
Prevalence of comorbidities in a surgical pectus excavatum population
Introduction
Pectus excavatum is the most common congenital chest wall deformity, predominantly affecting males (1). The aetiology of pectus excavatum is unknown, although familial and genetic predisposition have been observed (2,3). Patients with pectus excavatum have lower exercise capacity compared to healthy controls, although normalizing after surgical correction (4). The presence of cardiac anomalies, mainly affecting the mitral and tricuspid valves, have been found in up to one-third of patients referred for pectus excavatum correction (5). Furthermore, various conditions and syndromes have been described to be associated with pectus excavatum, e.g., connective tissue syndromes as Marfan, Ehlers-Danlos, and Poland syndromes (6). Two-thirds of patients diagnosed with Marfan syndrome have concomitant pectus excavatum while Marfan syndrome is found in 5% of patients with pectus excavatum referred for surgery (5). Moreover, conditions such as obstructive sleep apnoea and pulmonary blebs are found to be highly prevalent in pectus excavatum patients (7,8). In addition, pectus excavatum is found more frequently in patients with congenital diaphragm herniation (9).
The majority of the studies in this field are based on small study populations and are limited to investigating the association between pectus excavatum and various confined topics. Despite a multitude of syndromes and conditions being linked to pectus excavatum, it is unclear whether the pectus excavatum phenotype is notably associated to other conditions. Furthermore, the comorbidity burden of patients with this common chest wall deformity is unknown, and no studies have investigated the prevalence of all comorbidities in this patient category. Thus, the aim of this study was to examine the pectus excavatum phenotype by assessing the prevalence of comorbidities and previous medical conditions in patients undergoing correction of pectus excavatum.
We present the following article in accordance with the STROBE reporting checklist (available at http://dx.doi.org/10.21037/jtd-20-3352).
Methods
Study population and data collection
Between 2001 to 2012, 1,046 patients diagnosed with moderate to severe pectus excavatum based on clinical examination underwent surgical correction at our center with the modified Nuss procedure ad modum Pilegaard (10). Patients were identified and included if registered under the procedure code for correction of pectus excavatum (n=1,047). Exclusion criteria was missing medical records (n=1). Hospital medical records were retrospectively assessed between 2018 to 2019 and information was registered on gender, date of birth, date of operation, past medical history requiring hospitalization or known comorbidities registered at the time of surgery. Furthermore, comorbidities and past medical conditions were categorized separately if a solitary condition was notably prevalent or otherwise clustered according to the affected organ system in the following categories: gastric, urologic, neurologic, psychiatric, cardiac, ear-nose-throat, and other.
Ethical statement
The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by the head of the Department of Cardiothoracic and Vascular Surgery, Aarhus University Hospital, and individual consent for this retrospective analysis was waived.
Statistical analysis
All data were registered in REDCap (11) (Research Electronic Data Capture, REDCap Consortium, Vanderbilt University Medical Center, Tennessee, USA), and statistical analyses were performed in Stata (Version 15.1, Lakeway dr, TX. StataCORP). Differences between prevalence of comorbidities across gender groups were assessed with Fishers exact test or Chi2 test, as appropriate. Two-sided P values <0.05 were considered statistically significant.
Results
Characteristics of the study population and gender differences
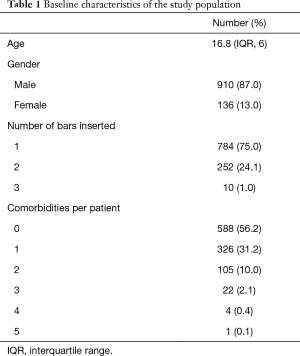
A total of 623 comorbidities and past medical conditions were found in 1,046 patients. Table 1 shows the baseline characteristics of the study population as well as the number of comorbidities per patient. The median age was 16.8 years and the male to female ratio was 5:1. The majority of the population had no comorbidities (56.2%), although nearly one third (31.2%) of the patients had one comorbidity and one of eight patients (12.6%) had more than one comorbidity (Figure 1).
Full table
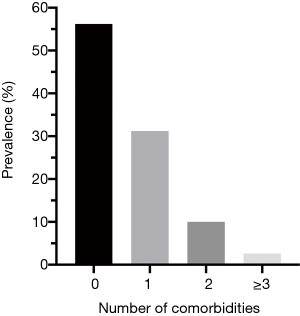
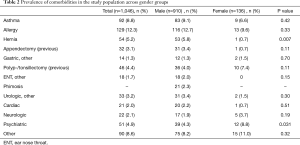
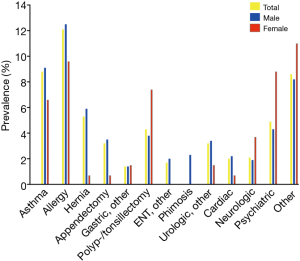
Table 2 shows the comorbidity categories across gender groups. Notable prevalence of allergies (12.3%), asthma (8.8%), hernias (5.2%), psychiatric conditions (4.9%), and previous polyp-/tonsillectomies (4.4%) were found in the population (Figure 2). Prevalence of hernias (males 5.8% vs. female 0.7%, P=0.007) and psychiatric conditions (males 4.3% vs. females 8.8%, P=0.031) were found to be different across genders with a statistical significance.
Full table
Hernias and GI-tract conditions
A total of 54 patients had a history of surgical hernia repair—predominantly inguinal hernias (27 patients) followed by umbilical hernias (8 patients) and diaphragmatic hernia (1 patient). The remaining hernia types was not specified in the medical charts (18 patients). A total of 46 gastrointestinal conditions were registered with majority of patients having a history of previous appendectomy (32 patients), followed by inflammatory bowel disease (6 patients) and pyloric stenosis (3 patients).
Cardiac conditions
Five patients had paroxysmal supraventricular tachycardia of which three had atrial fibrillation and one patient with Wolf-Parkinsons-White syndrome. Four patients had history of ventricular septum defects while one patient had atrial septum defect. Furthermore, four patients had aortic root dilatation with three patients requiring surgery [all three underwent single stage correction of pectus excavatum and cardiac anomalies as previously reported (12)], and two patients had aortic coarctation.
Phimosis and other urologic conditions
The urologic conditions were dominated by phimosis (21 patients), followed by cryptorchism (6 patients), torsio testis (4 patients), pyelonephritis (5 patients), testicular cancer (3 patients), hydrocele (3 patients), urethral stricture (4 patients), and haematuria (3 patients).
Neurologic conditions
The 22 patients with neurologic conditions were mainly due to migraine (15 patients), followed by epilepsy (2 patients), meningitis (2 patients), intracranial aneurysm (1 patient), intracranial tumour (1 patient), and hydrocephalus (1 patient).
Psychiatric conditions
Of 51 patients registered with history of psychiatric conditions, 23 patients had a history of depression and 14 patients had attention-deficit/hyperactivity disorder.
Other not classified conditions
Various conditions could not be classified in the above-mentioned categories (90 patients). Some of these patients had a history of scoliosis (9 patients), morbus Scheuerman (6 patients), Marfan syndrome (4 patients), muscular dystrophias (3 patients), Ehlers Danlohs syndrome (2 patients), and medically treated acne vulgaris (10 patients).
Discussion
This study found a high prevalence of comorbidities and previous medical conditions (44%) amongst patients undergoing surgical correction of pectus excavatum. Notable prevalence of asthma, allergies, hernias, psychiatric conditions and previous polyp-/tonsillectomies were found. Furthermore, hernias were observed predominantly in males while females had a higher prevalence of psychiatric comorbidity.
We found a relatively high prevalence of previous surgery for hernias (5.2%) in this study population. One theory for the aetiology of hernias is alternations of the connective tissue (13). Both collagen subtypes, tissue architecture and connective tissue homeostasis are found to be different in patients with hernias compared to controls (13). The association between pectus excavatum and connective tissue diseases as Marfan and Ehlers Danlohs syndromes is well established (6). The presence of pectus excavatum requiring surgery is included in the diagnostic criteria in Marfan syndrome with the Ghent Nosology (14). As for hernias, several abnormalities in the connective tissue are found in the aforementioned connective tissue syndromes (13). Despite these considerations, one cross-sectional study found, very similar to our study population, a cumulated incidence of inguinal hernias from birth to 15 years of age in 7.4% of the study population (15). Only 4 patients in our study population were diagnosed with Marfan syndrome (0.4%). Other studies have shown prevalence of Marfan syndrome ranging from 0.5% to 5.3% in surgical pectus excavatum populations (5). Moreover, Behr et al. found presence of cardiac abnormalities in one third of patients undergoing pectus excavatum surgery (5). In contrast, only 2% of patients had a history of cardiac conditions in our study population. However, comparisons of prevalence across study populations are of limited value in this context due to the obvious risk of selection biases.
Both asthma (8.8%) and allergies (12.3%) were found remarkably prevalent in this study. A Nordic register based cross-sectional study found comparable prevalence of asthma (12%), atopic dermatitis (13%), and allergic rhinoconjunctivitis (7%) in danish children (16). As these conditions peak in childhood and adolescence, the high prevalence of these conditions in our study population are more likely to be due to the age distribution rather than the presence of pectus excavatum.
In our study population, 4.9% of the patients had a history of psychiatric diagnosis. Previous studies have shown quality of life and self-image improvements after surgical correction of pectus excavatum (17,18). Also, patients with pectus excavatum have lower health-related quality of life prior to surgery compared to controls (17). In spite of this, patients with pectus excavatum do not appear to be more burdened with mental health conditions compared to controls; Steinmann et al. found a prevalence of 17% for any previous mental disorders in males undergoing surgery for pectus excavatum, and this was not different from a control group (18).
The strength of this study is the systematic assessment of comorbidities in a large single-center study population. The retrospective study design and lack of a control group limit the scientific value of the findings. No control group could be sampled based on hospital medical records for comparison, as information would only be accessible for hospitalized patients at the time of hospitalization. This would underestimate prevalence of comorbidities in the control group and imply major risk of bias. Therefore, it is not possible to thoroughly discern differences in the comorbidity burden in pectus excavatum patients compared to the background population. Further studies are required to fully comprehend the health-related implications of the pectus excavatum phenotype.
Conclusions
In patients undergoing minimal invasive repair of pectus excavatum, the majority of patients had no comorbidities or previous conditions. However, notable prevalence of asthma, allergies, previous hernia surgery, and psychiatric comorbidity were found. When comparing our findings to previous studies, the comorbidity burden in patients with pectus excavatum requiring surgery seems be comparable to the background population. Thus, our findings do not support screening this patient category for associated conditions.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at http://dx.doi.org/10.21037/jtd-20-3352
Peer Review File: Available at http://dx.doi.org/10.21037/jtd-20-3352
Data Sharing Statement: Available at http://dx.doi.org/10.21037/jtd-20-3352
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/jtd-20-3352). Dr. TDC reports personal fees from AstraZeneca, Boehringer-Ingelheim, Roche Diagnostics, Merck Sharp & Dohme (MSD, and Bristol Myers Squibb, all outside the submitted work. The other authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by the head of the Department of Cardiothoracic and Vascular Surgery, Aarhus University Hospital, and individual consent for this retrospective analysis was waived.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Kelly RE, Lawson ML, Paidas CN, et al. Pectus excavatum in a 112-year autopsy series: Anatomic findings and the effect on survival. J Pediatr Surg 2005;40:1275-8. [Crossref] [PubMed]
- Kotzot D, Schwabegger AH. Etiology of chest wall deformities-a genetic review for the treating physician. J Pediatr Surg 2009;44:2004-11. [Crossref] [PubMed]
- Creswick HA, Stacey MW, Kelly RE, et al. Family study of the inheritance of pectus excavatum. J Pediatr Surg 2006;41:1699-703. [Crossref] [PubMed]
- Maagaard M, Tang M, Ringgaard S, et al. Normalized cardiopulmonary exercise function in patients with pectus excavatum three years after operation. Ann Thorac Surg 2013;96:272-8. [Crossref] [PubMed]
- Behr CA, Denning NL, Kallis MP, et al. The incidence of Marfan syndrome and cardiac anomalies in patients presenting with pectus deformities. J Pediatr Surg 2019;54:1926-8. [Crossref] [PubMed]
- Tocchioni F, Ghionzoli M, Messineo A, et al. Pectus excavatum and heritable disorders of the connective tissue. Pediatr Rep 2013;5:e15 [Crossref] [PubMed]
- Schaerer D, Virbalas J, Willis E, et al. Pectus excavatum in children with laryngomalacia. Int J Pediatr Otorhinolaryngol 2013;77:1721-3. Erratum in Int J Pediatr Otorhinolaryngol 2015;79:1963. [Crossref] [PubMed]
- Huang HK, Huang YJ, Lin KH, et al. Severity of Pectus Excavatum is a Risk Factor for Primary Spontaneous Pneumothorax. World J Surg 2020;44:2035-41. [Crossref] [PubMed]
- Aydın E, Özler O, Burns P, et al. Left congenital diaphragmatic hernia-associated musculoskeletal deformities. Pediatr Surg Int 2019;35:1265-70. [Crossref] [PubMed]
- Hoffmann T, Vad H, de Paoli F. Correction of pectus excavatum using the modified Nuss procedure, ad modum Pilegaard. Multimed Man Cardiothorac Surg 2018;2018: [Crossref] [PubMed]
- Harris PA, Taylor R, Thielke R, et al. Research electronic data capture (REDCap)-A metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform 2009;42:377-81. [Crossref] [PubMed]
- Media AS, Pilegaard HK, de Paoli FV. Combining Correction of Pectus Excavatum and Open Heart Surgery in a Single-Stage Procedure. Ann Thorac Surg 2020;109:e71-4. [Crossref] [PubMed]
- Harrison B, Sanniec K, Janis JE. Collagenopathies—Implications for abdominal wall reconstruction: A systematic review. Plast Reconstr Surg Glob Open 2016;4:e1036 [Crossref] [PubMed]
- Loeys BL, Dietz HC, Braverman AC, et al. The revised Ghent nosology for the Marfan syndrome. J Med Genet 2010;47:476-85. [Crossref] [PubMed]
- Chang SJ, Chen JYC, Hsu CK, et al. The incidence of inguinal hernia and associated risk factors of incarceration in pediatric inguinal hernia: a nation-wide longitudinal population-based study. Hernia 2016;20:559-63. [Crossref] [PubMed]
- Henriksen L, Simonsen J, Haerskjold A, et al. Incidence rates of atopic dermatitis, asthma, and allergic rhinoconjunctivitis in Danish and Swedish children. J Allergy Clin Immunol 2015;136:360-366.e2. [Crossref] [PubMed]
- Lomholt JJ, Jacobsen EB, Thastum M, et al. A prospective study on quality of life in youths after pectus excavatum correction. Ann Cardiothorac Surg 2016;5:456-65. [Crossref] [PubMed]
- Steinmann C, Krille S, Mueller A, et al. Pectus excavatum and pectus carinatum patients suffer from lower quality of life and impaired body image: A control group comparison of psychological characteristics prior to surgical correction. Eur J Cardiothorac Surg 2011;40:1138-45. [Crossref] [PubMed]


