The multidrug-resistant tuberculosis threat: old problems and new solutions
With more than 1 million deaths and 9 million estimated incident cases in 2013 tuberculosis represents one of the top clinical and public health priorities worldwide (1).
The World Health Organization (WHO) public health strategy known as DOTS, launched in the 90s’ and then scaled-up globally, has contributed to revert the TB incidence trend and the disease-related mortality, if the current estimates are compared with those of the pre-DOTS era. However, TB control and eventually elimination (i.e., defined as less than one case per million population) are challenged by the cursed duet (the TB/HIV co-infection) and by multidrug-resistant tuberculosis (MDR-TB, tuberculosis caused by Mycobacterium tuberculosis strains resistant to at least two of the most powerful first-line anti-TB drugs, isoniazid and rifampicin).
The WHO estimated that 13% of the 9 million TB cases (1.1 million people) were HIV-infected, particularly in the WHO African Region, where 4 out of 5 of these cases are estimated to occur in 2013. The qualitative and quantitative immune-deficiency related to the HIV replication, not controlled by appropriate anti-retroviral therapy, and significantly increases the probability of acquiring TB disease given infection. In these individuals the clinical course of pulmonary and extra-pulmonary TB is more severe and associated with higher probability of death.
Furthermore, MDR-TB (which largely is a man-made phenomenon) has become a serious problem in those geographical areas where national health-care systems face economic, logistic, and organizational weaknesses (e.g., in Africa, Asia, and former Soviet Union countries) (2,3). The 2014 WHO Global Report estimated that 3.5% and 20.5% of new and previously treated TB cases had MDR-TB, with a total estimated incidence of 480,000 cases in 2013. Unfortunately, only 136,000 of them were detected, so that transmission of drug resistant strains is rampant among close contacts, treatment with inappropriate anti-TB regimens further increasing the probability of developing additional antibiotic resistances (1).
Aim of the present contribution is to describe the global MDR-TB context, focusing on the problems related to its prevention, diagnosis and treatment. In particular the new and re-proposed drugs are described into details. The review of the literature, although non-systematic, has been done to capture the recent key articles available.
Managing MDR: lights and shadows
The best way to prevent MDR-TB is to diagnose and treat correctly the cases whose strains of Mycobacterium tuberculosis are susceptible to first-line anti-TB drugs. A recent European study demonstrated that clinical and public health mismanagement of MDR-TB cases occurred also in highly specialized reference centers of the European Union. Management pitfalls were detected mainly in infection control activities (implementation of administrative and environmental measures), as well as inappropriate use of personal protective equipment), prescription of anti-TB drugs (particularly dosage and duration of second- and third-line antibiotics) and anti-retrovirals, as well as contact tracing of close contacts (4,5).
In low- and middle-income countries the situation is even worse due to the sub-optimal laboratory network (not making systematic culture, drug susceptibility testing and rapid molecular testing with Xpert MTB/RIF possible) and second line anti-TB drugs (6). Treatment of MDR-TB cases is long, expensive and complicated by the frequent occurrence of adverse events (AE), calling for changes in the prescribed regimen and need for ancillary drugs. All this may compromise the patients’ adherence to treatment.
In 2013, 97,000 patients were administered an appropriate treatment for MDR-TB. Although this represents a low proportion if compared with the estimated prevalent cases worldwide, the positive news is that the number of treated cases is today higher than those treated in 2009 (1).
Unfortunately more and more severe cases of MDR-TB, known as extensively-drug resistant tuberculosis (XDR-TB) (i.e., TB caused by MDR Mycobacterium tuberculosis strains resistant to any fluoroquinolones and to one of the second-line injectable drug amikacin, kanamycin, and capreomycin) have been described. The XDR-TB definition was considered to have a clinical and operational value (7) because of its worse clinical appearance coupled with worse prognosis. More recently, the new acronym totally drug-resistant tuberculosis (TDR-TB) was proposed for the top severe cases, but this definition was not endorsed by WHO because the drug-susceptibility testing for third-line drugs is not reliable and a complete characterization of the anti-TB drugs which should be ex vivo tested to ascertain their susceptibility is missing (8). The WHO estimated that the proportion of MDR-TB with an XDR-TB form should be 9% (1).
A systematic review and an individual patient data meta-analysis carried out a few years ago collected the most relevant MDR-TB cohorts described in the scientific literature (32 datasets including 9,153 patients) from 23 countries belonging to all WHO Regions, in order to assess the clinical outcomes and the covariates associated with the best success rates (9). Fifty-four percent, equivalent to 4,934 patients, achieved treatment success (cure or treatment completion), whereas 23% defaulted, 15% died, and 8% failed or relapsed. Individuals who defaulted or died were older, HIV-infected, previously exposed to anti-TB drugs, and with a more severe disease.
The administration of ethionamide/prothionamide, as well as ofloxacin or late-generation quinolones, pyrazinamide, and cycloserine was associated with a higher probability of treatment success, compared to failure, relapse and death. Unfortunately, the prescription of group 5 drugs (amoxicillin-clavulanate, clofazimine, clarithromycin, and thiacetazone), whose efficacy is unknown for Mycobacterium tuberculosis, did not demonstrate higher effectiveness in a subset of patients belonging to the pooled cohort. The treatment success rate was higher in those treated with at least four and three drugs during the intensive and the continuation phase, respectively. The effective duration of the intensive phase should be from 7 to 8.4 months, whereas the effective duration of the therapy should be 24.6-27.5 months.
The same authors proved how additional resistances to a basic MDR-TB pattern could significantly influence the treatment success rate: it was 64% for patients infected by mycobacterial strains with resistances only to isoniazid and rifampicin, whereas decreased in cases with further resistance to second-line injectable drugs (56%), fluoroquinolones (48%), or to second-line injectable drugs and fluoroquinolones (40%). The latter group (XDR-TB) could be successfully treated if exposed to at least six and four anti-TB drugs during the intensive and the continuation phase, respectively. Moreover, the duration is also important, as an intensive phase of 6.6-9 months and a total duration of 20.1-25 months proved to be successful. Additional resistances to the XDR pattern (for instance, group four drugs) were associated with higher rates of death and treatment failure (10,11).
Two new drugs after 40 years of neglect
The current WHO guidelines for MDR-TB (12), based on the above-mentioned systematic review and an individual patient data meta-analysis, support the best possible use of old, toxic, and poorly effective drugs. When facing XDR- or TDR-TB cases clinicians have difficulties in identifying a sufficient number of anti-TB drugs to design an effective regimen. This was a situation pushing them back to a pre-antibiotic era (13).
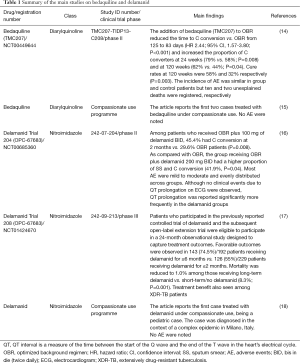
In this context, the need of new anti-TB drugs is obvious. After more than 40 years without new TB drugs, two new drugs (bedaquiline and delamanid) have been recently approved by the Food and Drug Administration (FDA) and the European Medicine Agency (EMA) for the American and European market, respectively (Table 1).
Full table
Bedaquiline (TMC207), a diarylquinoline, was the first drug released in the market after a clinical development process proving its efficacy, safety, and tolerability (19). In particular, the clinical trials confirmed its ability to inhibit the Mycobacterium tuberculosis ATP synthase and, consequently, its replication. The initial bacteriostatic action is followed by a bactericidal effect after 5-7 days. Phase II studies demonstrated positive pharmacological interactions with the other first- and second-line anti-TB drugs. The proportion of culture converters was high and the probability of developing resistance to bedaquiline was low. However, experts highlighted that its future efficacy is strictly related to the prescription of an appropriate backbone regimen as per WHO guidelines (proper drug selection, duration and dosages, based on full drug-susceptibility testing) (14,20-22). The drug has been initially available under compassionate use, and proved to be safe (15).
Delamanid (OPC-67683), a nitro-dihydro-imidazooxazole, is able to inhibit the synthesis of the mycolic acid, removing a crucial component of the bacterial wall. Its bactericidal activity has been compared to that of isoniazid, acting in both the intra- and extra-cellular environment (23). One study showed that delamanid-containing regimens could significantly decrease the mortality after 6 months of treatment. The delamanid-related treatment success was 74.2% in a large cohort of MDR-TB patients after 6 months of treatment; furthermore, its efficacy was also confirmed in the XDR-TB group (treatment success: 61.4%) (16,17,24). The first case treated under compassionate use was a pediatric case, who tolerated the treatment well (18).
Knowing more on re-proposed drugs
In parallel with the studies on bedaquiline and delamanid, other observational and experimental trials were conducted to assess efficacy, safety, and tolerability of other antibiotics licensed to treat different bacterial infections. In particular, linezolid (used to treat methicillin-resistant Staphylococcus aureus infections) and glycopeptides (vancomycin and teicoplanin) are used off-label to treat MDR- and XDR-TB patients when the therapeutic alternatives do not allow designing an effective regimen (25-29). A systematic review and individual patient data meta-analysis collected all the global observational experience on linezolid to treat drug-resistant Mycobacterium tuberculosis strains and pooled individual data to provide a clear picture on its efficacy, safety, and tolerability (25). The linezolid-containing regimens prescribed to 121 MDR-TB patients contributed to achieve high sputum smear (SS) and culture conversion rates (92.5% and 93.5%, respectively). The pooled success rate was 81.8%. If the efficacy was similar comparing outcome indicators in individuals treated with a daily dosage >600 or ≤600 mg, the safety and tolerability profiles were significantly better in those treated with a lower daily linezolid dosage. The most relevant AE involved the blood count (i.e., anemia and thrombocytopenia), the peripheral nervous system, the optic nerve, and the gastro-intestinal apparatus. Those findings confirmed the results of the largest observational, multi-country cohort which underscored the potentiality of this drug (26). The validity of the retrospective observational design was confirmed by the first experimental study which enrolled 41 XDR-TB patients (27,28). The majority of them (87%) achieved sputum culture conversion after 6 months of linezolid exposure. However, potentially linezolid-related AE occurred in 82% of cases, leading to its permanent discontinuation in three individuals. All the XDR-TB cases were treated with 600 mg once daily. A sub-group of individuals treated with 300 mg per day proportionally experienced less AE. The assessment of the blood concentration of linezolid [the so called Therapeutic Drug Monitoring (TDM)] is able to reduce the side effects related to highest concentration of the drug, while maintaining adequate concentration and achieving economic savings, given linezolid is very expensive (30).
Another interesting class of antibiotics, used off-label in difficult-to-treat cases is represented by the carbapenems supported by a β-lactamase inhibitor. Meropenem showed interesting preliminary results in the only study published as of today. This observational, retrospective study addressed the issues related to meropenem efficacy and safety; it was administered with linezolid to 37 cases in Italian and Dutch centers at a daily dosage of 3 g. Although patients treated with meropenem had a more severe disease, the proportion of SS and culture conversion was lower in individuals exposed to a linezolid-containing regimen only in comparison with those treated with meropenem. One patient only discontinued meropenem because of liver toxicity (31). Very recently our group published the first report on the use of ertapenem at the dose of 1 g daily during the ambulatory phase of treatment. The drug was well tolerated (32).
The tolerability and pharmacokinetic profile of co-trimoxazole, frequently prescribed for different bacterial, fungal, and parasitic infections, was proven in a study enrolling ten patients. The Authors concluded that the drug was effective and safe, a single patient reporting gastro-intestinal symptoms (33).
The role of surgery
Surgical intervention was perceived as an old-fashioned therapeutic option although it has been frequently used in some geographical areas (e.g., in former Soviet Union countries) as an alternative or an adjunctive therapy for TB patients. However, more, recently surgery has been re-discovered to manage difficult-to-treat MDR-/XDR-TB patients (34-36). A systematic review and meta-analysis showed that the success rate in those surgically treated is higher [with odds ratio (OR) >2], particularly in the XDR-TB patients (OR of treatment success: 4.55) (34). The WHO Regional Office for Europe issued a document, supported by experts, where observational scientific evidence proved the efficacy of surgery in localized forms of MDR- and XDR-TB, particularly after the patient’s exposure to 4-6 active anti-TB drugs. However, the expert panel recommended several conditions allowing surgical interventions, which include good pulmonary reserve, localized forms, low surgical risk, and proven previous failure with polichemotherapy. The interventions should be performed only in specialized centers with an appropriate infection control system in place (35,36).
Conclusions
The MDR-TB phenomenon has been defined a ‘back to the future’; it need to be adequately addressed. The WHO’s Stop TB Strategy, launched in 2006, underlined for the first time the risk posed by the MDR-TB and TB/HIV co-infection pandemics to the global TB control and provided strategic answers to tackle them. The new End TB Strategy, supporting the vision of TB elimination, further elaborates on how to prevent its occurrence while managing the cases already existing.
The availability of two new drugs and of several re-proposed ones, gives us a real opportunity. Day after day we understand better how to use these new therapeutic options both when added to an optimized background regimen (OBR) or when included in new regimens.
It is important to underline that an essential condition to protect the new drug is to ensure their rational use within stronger public health systems supporting patient’s adherence and preventing default and failure (37,38). Without governments’ commitment and adequate funding we risk losing in a few years the results of 40 years of efforts.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- World Health Organization. Global tuberculosis report 2014. Geneva, Switzerland, 2014. Available online: http://www.who.int/tb/publications/global_report/en/
- Sotgiu G, Mauch V, Migliori GB, et al. Evidence-based, agreed-upon health priorities to remedy the tuberculosis patient’s economic disaster. Eur Respir J 2014;43:1563-6. [PubMed]
- Skrahina A, Hurevich H, Zalutskaya A, et al. Alarming levels of drug-resistant tuberculosis in Belarus: results of a survey in Minsk. Eur Respir J 2012;39:1425-31. [PubMed]
- Migliori GB, Sotgiu G, D'Ambrosio L, et al. TB and MDR/XDR-TB in European Union and European Economic Area countries: managed or mismanaged? Eur Respir J 2012;39:619-25. [PubMed]
- Sotgiu G, D'Ambrosio L, Centis R, et al. TB and M/XDR-TB infection control in European TB reference centres: the Achilles' heel? Eur Respir J 2011;38:1221-3. [PubMed]
- Weyer K, Mirzayev F, Migliori GB, et al. Rapid molecular TB diagnosis: evidence, policy making and global implementation of Xpert MTB/RIF. Eur Respir J 2013;42:252-71. [PubMed]
- Migliori GB, Besozzi G, Girardi E, et al. Clinical and operational value of the extensively drug-resistant tuberculosis definition. Eur Respir J 2007;30:623-6. [PubMed]
- Migliori GB, Centis R, D'Ambrosio L, et al. Totally drug-resistant and extremely drug-resistant tuberculosis: the same disease? Clin Infect Dis 2012;54:1379-80. [PubMed]
- Ahuja SD, Ashkin D, Avendano M, et al. Multidrug resistant pulmonary tuberculosis treatment regimens and patient outcomes: an individual patient data meta-analysis of 9,153 patients. PLoS Med 2012;9:e1001300. [PubMed]
- Falzon D, Gandhi N, Migliori GB, et al. Resistance to fluoroquinolones and second-line injectable drugs: impact on multidrug-resistant TB outcomes. Eur Respir J 2013;42:156-68. [PubMed]
- Migliori GB, Sotgiu G, Gandhi NR, et al. Drug resistance beyond extensively drug-resistant tuberculosis: individual patient data meta-analysis. Eur Respir J 2013;42:169-79. [PubMed]
- Falzon D, Jaramillo E, Schünemann HJ, et al. WHO guidelines for the programmatic management of drug-resistant tuberculosis: 2011 update. Eur Respir J 2011;38:516-28. [PubMed]
- Migliori GB, Sotgiu G, Lange C, et al. Extensively drug-resistant tuberculosis: back to the future. Eur Respir J 2010;36:475-7. [PubMed]
- Diacon AH, Pym A, Grobusch MP, et al. Multidrug-resistant tuberculosis and culture conversion with bedaquiline. N Engl J Med 2014;371:723-32. [PubMed]
- Tiberi S, De Lorenzo S, Centis R, et al. Bedaquiline in MDR/XDR-TB cases: first experience on compassionate use. Eur Respir J 2014;43:289-92. [PubMed]
- Gler MT, Skripconoka V, Sanchez-Garavito E, et al. Delamanid for multidrug-resistant pulmonary tuberculosis. N Engl J Med 2012;366:2151-60. [PubMed]
- Skripconoka V, Danilovits M, Pehme L, et al. Delamanid improves outcomes and reduces mortality in multidrug-resistant tuberculosis. Eur Respir J 2013;41:1393-400. [PubMed]
- Esposito S, D'Ambrosio L, Tadolini M, et al. ERS/WHO Tuberculosis Consilium assistance with extensively drug-resistant tuberculosis management in a child: case study of compassionate delamanid use. Eur Respir J 2014;44:811-5. [PubMed]
- Chahine EB, Karaoui LR, Mansour H. Bedaquiline: a novel diarylquinoline for multidrug-resistant tuberculosis. Ann Pharmacother 2014;48:107-15. [PubMed]
- Diacon AH, Donald PR, Pym A, et al. Randomized pilot trial of eight weeks of bedaquiline (TMC207) treatment for multidrug-resistant tuberculosis: long-term outcome, tolerability, and effect on emergence of drug resistance. Antimicrob Agents Chemother 2012;56:3271-6. [PubMed]
- Diacon AH, Dawson R, Von Groote-Bidlingmaier F, et al. Randomized dose-ranging study of the 14-day early bactericidal activity of bedaquiline (TMC207) in patients with sputum microscopy smear-positive pulmonary tuberculosis. Antimicrob Agents Chemother 2013;57:2199-203. [PubMed]
- World Health Organization. The use of bedaquiline in the treatment of multidrug-resistant tuberculosis Interim policy guidance. Geneva, Switzerland, 2013. Available online: http://apps.who.int/iris/bitstream/10665/84879/1/9789241505482_eng.pdf?ua=1&ua=1
- Matsumoto M, Hashizume H, Tomishige T, et al. OPC-67683, a nitro-dihydro-imidazooxazole derivative with promising action against tuberculosis in vitro and in mice. PLoS Med 2006;3:e466. [PubMed]
- World Health Organization. The use of delamanid in the treatment of multidrug-resistant tuberculosis Interim policy guidance. Geneva, Switzerland, 2014. Available online: http://apps.who.int/iris/bitstream/10665/137334/1/WHO_HTM_TB_2014.23_eng.pdf?ua=1&ua=1&ua=1
- Sotgiu G, Centis R, D'Ambrosio L, et al. Efficacy, safety and tolerability of linezolid containing regimens in treating MDR-TB and XDR-TB: systematic review and meta-analysis. Eur Respir J 2012;40:1430-42. [PubMed]
- Migliori GB, Eker B, Richardson MD, et al. A retrospective TBNET assessment of linezolid safety, tolerability and efficacy in multidrug-resistant tuberculosis. Eur Respir J 2009;34:387-93. [PubMed]
- Lee M, Lee J, Carroll MW, et al. Linezolid for treatment of chronic extensively drug-resistant tuberculosis. N Engl J Med 2012;367:1508-18. [PubMed]
- Sotgiu G, Centis R, D'Ambrosio L, et al. Linezolid to treat extensively drug-resistant TB: retrospective data are confirmed by experimental evidence. Eur Respir J 2013;42:288-90. [PubMed]
- Sotgiu G, Pontali E, Migliori GB. Linezolid to treat MDR-/XDR-tuberculosis: available evidence and future scenarios. Eur Respir J 2015;45:25-9. [PubMed]
- Srivastava S, Peloquin CA, Sotgiu G, et al. Therapeutic drug management: is it the future of multidrug-resistant tuberculosis treatment? Eur Respir J 2013;42:1449-53. [PubMed]
- De Lorenzo S, Alffenaar JW, Sotgiu G, et al. Efficacy and safety of meropenem-clavulanate added to linezolid-containing regimens in the treatment of MDR-/XDR-TB. Eur Respir J 2013;41:1386-92. [PubMed]
- Tiberi Simon, D’Ambrosio Lia, De Lorenzo Saverio, et al. Ertapenem in the treatment of MDR-TB: first clinical experience. Eur Respir J 2015. In press.
- Alsaad N, van Altena R, Pranger AD, et al. Evaluation of co-trimoxazole in the treatment of multidrug-resistant tuberculosis. Eur Respir J 2013;42:504-12. [PubMed]
- Marrone MT, Venkataramanan V, Goodman M, et al. Surgical interventions for drug-resistant tuberculosis: a systematic review and meta-analysis. Int J Tuberc Lung Dis 2013;17:6-16. [PubMed]
- Dara M, Sotgiu G, Zaleskis R, et al. Untreatable tuberculosis: is surgery the answer? Eur Respir J 2015;45:577-82. [PubMed]
- WHO Regional Office for Europe. The role of surgery in the treatment of pulmonary TB and multidrug- and extensively drug-resistant TB. Copenhagen, Denmark, 2014. Available online: http://www.euro.who.int/__data/assets/pdf_file/0005/259691/The-role-of-surgery-in-the-treatment-of-pulmonary-TB-and-multidrug-and-extensively-drug-resistant-TB.pdf
- Migliori GB, Lienhardt C, Weyer K, et al. Ensuring rational introduction and responsible use of new TB tools: outcome of an ERS multisector consultation. Eur Respir J 2014;44:1412-7. [PubMed]
- Salfinger M, Migliori GB. Bedaquiline: finding the pores on the pot. Eur Respir J 2015;46:289-91. [PubMed]


