, stapler use, recognition of correct structures | RUL bronchus, RMB, azygos, PA |
| Complete posterior/horizontal fissure | Stapler use, retraction, visualization of divided hilum | Phrenic nerve, bronchus intermedius, RML artery, lung parenchyma |
| Management of PA injury | Tamponade (lung, sponge, time dependent), retraction of camera, decision to convert, request additional staff, communication, blood request | Grabbing vessel, delay |
The consensus conference participants were then divided into two breakout groups responsible for developing the didactic online curriculum and the psychomotor skills curriculum, respectively. The output of the breakout groups included the outline of five modules to teach all components of a lobectomy procedure from the perspective of the pre-procedure patient assessment and preparation, the bedside assistant, the console surgeon, and the operating room team.
Curriculum development
Curriculum outline
The final outline of the FTRS curriculum derived from this process is provided below.
Module 1: introduction
- Learning Objectives.
- Brief Review of Advantages of Robotic Surgery.
- Fundamentals of Thoracic Robotic Surgery (FTRS) Consensus Conference.
Module 2: pre-procedure patient assessment and preparation for lobectomy
- Learning Objectives.
- Pre-Procedure Patient Assessment and Preparation.
- Review of Indications/Contraindications Robotic-Assisted Lobectomy.
- Pre-operative Assessment for Robotic-Assisted Lobectomy.
- Environment Considerations (Functioning Equipment, Instruments, Suture/Stapling Devices, etc.).
- Module 2 Assessment.
Module 3: bedside assistant
- Learning Objectives.
- Patient Positioning.
- General Description.
- Lateral Decubitus Position.
- Padding and Securing the Patient.
- Platform Specific Positioning Considerations.
- Port Placement/Trocar Placement.
- General Description.
- Platform Specific Port/Trocar Placement.
- Camera Management.
- Camera Insertion.
- Camera Removal.
- Platform Specific Camera Management.
- Insertion of Instruments.
- General Description.
- Potential Problems When Inserting Instrument.
- Platform Specific Instrument Insertion.
- Instrument Exchange.
- General Description.
- Stapling.
- General Description.
- Staple Height, Length, and Design.
- Stapler Manipulation.
- Platform Specific Stapling.
- Specimen Removal (Nodes, Lobe).
- General Description.
- Platform Specific Specimen Removal.
- Exposure.
- General Description.
- Suctioning.
- General Description.
- Platform Specific Suctioning.
- Standard Undocking.
- General Description.
- Platform Specific Standard Undocking.
- Emergency Undocking.
- General Description.
- Platform Specific Emergency Undocking.
- Postoperative Checklist.
- General Description.
- Platform Specific Postoperative Checklist.
- Summative Assessment.
- Dry Lab Skills Assessment (with Mannequin and Robot).
- Bedside Assistant Certificate.
Module 4: console surgeon
- Learning Objectives.
- Overview.
- Takedown of Inferior Pulmonary Ligament, Division of Posterior Pleura.
- Anatomy Review.
- Description.
- Instruments Used.
- Video Examples.
- Potential Errors and Complications.
- Dissect Subcarinal Posterior/Paratracheal/Hilar Nodes.
- Anatomy Review.
- Description.
- Instruments Used.
- Video Examples.
- Potential Errors and Complications.
- Dissect/Divide Superior Vein.
- Anatomy Review.
- Description.
- Instruments Used.
- Video Examples.
- Potential Errors and Complications.
- Dissect Superior Hilar/Peribronchial Nodes.
- Anatomy Review.
- Description.
- Instruments Used.
- Video Examples.
- Potential Errors and Complications.
- Dissect/Divide Pulmonary Arteries.
- Anatomy Review.
- Brief Description.
- Instruments Used.
- Video Examples.
- Potential Errors and Complications.
- Dissect/Divide Bronchus.
- Anatomy Review.
- Brief Description.
- Instruments Used.
- Video Examples.
- Potential Errors and Complications.
- Incomplete Posterior/Horizontal Fissure.
- Anatomy Review.
- Description.
- Instruments Used.
- Video Examples.
- Potential Errors and Complications.
- Management of Pulmonary Artery Injury.
- Description.
- Instruments Used.
- Video Examples.
- Potential errors and complications.
- Psychomotor Component (Description of Simulation).
- Lung Retraction.
- Dissection of the Pulmonary Artery.
- Stapling and Dividing the Pulmonary Artery.
- Dissection and Removal of Peribronchial Lymph Nodes.
- Managing Minor Bleeding.
- Video Review.
- Psychomotor Skills Assessment.
Module 5: team training
- Learning Objectives.
- Overview.
- TeamSTEPPS® Background.
- Communication.
- Overview.
- Requests.
- Call-Outs.
- Cross-Checks.
- Check-Backs.
- Situation Awareness.
- Overview.
- Pre-Brief.
- Huddle.
- Debrief.
- SBAR.
- Mutual Support.
- Overview.
- CUS.
- Two-Challenge Rule.
- Checklists.
- WHO Checklist.
- General Pre-operative Phase Checklist.
- Nurse and Operating Department Practitioner (ODP) Checklist.
- Bedside Assistant Related Checklist.
- Trouble Shooting Checklist.
- Leadership.
- Overview.
- Emergency Undocking.
- Principles and Differences from Standard Undocking.
- Deliberate Practice.
- Assessment.
- Cognitive-Questions.
- Robotic Thoracic Surgery Team.
- Team Training Scenarios.
- Pre-Brief Scenario.
- SBAR Scenario.
- CUS Scenario.
- Emergency Undocking.
- Debrief.
Psychomotor skills training
It was determined at the consensus conference that thoracic surgeons undergoing the FTRS curriculum must complete the online component before progressing to the hands-on psychomotor skills training. At the consensus conference physical thoracic surgery training models (animal tissue and 3D printed models) were discussed as well as virtual reality simulation models. Following the meeting, several thoracic robotic surgery experts have worked with a simulation company to make the VR lobectomy procedure more realistic and anatomically accurate. An example of the VR lobectomy simulation (developed by 3D Systems) is shown in Figure 1.

Multimedia development
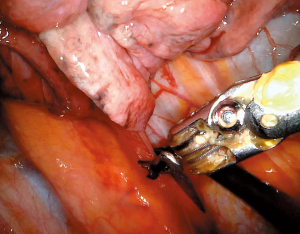
Following the consensus conference, new medical illustrations were developed by ISE and more than two dozen video examples from consensus conference participants to support the curriculum. Some examples are shown (Figures 2-5).


Post-conference action plan
In addition, a post-conference action plan was initiated and successfully completed including:
- Disseminating the information about FTRS to participants’ respective organizations and societies to obtain input and “buy in”.
- Creating a steering committee comprised of Drs. Anthony Kim, Bernard Park, Allan Pickens and David Rice to finish the content development process for the curriculum.
- All participants reviewing and editing the final draft of the FTRS curriculum.
- Collaborating with European thoracic surgeons to coordinate international curriculum development efforts.
Conclusions
FRS is a proven curriculum development model that included consensus conferences on Outcomes Measures, Curriculum Planning, Curriculum Development, and Validation Study Design. This process led to a validated basic cross-specialty curriculum. The FTRS consensus conference followed this model but in an accelerated process due to important groundwork set by experts in the FRS consensus conferences. A full online curriculum and supporting psychomotor skills training and team communication has been developed for the lobectomy procedure. There are plans to duplicate this process for other important thoracic robotic surgical procedures including segmentectomy, esophagectomy, thymectomy, repair of hiatal hernias, Heller myotomy, selective dorsal sympathectomy and first rib resection.
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editor (Ghulam Abbas) for the series “Robotic Thoracic Surgery” published in Journal of Thoracic Disease. The article has undergone external peer review.
Conflicts of Interest: Both authors have completed the ICMJE uniform disclosure form (available at: http://dx.doi.org/10.21037/jtd-2019-rts-02). The series “Robotic Thoracic Surgery” was commissioned by the editorial office without any funding or sponsorship. Dr. Levy reports grants from Medtronic, during the conduct of the study. Dr. Gharagozloo reports grants from Medtronic, during the conduct of the study. Both authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Braga M, Vignali A, Gianotti L, et al. Laparoscopic versus open colorectal surgery: a randomized trial on short-term outcome. Ann Surg 2002;236:759-66; disscussion 767.
- Nieboer TE, Johnson N, Lethaby A, et al. Surgical approach to hysterectomy for benign gynaecological disease. Cochrane Database Syst Rev 2009;CD003677 [PubMed]
- Perino A, Cucinella G, Venezia R, et al. Total laparoscopic hysterectomy versus total abdominal hysterectomy: an assessment of the learning curve in a prospective randomized study. Hum Reprod 1999;14:2996-9. [Crossref] [PubMed]
- Chapron C, Fauconnier A, Goffinet F, et al. Laparoscopic surgery is not inherently dangerous for patients presenting with benign gynecologic pathology: results of a meta-analysis. Hum Reprod 2002;17:1334-42. [Crossref] [PubMed]
- Schreuder HWR, Verheijen RHM. Robotic surgery. BJOG 2009;116:198-213. [Crossref] [PubMed]
- Satava RM, Stefanidis D, Levy JS, et al. Proving the Effectiveness of the Fundamentals of Robotic Surgery (FRS) Skills Curriculum: A Single-blinded, Multispecialty, Multi-institutional Randomized Control Trial. Ann Surg 2020;272:384-92. [Crossref] [PubMed]
- Gallagher AG. Metric-based simulation training to proficiency in medical education:- what it is and how to do it. Ulster Med J 2012;81:107-13. [PubMed]
- Zevin B, Levy JS, Satava RM, et al. A Consensus-Based Framework for Design, Validation, and Implementation of Simulation-Based Training Curricula in Surgery. J Am Coll Surg 2012;215:580-6. [Crossref] [PubMed]


