Lung cancer screening using low dose CT: screening population and positive results definition
Lung cancer is the leading cause of cancer-related death worldwide. The morbidity and mortality increase steadily in the near future. The 5-year survival rate of IA, IB, IIA, IIB, IIIA, IIIB and IV stage lung cancer decreased with the progression of disease, which was 50%, 43%, 36%, 25%, 19%, 7% and 2%, respectively (1). Therefore, early detection, early diagnosis and early therapy play great roles in decreasing the mortality and improving the life quality of patients. Among the current imaging modalities, CT is the most effective technique for lung cancer screening due to high detection rate and detailed anatomic structures. Sone and his colleagues reported the mass screening for lung cancer using mobile spiral CT in 1998, which was the first mass screening (5,483 participants) using CT (2). In the following about 20 years, many screening programs were performed, such as National Lung Screening Trial (NLST), International Early Lung Cancer Action Project (I-ELCAP), Nederlands-Leuvens Longkanker Screenings Onderzoek (NELSON) and Italian Lung (ITALUNG) (3-6).
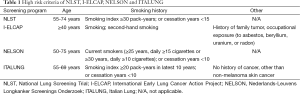
With great interest we read the article by Yi et al. (7) entitled ‘Low-dose CT screening in an Asian population with diverse risk for lung cancer: A retrospective cohort study’, which was published on European Radiology 2015;25:2335-45. They retrospectively compared the low dose CT (LDCT) and chest radiology (CXR) on the detection of early stage lung cancer in 12,427 symptomless Asian subjects and found LDCT can help detect more early-staged lung cancers in an Asian non-high-risk group and majority of these early-staged lung cancers are non-solid or part-solid nodules. In comparison with other screening programs, this program included the high risk and the non-high risk group. The selection of screening population is very important, in other words, the high risk criteria are essential. Both age and smoking history are always the major high risk factors for lung cancer. The high risk criteria of major screening programs are listed in Table 1. In this retrospective study by Yi et al. (7), there were no defined criteria for high risk population based on their national characteristics; instead, they classified the population into high-risk and non-high risk using NLST (≥30 pack-years of smoking and ≥55 years of age; the upper age limit of the NLST was not considered in our study) and European criteria (≥20 pack-years of smoking and ≥50 years of age). They found LDCT is helpful for early detection of lung cancer in non-high risk group. But the difference in detection rate of lung cancer between non-high risk and high risk group was not performed, which would help to draw the criteria suitable for the South Korea. Although age and smoking history are very important high risk factors, but the incidence of lung cancer in young people without smoking history increased. In Asian, except for South Korea, Japan was the first to perform the lung cancer screening program, all the people between 40-80 years old were recruited, while the smoking history were not considered. The detection rate of lung cancer was 0.9% (14/1,611) at the baseline screening (8). Besides smoking history, environmental population may be another important high risk factor for lung cancer, especially the increasing of PM2.5 in air. Therefore, the high risk criteria need to be defined according to different nations. The study evaluated the high-risk and non-high risk group, which indicates a research direction to define the high risk criteria. By assessing the lung cancer detection rate in different age distributions, smoking history, and other high risk factors, determinate high risk criteria may be drawn suitable for different countries. In China, air pollution is threatening the public health; the morbidity of lung cancer is increasing, even in 35 years old people without smoking history. Therefore, the high risk criteria may be expanded in China. A lung cancer screening program is performing in Shanghai, which would try to make the high risk criteria suitable for the Chinese. On the other hand, if the criteria are expanded, the over-diagnosis would be increased and the long-term benefit of screening should be investigated. Although there are several screening program in Europe, there are no lung cancer screening recommendation in Europe. Therefore, the European Society of Radiology (ESR)/European Respiratory Society (ERS) issued the white paper on lung cancer screening (9). In the near future, the Asia should make a recommendation or guideline on the lung cancer screening.
Full table
How to evaluate CT imaging is another important issue for the screening. The positive results are related to the management of participants. The detailed positive definition of NLST, I-ELCAP, NELSON and ITALUNG are listed in Table 2 (3-6). From Table 2, we can find most of the positive results are defined based on the nodule size and density; and most of the programs classified the nodules into positive and negative ones. Only the NELSON trial used volume as the positive threshold and classified the nodules into positive, indeterminate and negative. I-ELCAP and ITALUNG defined the different size threshold according to the density, which is consistent with the different management for solid and subsolid nodules. NLST defined non-calcified nodules 4 mm or bigger in longest diameter as the positive. Those less than 4 mm were regarded as the negative. A recent study on the growth of pure ground glass nodules (GGNs) 5 mm or smaller, recommended that these nodules should perform follow-up CT 3.5 years later to look for the presence of solid component (10). However, according to the Fleischner society (11), these solitary pure GGNs do not recommend for the follow up CT scanning. In Japanese screening programs, any size and any density nodules were considered as positive, which is similar to the study by Yi et al. (7). The positive rate of this study was 46.8% (2,700/5,771), which was higher than that of any other screening program due to the expanded positive definition. The size threshold or positive definition is not consistent, which need further big data to be investigated.

Full table
Except for the high risk criteria and positive definition, another advantage of the study by Yi et al. (7) is the detailed classification of nodule according to the density. The nodules were classified into solid, part-solid, non-solid and calcified ones. The frequency of part-solid and non-solid nodules was 5.6% (1/18) and 22.2% (4/18) in high-risk group according to the NLST criteria, respectively. In contrast, other screening programs mainly evaluated the subsolid nodules in total. The evaluation of different pathological type distribution in high and non-high risk group is another advantage. Meantime, there is a small error of the study, on page 2337 “according to their greatest dimension: (<5 mm, 5-10 mm and >0 mm in diameter)” should be changed into “according to their greatest dimension: (<5 mm, 5-10 mm and >10 mm in diameter)”.
We would like to congratulate Dr. Yi et al. for their work. They evaluated the non-high risk and high risk groups and had detailed nodule classifications and pathological types, which were different from those of the America and European screening programs. The Asian may issue a guidelines or recommendation on lung cancer screening in the near future.
Acknowledgements
Funding: This work was supported by the National Natural Science Foundation of China [81370035 to L Fan, 81230030 to SY Liu]; and major projects of Biomedicine Department of Shanghai Science and Technology Commission [13411950100 to SY Liu].
Footnote
Provenance: This is a Guest Editorial commissioned by the Guest-Editor Lihua Chen [Department of Radiology, Taihu Hospital (PLA 101 Hospital), Wuxi, Jiangsu, China].
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Goldstraw P, Crowley J, Chansky K, et al. The IASLC Lung Cancer Staging Project: proposals for the revision of the TNM stage groupings in the forthcoming (seventh) edition of the TNM Classification of malignant tumours. J Thorac Oncol 2007;2:706-14. [PubMed]
- Sone S, Takashima S, Li F, et al. Mass screening for lung cancer with mobile spiral computed tomography scanner. Lancet 1998;351:1242-5. [PubMed]
- Aberle DR, DeMello S, Berg CD, et al. Results of the two incidence screenings in the National Lung Screening Trial. N Engl J Med 2013;369:920-31. [PubMed]
- van Klaveren RJ, Oudkerk M, Prokop M, et al. Management of lung nodules detected by volume CT scanning. N Engl J Med 2009;361:2221-9. [PubMed]
- International Early Lung Cancer Action Program Investigators. Survival of patients with stage I lung cancer detected on CT screening. N Engl J Med 2006;355:1763-71. [PubMed]
- Lopes Pegna A, Picozzi G, Falaschi F, et al. Four-year results of low-dose CT screening and nodule management in the ITALUNG trial. J Thorac Oncol 2013;8:866-75. [PubMed]
- Yi CA, Lee KS, Shin MH, et al. Low-dose CT screening in an Asian population with diverse risk for lung cancer: A retrospective cohort study. Eur Radiol 2015;25:2335-45. [PubMed]
- Sobue T, Moriyama N, Kaneko M, et al. Screening for lung cancer with low-dose helical computed tomography: anti-lung cancer association project. J Clin Oncol 2002;20:911-20. [PubMed]
- Kauczor HU, Bonomo L, Gaga M, et al. ESR/ERS white paper on lung cancer screening. Eur Respir J 2015;46:28-39. [PubMed]
- Kakinuma R, Muramatsu Y, Kusumoto M, et al. Solitary Pure Ground-Glass Nodules 5 mm or Smaller: Frequency of Growth. Radiology 2015;276:873-82. [PubMed]
- Naidich DP, Bankier AA, MacMahon H, et al. Recommendations for the management of subsolid pulmonary nodules detected at CT: a statement from the Fleischner Society. Radiology 2013;266:304-17. [PubMed]


