Boerhaave’s syndrome and tension pneumothorax secondary to Norovirus induced forceful emesis
Introduction
Boerhaave’s syndrome, also known as spontaneous esophageal perforation was first described in 1724 by Hermann Boerhaave (1). The perforation is mostly on the left inferior part of the esophagus and is very often associated with forceful vomiting leading to a rapid rise in the intraluminal pressure in the distal esophagus, causing the perforation (2). Mortality rates are 20-40% in treated and nearly 100% in untreated cases (3,4).
The incidence is low - in Denmark (5,300,000 inhabitants) 89 cases have been reported in the period from 1997-2005 (5). The approach for treatment is still controversial, but can be endoscopic, surgical or conservative (3). We describe a case of Boerhaave’s syndrome triggered by Norovirus that was acutely complicated with tension pneumothorax, in an otherwise healthy person.
Case report
A 67-year-old previously healthy man without any co-morbidity was admitted to the Emergency Department (ED) with excessive vomiting, diarrhoea and severe epigastric pain. The patient described that after the third time he vomited, he started having trouble breathing which gradually improved. The day before he had been eaten raspberries along with several other people, who also developed vomiting and diarrhoea. At the admission his symptoms were interpreted as a simple gastroenteritis and no further investigations were done and he was discharged. Four days later he was re-admitted to the ED in respiratory distress with respiratory rate 32 per minute, oxygen saturation 82% with O2 15 L/min, rectal temperature 38.0 °C (100.4 F), blood pressure 139/82 mmHg, pulse 108 beats per minute and blood analysis demonstrated leukocytes 20.1×109 /L (reference 3-10) and C-reactive protein 409 mg/L (reference less than 10). 12 Lead EKG demonstrated sinus tachycardia but otherwise normal. His main complaint was still severe epigastric pain.
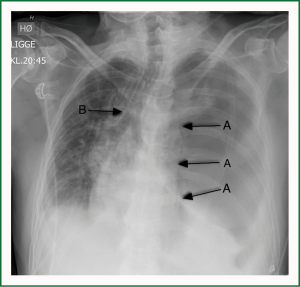
The patient’s critical clinical presentation provided a chest X-ray at the primary survey, which demonstrated tension pneumothorax with mediastinal shift to the right and with pleural effusion (Figure 1).
He was acutely decompressed with a 17 G peripheral venous cannula in the left second intercostal space in the mid-clavicular line which led to marked improvement and immediately followed after a 24 Fr chest tube in the left fifth intercostal space in the mid-axillary line, which drained of 1.5 litre of white fluid within 5 minutes. He responded promptly with normalized respiration on O2 2 L/min supply, and was clinically stable.
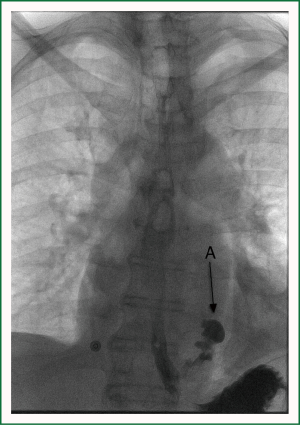
Esophagogram demonstrated contrast extravasation from oesophagus on the inferior left side (Figure 2). He underwent acute thoracotomy and perioperative findings confirmed a 4 cm rupture in the lower part of oesophagus, gastric content in the thoracic cavity and emphyema. The rupture was treated with primary suture, decortication of the lung, drainage with two chest tubes and a feeding jejunostomy. At the admission a stool test was found positive for Norovirus, which accomplished an investigation through the Danish Veterinary and Food Administration and a withdrawal of a shipment of frozen raspberries from Serbia.
Postoperative course was complicated with acute respiratory distress syndrome and sepsis, which was treated with intravenous antibiotics (cefuroxime and metronizadole) and mechanical ventilation. The course was further complicated with three times of contrast extravasation from the repaired area at 21, 46 and 50th postoperative day which were all confirmed with esophagogram. Every leakage was treated endoscopically with an esophageal stent, but due to the distally location of the rupture the covered esophageal stent extending into the stomach and apparently causing retrograde leakage of gastric content on the outside of the stent which delayed healing.
The patient gradually recovered and started normal diet before discharge from the hospital after 98 days. The oesophageal stent was removed 2 weeks after discharge and the patient was last seen in the out patient clinic after further 14 days where he was in good health.
Discussion
The clinical presentation of Boerhaave’s syndrome is described as vomiting, chest pain, dyspnoa, mediastinal or subcucataneous emphysema and cardiovascular collapse (2). X-ray findings are pleural effusion and pneumothorax (2).
X-ray of esophagus with contrast is the first choice to achieve the definitive diagnosis with a false negative rate of 10-25% while chest CT with oral contrast is the second choice (2,6,7). In the literature there are three strategies of treatment: (I) endoscopic, (II) open surgery and (III) conservative approach. This is still being discussed, but in a recent review de Schipper JP et al. conclude that endoscopic treatment is recommended when the patient is diagnosed within 48 hours and without sepsis. If the patient is diagnosed within 48 hours and has a septic profile thoracotomy with suture of the rupture and mediastinal/pleural drainage is the treatment of choice.
For a patient diagnosed after 48 hours, conservative treatment is recommended, and surgical treatment reserved for a patient with a septic profile (3). Others recommend an aggressive treatment of sepsis and radiological guided drainage of the leakage which in most cases avoids major surgery and allows esophageal healing with reduced mortality and morbidity (8). A new study with a relatively small number of patients compared Video Assisted Thoracoscopic Surgery (VATS) with open surgery which concluded that VATS is not inferior to open surgery (thoracotomy) (9).
We followed the recommendations from de Schipper et al. for a late diagnosed esophageal rupture in a septic patient (3).
Pneumothorax develops from a lesion in the visceral or parital pleura and may evolve into a tension pneumothorax if the pleural defect functions as a one-way valve with air trapping during inspiration leading to increased ipsilateral intrapleural pressure (10).
A combination of Boerhaave’s syndrome and tension pneumothorax has only been described a few times in literature (11).
At the first examination our patient’s symptoms were mistaken as gastroenteritis, which is common because the signs in Boerhaave’s syndrome are often weak and symptoms such as epigastric pain often obscure the clinical picture and delay definitive diagnosis and treatment (2,6). The most common differential diagnoses are perforated ulcer, myocardial infarction, pulmonary embolism, aortic dissection and pancreatitis (2,3).
At the second referral the patient had gastroenteritis (Norovirus infection), mediastinitis, tension pneumothorax, and esophageal perforation.
We speculate that the clinical picture developed because of the infection with Norovirus which accomplished forceful vomiting, that resulted in an increase in the intraesophageal pressure and a rotation of the esophagus that teared the muscle layer proximally to the esophageal mucosa which possibly lead to formation of a “pseudo” one-way valve with trapping of fluid and air in the pleural cavity. The increase in intrapleural pressure caused a mediastinal shift and progressive respiratory deterioration of a patient with progressive developing emphyema and mediastinitis and without decompression with a venous cannula and chest tube it could have ended fatal.
In conclusion, we describe the first case of Boerhaave’s syndrome triggered by Norovirus and acutely complicated with tension pneumothorax, in an otherwise healthy person.
Our case demonstrates that a harmless virus infection under certain circumstances can cause a rare and often misdiagnosed syndrome (Boerhaave’s), which can progress to a lethal stage. Boerhaave’s syndrome has high mortality and is worth keeping in mind when a patient has signs of respiratory distress with a history of vomiting, although the classical signs are often absent.
Acknowledgements
Disclosure : The authors declare no conflict of interest.
References
- Boerhaave H. Atrocis, nec descripti prius, morbi historia. Secundum medicae artis leges conscripta. Lugduni Batavorum: Ex Officina Boutesteniana 1724.
- Janjua KJ. Boerhaave’s syndrome. Postgrad Med J 1997;73:265-70.
- de Schipper JP, Pull ter Gunne AF, Oostvogel HJ, et al. Spontaneous rupture of the oesophagus: Boerhaave’s syndrome in 2008. Literature review and treatment algorithm. Dig Surg 2009;26:1-6.
- Curci JJ, Horman MJ. Boerhaave’s syndrome: The importance of early diagnosis and treatment. Ann Surg 1976;183:401-8.
- Ryom P, Ravn JB, Penninga L, et al. Aetiology, treatment and mortality after oesophageal perforation in Denmark. Dan Med Bull 2011;58:A4267.
- Lemke T, Jagminas L. Spontaneous esophageal rupture: a frequently missed diagnosis. Am Surg 1999;65:449-52.
- Backer CL, LoCicero J 3rd, Hartz RS, et al. Computed tomography in patients with esophageal perforation. Chest 1990;98:1078-80.
- Vogel SB, Rout WR, Martin TD, et al. Esophageal perforation in adults: aggressive, conservative treatment lowers morbidity and mortality. Ann Surg 2005;241:1016-21; discussion 1021-3.
- Haveman JW, Nieuwenhuijs VB, Kobold JP, et al. Adequate debridement and drainage of the mediastinum using open thoracotomy or video-assisted thoracoscopic surgery for Boerhaave’s syndrome. Surg Endosc 2011;25:2492-7.
- Leigh-Smith S, Harris T. Tension pneumothorax--time for a re-think? Emerg Med J 2005;22:8-16.
- Onyeka WO, Booth SJ. Boerhaave’s syndrome presenting as tension pneumothorax. J Accid Emerg Med 1999;16:235-6.


