High-flow oxygen cannula: a very effective method to correct severe hypoxemia
Nasal high-flow (NHF) oxygen administration through a cannula is a simple and very effective way to correct severe hypoxemia. Initially developed in neonatal units, the system has been more recently adapted for use in adults. Several systems are now available, delivering warm, humidified oxygen at flows of up to 60 L/min. In addition to low costs and ease of application, NHF has several distinct features. First, the high flow rates can flush expired CO2 from the upper airways and reduce dead space. Second, it creates a small continuous positive airway pressure (CPAP), typically of 2-4 cmH2O. Third, the high flow, which exceeds the peak inspiratory flow of the patient, can limit the entrainment of room air during inspiration, and can thus provide a more stable oxygen concentration in the inspired gases. Fourth, the heated, humidified oxygen administered at high flow rates may help to prevent the stagnation of secretions and the formation of atelectasis. These features contribute to make the system particularly well-tolerated by patients with severe respiratory failure. Maggiore et al. (1) recently showed that use of NHF after extubation resulted in better oxygenation than with Venturi mask oxygen therapy for the same set FiO2, and was associated with better patient comfort, fewer desaturations and interface displacements, and a lower reintubation rate.
Non-invasive ventilation (NIV) is clearly a different concept. NIV can increase end-expiratory lung volumes, decrease the work of breathing, and also improve gas exchange. On the other hand, with its interfaced equipment, NIV may increase dead space. Despite some encouraging observations (2), CPAP with or without NIV may be hazardous in the management of the acute respiratory distress syndrome (ARDS) (3). In a multicenter cohort study, Antonelli et al. (4) reported that the use of NIV as first-line therapy for ARDS was followed by endotracheal intubation in close to 50% of cases, especially in the most severe cases or when gas exchange did not improve after 1 h. Hence, NIV may be tried in less severe cases, especially in expert hands, but should not be used for long if there is no clear clinical response. NIV may be better used in the presence of severe hypoxemia due to cardiogenic lung edema (4,5), because of the beneficial cardiac effects of the increase in intrathoracic pressure decreasing left ventricular afterload.
In a recent multicenter study, Frat et al. (6) demonstrated the value of NHF in 313 patients with severe hypoxemia: 3/4 of the total population had bilateral chest infiltrates and about 2/3 had community-acquired pneumonia. Patients were randomized into three groups: treatment with NHF, with regular oxygen therapy by face mask, or with NIV (at least 8 h a day for at least 2 days). Although the differences were not statistically significant, the 28-day intubation rate (the primary outcome) was 38% in the NHF group versus 47% in the standard oxygen group and 50% in the NIV group. Interestingly, the mortality rate was significantly lower with NHF than in the two other groups, and remained so after adjustment for severity. Were these differences in mortality due only to chance? It is hard to say, as the study was limited to about 100 patients per group and was, not-surprisingly, unblinded. The mortality rates were recorded over a 90-day period, but the differences were already present after 14 days. The study clearly highlights the potential role of NHF in patients with severe hypoxemia, and supports previous observations. It also stresses the very limited place for NIV, if any, in the management of severe hypoxemia, as NIV had no benefits over simple oxygen administration. In a slightly different setting of postoperative care, a recent study by Stéphan et al. (7) indicated that NHF was as effective as NIV (applied by bilevel positive airway pressure) in the prevention of respiratory failure in 830 patients after cardiothoracic surgery.
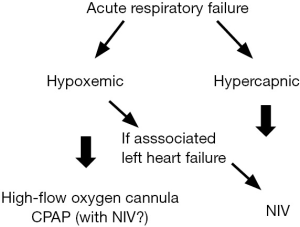
NHF is becoming the preferred option for the management of severe hypoxemic respiratory failure, and is superior to NIV in this condition. In contrast, NIV remains well established in the management of hypercapnic respiratory failure, since the landmark study by Brochard et al. 20 years ago showing that NIV was associated with reduced need for endotracheal intubation, length of hospital stay, and in-hospital mortality in patients with acute exacerbations of chronic obstructive pulmonary disease (8). NIV should be used cautiously in purely hypoxemic respiratory failure, unless there is associated left heart failure. The management of these different entities is, therefore, clearly different, as illustrated in Figure 1.
Acknowledgements
None.
Footnote
Provenance: This is a Guest Editorial commissioned by the Guest-Editor Ming Zhong (Department of Critical Care Medicine of Zhongshan Hospital, Fudan University, Shanghai, China).
Conflicts of Interest: The author has no conflicts of interest to declare.
References
- Maggiore SM, Idone FA, Vaschetto R, et al. Nasal high-flow versus Venturi mask oxygen therapy after extubation. Effects on oxygenation, comfort, and clinical outcome. Am J Respir Crit Care Med 2014;190:282-8. [PubMed]
- Ferrer M, Esquinas A, Leon M, et al. Noninvasive ventilation in severe hypoxemic respiratory failure: a randomized clinical trial. Am J Respir Crit Care Med 2003;168:1438-44. [PubMed]
- Delclaux C, L’Her E, Alberti C, et al. Treatment of acute hypoxemic nonhypercapnic respiratory insufficiency with continuous positive airway pressure delivered by a face mask: A randomized controlled trial. JAMA 2000;284:2352-60. [PubMed]
- Antonelli M, Conti G, Esquinas A, et al. A multiple-center survey on the use in clinical practice of noninvasive ventilation as a first-line intervention for acute respiratory distress syndrome. Crit Care Med 2007;35:18-25. [PubMed]
- Masip J, Roque M, Sánchez B, et al. Noninvasive ventilation in acute cardiogenic pulmonary edema: systematic review and meta-analysis. JAMA 2005;294:3124-30. [PubMed]
- Frat JP, Thille AW, Mercat A, et al. High-flow oxygen through nasal cannula in acute hypoxemic respiratory failure. N Engl J Med 2015;372:2185-96. [PubMed]
- Stéphan F, Barrucand B, Petit P, et al. High-Flow Nasal Oxygen vs Noninvasive Positive Airway Pressure in Hypoxemic Patients After Cardiothoracic Surgery: A Randomized Clinical Trial. JAMA 2015;313:2331-9. [PubMed]
- Brochard L, Mancebo J, Wysocki M, et al. Noninvasive ventilation for acute exacerbations of chronic obstructive pulmonary disease. N Engl J Med 1995;333:817-22. [PubMed]


