Chronic Klebsiella pneumonia: a rare manifestation of Klebsiella pneumonia
Introduction
Chronic pneumonia can be caused by either infectious or non-infectious diseases. Among infectious diseases, Mycobacterium tuberculosis, Burkholderia pseudomallei, Nocardia species, and Aspergillus species are the most likely pathogens. Although common pathogens that cause community-acquired pneumonia, such as Streptococcus pneumoniae, Klebsiella pneumoniae, Haemophilus influenzae, and Staphylococcus aureus, can develop a necrotic process and result in a prolonged clinical course, the process usually follows the course of acute pneumonia and turns rapidly progressive, with patients tending to develop acute respiratory distress (1). Herein, we present two cases of chronic Klebsiella pneumonia, a rare manifestation of Klebsiella pneumonia presenting with a chronic, indolent course.
Case reports
Case 1
In March 2014, a 59-year-old male with poorly controlled type 2 diabetes mellitus was referred to our hospital with a 2-month history of low-grade fever, productive cough, and right-sided pleuritic chest pain. On the first day of symptoms, he had visited a general practitioner. The chest radiograph was unremarkable and he was diagnosed with myalgia. One month prior to presentation, he occasionally began coughing up blood-streaked sputum. He went to a private hospital and was then referred to our hospital. During this period, he was diagnosed with an upper respiratory tract infection and was prescribed a 5-day course of amoxicillin/clavulanate by his general practitioner, but failed to show any improvement. He had a 40 pack year history of smoking and was a social alcohol drinker. He also noted weight loss of 5 kg during this time.
On physical examination, the patient was in no distress. His vital signs were as follows: body temperature, 37.1 °C; blood pressure, 130/70 mmHg; pulse, 106 beats/min; respiratory rate, 16 breaths/min; and oxygen saturation while breathing room air, 98%. Respiratory examination did not reveal any abnormality. Other physical findings were unremarkable. Complete blood count showed a hematocrit of 35%, white blood cell count of 12,350 cells/mm3 with 63% neutrophils, 28% lymphocytes, and 6% monocytes, and a platelet count of 391,000 cells/mm3. Blood sugar was 530 mg/dL. Other blood chemistries were within normal limits.
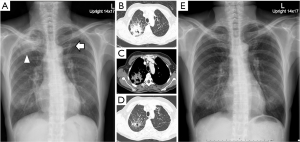
The chest radiograph at presentation revealed patchy opacity with cavitary lesion at the superior segment of the right lower lobe (Figure 1A). A chest computed tomography (CT) scan showed heterogenous subpleural consolidation with air bronchogram and cavitation at the superior segment of the right lower lobe (Figure 1B,C).

A sputum Gram stain demonstrated mixed organisms and sputum culture was contaminated with oropharyngeal flora. In addition, a sputum acid-fast bacillus (AFB) stain was negative. Radial endobronchial ultrasound (R-EBUS) and fluoroscopic-guided flexible bronchoscopy (FB) was performed. Bronchoalveolar lavage fluid (BALF) showed numerous polymorphonuclear cells and gram-negative bacilli by Gram stain. Aerobic culture grew K. pneumoniae. AFB stain, PCR testing, and culture for tuberculosis were negative. Histopathological examination of transbronchial lung biopsy revealed only acute inflammation without evidence of malignancy or granuloma.
Following an extensive literature review, chronic Klebsiella pneumonia was suspected. The patient was then prescribed intravenous ceftriaxone 1 g every 12 h for 2 weeks followed by a 6-week course of oral amoxicillin/clavulanate (1 g every 12 h). The symptoms improved within the first week of treatment. Follow-up chest X-rays demonstrated continued improvement over time. CT of the chest was performed 3 months after treatment and revealed nearly complete resolution of the pre-existing area of consolidation, leaving a small thin-walled cavity and some residual fibrosis (Figure 1D,E).
Case 2
A 55-year-old female presented to our hospital in September 2014 with a 2-month history of productive cough and 3-week of low-grade fever and right-sided pleuritic chest pain. She had a history of pulmonary tuberculosis that had been treated 20 years before, leaving a fibrotic scar at the left upper lobe in the chest X-ray, which was last taken three months prior to this presentation. She had no co-morbidities and denied a history of smoking, drinking, or any use of illicit drugs. During this period, she had not received any antibiotics.
On presentation, the patient was not tachypneic or dyspneic. Vital signs were body temperature of 37.5 °C, blood pressure of 100/70 mmHg, pulse of 105 beats/min, respiratory rate of 20 breaths/min, and oxygen saturation of 98% on room air. On auscultation, bronchial breath sound and increased vocal resonance were detected at the right upper lobe. Other physical examinations were unremarkable. Complete blood count showed leukocytosis of 13,990 cells/mm3 (77% neutrophils, 16% lymphocytes, 6% monocytes). Other blood chemistry tests were all within normal ranges.
Compared with the last chest X-ray taken three months previously, a new X-ray revealed a new consolidation at the apical segment of the right upper lobe, while the lesion at the left upper lobe remained unchanged (Figure 2A). A chest CT scan showed a large cavitary consolidation at the apical segment of the right upper lobe (Figure 2B,C). A small focal consolidation was also detected at the inferior lingular segment.
Sputum examination demonstrated few gram-positive cocci and gram-negative bacilli, and negative AFB stain. Empiric treatment for melioidosis with ceftazidime 2 g every 8 h was initiated. R-EBUS and fluoroscopic-guided FB was performed over the next three days. BALF showed numerous polymorphonuclear cells with no organisms detected by Gram and AFB stain. Sputum aerobic culture grew K. pneumoniae, while there was no organism growth in BALF culture. Histopathology was negative for malignancy and granuloma.
Chronic Klebsiella pneumonia was diagnosed and ceftazidime was changed to ceftriaxone 1 g every 12 h for 2 weeks. After that, a 6-week course of amoxicillin-clavulanate (1 g every 12 h) was substituted. Continuous improvement of the lesion was found on follow-up chest X-rays. A chest CT scan, performed 6 weeks after initiation of treatment, showed partial regression of the previous cavitary consolidation with a residual thin-walled cavity and fibrotic changes (Figure 2D,E). Previous focal consolidation at the inferior lingular segment was also improved.
Discussion
K. pneumoniae (previously known as Friedländer’s bacillus) can present as two forms of community-acquired pneumonia. The acute form, a well-known disease entity, usually develops quickly and lasts less than two weeks. A minority of patients with this form may develop necrotizing pneumonia and run a protracted clinical course (1-3). In contrast, the chronic form is not well recognized and has rarely been reported (3,4).
As in our cases, chronic productive cough is a frequent presenting symptom and hemoptysis may be noted in some cases (3,4). Although it is an infectious disease, fever may not be detected in some cases, requiring a broad differential diagnosis, including malignancy and connective tissue disease.
A chest X-ray of chronic Klebsiella pneumonia usually demonstrates as consolidation located mainly at the apical and posterior segments of the right upper lobe and the superior segment of the right lower lobe (3,4). Due to the zonal preferences in conjunction with a chronic indolent course, it may be mistaken for pulmonary tuberculosis (4). As in our cases, a CT scan depicts the cavitary lesion and multiple areas of low attenuation within the consolidation, indicating a necrotic process. This radiographic finding resembles necrotizing pneumonia but the two diseases are different in clinical course (1,4-6).
Non-invasive diagnostic methods for chronic Klebsiella pneumonia are problematic. Sputum Gram stain and aerobic culture are usually contaminated with oropharyngeal flora. Even when K. pneumoniae is isolated from the sputum culture, whether it is a true pathogen remains a question, as it can be found as a saprophyte in the airway. Thus, it is inevitable to perform FB when sputum examination cannot lead to an alternative definite diagnosis such as tuberculosis, nocardiosis, or malignancy. FB with a guidance technique toward the lesion such as R-EBUS and fluoroscopy should be used in order to avoid inappropriate samplings. Definite diagnosis of chronic Klebsiella pneumonia can be made when the organism is isolated from BALF, without having to identify other potential causes from FB specimens. In case 2, the patient had received intravenous antibiotic before FB, resulting in negative microbial growth. The diagnosis of chronic Klebsiella pneumonia was concluded by identification of the organism in sputum culture, together with negative results for other microbial agents as well as tumor cells in BALF, and the patient responded well to antibiotic therapy.
The optimal duration of antibiotic therapy is unclear, but usually corresponds to the treatment of necrotizing pneumonia (4,5,7,8), typically 4 weeks to 4 months depending on clinical and radiologic responses. Symptoms generally improve within one week after initiation of treatment, while the radiographic finding shows gradual improvement over time and demonstrates almost complete resolution of the lesion with some residual fibrosis (3,4).
In conclusion, we report on two cases of chronic Klebsiella pneumonia. Although rare, physicians should keep this form of Klebsiella pneumonia in mind because it can mimic other chronic pulmonary infections and malignancies. When a definite diagnosis is not reached by routine sputum examination, FB may be necessary to obtain the samples for examination. The diagnosis of chronic Klebsiella pneumonia is established by positive microbiological culture of BALF, without having the other potential causes discovered from FB sampling specimens.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Tsai YF, Ku YH. Necrotizing pneumonia: a rare complication of pneumonia requiring special consideration. Curr Opin Pulm Med 2012;18:246-52. [PubMed]
- Solomon S. Chronic Friedländer infections of the lungs. JAMA 1940;115:1527-36.
- Erasmus LD. Friedländer bacillus infection in the lung: With special reference to classification and pathogenesis. Q J Med 1956;25:507-21. [PubMed]
- Sinha R, Panjabi C, Varma M, et al. Chronic Klebsiella pneumonia in an immunocompetent host. J Assoc Physicians India 2003;51:306-8. [PubMed]
- Seo H, Cha SI, Shin KM, et al. Focal necrotizing pneumonia is a distinct entity from lung abscess. Respirology 2013;18:1095-100. [PubMed]
- Moon WK, Im JG, Yeon KM, et al. Complications of Klebsiella pneumonia: CT evaluation. J Comput Assist Tomogr 1995;19:176-81. [PubMed]
- Sawicki GS, Lu FL, Valim C, et al. Necrotising pneumonia is an increasingly detected complication of pneumonia in children. Eur Respir J 2008;31:1285-91. [PubMed]
- Krenke K, Sanocki M, Urbankowska E, et al. Necrotizing Pneumonia and Its Complications in Children. Adv Exp Med Biol 2015;857:9-17. [PubMed]


